A comparison is made of the accuracy between severity models, based on different sepsis definitions (systemic inflammatory response syndrome (SIRS), predisposition, insult, response, organ dysfunction (PIRO), and sequential organ failure assessment (SOFA) concepts), in predicting outcomes among sepsis patients.
DesignA retrospective study was carried out.
SettingThe study was conducted in the Intensive Care Unit (ICU) of a university teaching hospital.
PatientsSeptic patients admitted to the ICU during 2007–2016.
Main variables of interestThe primary outcome was in-hospital mortality, with ICU mortality being the secondary outcome.
ResultsA total of 2152 septic patient were identified, with ICU and in-hospital mortality rates of 33.3% and 45.9%, respectively. The Moreno PIRO (AUC, 95%CI) (0.835; 0.818–0.852) showed the highest discriminating capacity, followed by SOFA (0.828; 0.811–0.846), qSOFA (0.792; 0.775–0.809), Rubulotta PIRO (0.708; 0.687–0.730), Howell PIRO (0.706; 0.685–0.728) and SIRS (0.578; 0.556–0.600). The AUC of the SOFA score was comparable to that of the Moreno PIRO (p=0.43), though the AUCs of both of these scores were significantly higher than those of the other scores (p<0.001 for all other comparisons). However, the SOFA score showed the best discriminating capacity in predicting ICU mortality (0.838; 0.820–0.855), followed by Moreno PIRO (0.804; 0.785–0.823) and qSOFA (0.787; 0.770–0.805). The accuracy of the qSOFA in predicting ICU mortality was comparable to that of the Moreno PIRO score (p=0.15).
ConclusionThe SOFA score and Moreno PIRO score showed the best accuracy in predicting in-hospital mortality among septic patients admitted to the ICU.
Comparar la precisión entre varios modelos de intensidad, basándose en diferentes definiciones de la sepsis (síndrome de respuesta inflamatoria sistémica [SIRS, por sus siglas en inglés], predisposición, infección, respuesta, disfunción orgánica [PIRO por sus siglas en inglés] y puntuación de la evaluación del fallo orgánico secuencial [SOFA por sus siglas en inglés]) para predecir los desenlaces en los pacientes con sepsis.
DiseñoEstudio retrospectivo.
ÁmbitoEl estudio se llevó a cabo en la unidad de cuidados intensivos (UCI) de un hospital universitario.
PacientesEnfermos con sepsis ingresados en la UCI durante 2007-2016.
Variables de interés principalesEl desenlace principal fue la mortalidad hospitalaria, mientras que la mortalidad en la UCI fue el desenlace secundario.
ResultadosSe identificó un total de 2.152 pacientes con sepsis, con unas tasas de mortalidad en la UCI e intrahospitalaria del 33,3 y del 45,9%, respectivamente. El modelo Moreno-PIRO (AUC, IC del 95%) (0,835; 0,818-0,852) fue el que presentó una mayor capacidad de discriminación, seguido del modelo SOFA (0,828; 0,811-0,846), modelo qSOFA (0,792; 0,775-0,809), modelo Rubulotta-PIRO (0,708; 0,687-0,730), modelo Howell-PIRO (0,706; 0,685-0,728) y modelo SIRS (0,578; 0,556-0,600). El AUC de la puntuación SOFA fue comparable al de Moreno-PIRO (p=0,43), si bien el AUC de ambas puntuaciones fue significativamente superior al de otras puntuaciones (p<0,001 para todas las demás comparaciones). Sin embargo, la puntuación SOFA es la que presenta la mayor capacidad de discriminación para predecir la mortalidad en la UCI (0,838; 0,820-0,855), seguida de Moreno-PIRO (0,804; 0,785-0,823) y qSOFA (0,787; 0,770-0,805). La precisión de la puntuación qSOFA en cuanto a la predicción de la mortalidad en la UCI fue comparable a la de la puntuación Moreno-PIRO (p=0,15).
Conclusión La puntuación SOFA y la puntuación Moreno-PIRO mostraron la mejor precisión en la predicción Mortalidad intrahospitalaria entre pacientes sépticos ingresados en la UCI.
Sepsis and septic shock are currently a leading problem