The outbreak of SARS-CoV-2 has been a huge obstacle for the normal functioning of nosocomial infection (NI) control programs including the active surveillance of multidrug-resistant microorganisms (MDRM). COVID-19 has increased healthcare pressure and precipitated changes in the routine workload both at hospital and microbiology lab level. Also, the current clinical guidelines on the management of patients with COVID-19 do not include recommendations on how to perform surveillance cultures or implement special control measures to avoid MDRM related NIs in these patients.
Despite all difficulties, the low prevalence of COVID-19 during the first stage of the pandemic in our region allowed us to continue with the active surveillance programs of MDRM in our center as we had been doing before the beginning of the pandemic.
The objective of this study is to analyze the impact COVID-19 has had on MDRM colonization in patients referred to the ICU setting from a tertiary center.
We present a descriptive and retrospective study that analyzed the isolation of MDRM within the surveillance program of antibiotic resistance of our hospital adult ICU from March 1, 2020 through May 31, 2020.
MDRM colonization studies were conducted periodically once a week at the patient’s admission to the ICU during his stay following the protocol of the Zero Resistance project.1 Axillary, pharyngeal, and rectal exudates were collected to rule out the presence of multi-drug resistant gram-negative bacilli followed by a nasal exudate to rule out the presence of linezolid-resistant Staphylococcus spp. and methicillin-resistant Staphylococcus aureus.
Patients who had tested positive for SARS-CoV-2 on the reverse transcriptase polymerase chain reaction (RT-PCR) test were included in the COVID-19 group. On the other hand, patients without a RT-PCR test or who had tested negative to this test were included in the non-COVID-19 group.
Data were expressed as mean ± interquartile range for the quantitative variables. The qualitative ones were expressed as frequencies and percentages. The Mann–Whitney U test was used for the quantitative variables while Fisher’s exact test was used for the categorical ones. The 95% confidence interval was used for the statistics.
The study was approved by the research committee and no informed consent form was required to handle the anonymous data because of the descriptive and observational nature of the study.
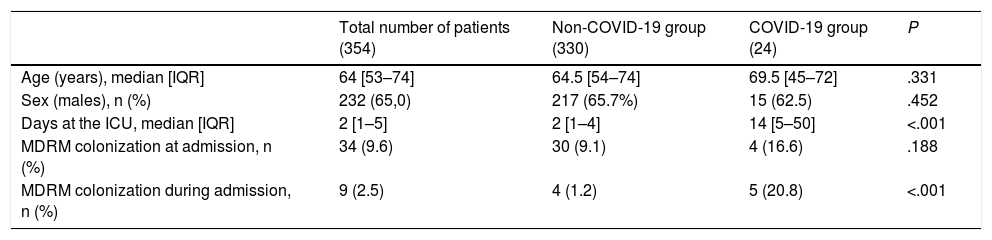
A total of 2139 specimens from 354 patients were analyzed. Of these, 361 came from 24 patients with a positive RT-PCR test for SARS-CoV-2 while 1778 specimens came from 330 patients without COVID-19. Table 1 shows the clinical and demographic characteristics of the patients.
Demographic data of patients with detection studies of multidrug-resistant microorganisms (MDRM) in the intensive care setting.
| Total number of patients (354) | Non-COVID-19 group (330) | COVID-19 group (24) | P | |
|---|---|---|---|---|
| Age (years), median [IQR] | 64 [53–74] | 64.5 [54–74] | 69.5 [45–72] | .331 |
| Sex (males), n (%) | 232 (65,0) | 217 (65.7%) | 15 (62.5) | .452 |
| Days at the ICU, median [IQR] | 2 [1–5] | 2 [1–4] | 14 [5–50] | <.001 |
| MDRM colonization at admission, n (%) | 34 (9.6) | 30 (9.1) | 4 (16.6) | .188 |
| MDRM colonization during admission, n (%) | 9 (2.5) | 4 (1.2) | 5 (20.8) | <.001 |
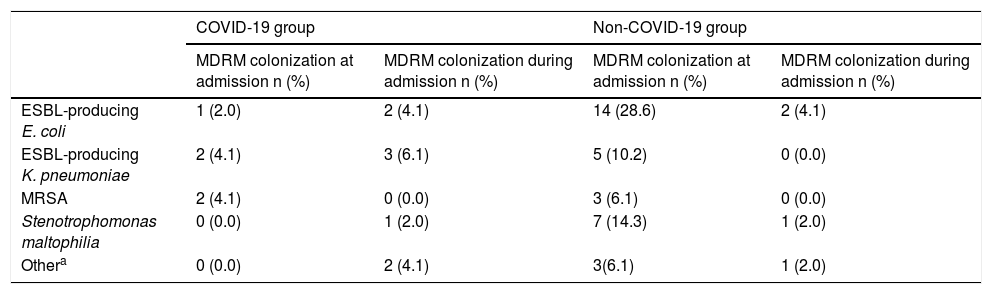
The MDRM most often found were extended spectrum beta-lactamase (ESBL)-producing enterobacteriaceae. Table 2 shows the MDRM isolated. Patients colonized with more than one species of MDRM were found in both groups. The positivity of the specimens analyzed (axillary, pharyngeal, nasal, and rectal exudates) was 2%, 2.4%, 0.9%, and 8.2%, respectively. The latter were the most cost-effective specimens for the detection of ESBL-producing enterobacteriaceae.
Multidrug-resistant microorganisms (MDRM) isolated from patients hospitalized at the intensive care unit (ICU) from March 1, 2020 through May 31, 2020.
| COVID-19 group | Non-COVID-19 group | |||
|---|---|---|---|---|
| MDRM colonization at admission n (%) | MDRM colonization during admission n (%) | MDRM colonization at admission n (%) | MDRM colonization during admission n (%) | |
| ESBL-producing E. coli | 1 (2.0) | 2 (4.1) | 14 (28.6) | 2 (4.1) |
| ESBL-producing K. pneumoniae | 2 (4.1) | 3 (6.1) | 5 (10.2) | 0 (0.0) |
| MRSA | 2 (4.1) | 0 (0.0) | 3 (6.1) | 0 (0.0) |
| Stenotrophomonas maltophilia | 0 (0.0) | 1 (2.0) | 7 (14.3) | 1 (2.0) |
| Othera | 0 (0.0) | 2 (4.1) | 3(6.1) | 1 (2.0) |
MRSA, methicillin-resistant Staphylococcus aureus.
This study analyzed patients with COVID-19 admitted to the ICU who have higher chances of MDRM colonization compared to patients admitted for other reasons (20.8% vs 1.2%, respectively). This can be due to the special characteristics of these hospitalized patients. One of these differences is longer ICU stays (14 days on average compared to just 2 days for non-COVID-19 patients). Former studies proved that extended hospital stays are one of the predisposing factors for MDRM colonization.2–5
The greater use of invasive techniques, common in this type of patients, is another factor associated with MDRM colonization.6 In our case, 68% of the patients with COVID-19 required mechanical ventilation within the first 24 h and 80% within the first 48 h.
Another aspect we should take into account is that most of these patients are on antibiotic treatment. In our case, 84% of the patients with COVID-19 received azithromycin during their ICU stay.
Added to all these factors there is a series of changes in how hospitals were organized, which may have led to worse detection control and management of MDRM.
In the first place, the tremendous workload sustained has precipitated the hiring of new personnel and the fact that part of the multidisciplinary teams dedicated to multi-drug resistance surveillance systems have had to assist patients with COVID-19. The increased pressure exerted on the healthcare system and the adoption of new safety measures like the use of personal protection equipment (PPE) can complicate the performance of certain techniques, among other, specimen extraction from patients with COVID-19 for the detection of MDRM.
Secondly, the saturated healthcare system has produced a lack of hospital and ICU beds that has complicated the implementation of isolation measures necessary in MDRM colonized patients or in case of other possible outbreaks.
Conversely, the hygiene measures implemented to prevent SARS-CoV-2 infections like frequent hand washing or use of hydroalcoholic gel are also valid to reduce the number of NIs and improve the surveillance of MDRM at the hospital setting.7
ConclusionsPatients with COVID-19 admitted to the UCI are more susceptible to MDRM colonization compared to other patients hospitalized in these units because of their special characteristics and the fact that most of them require long stays. However, given the limited number of patients recruited during this first pandemic wave, it would be interesting to conduct more studies including other areas of hospitalization.
Please cite this article as: Fernández P, Moreno L, Yagüe G, Andreu E, Jara R, Segovia M. Colonización por microorganismos multirresistentes en pacientes de UCI durante la pandemia de la COVID-19. Med Intensiva. 2021;45:313–315.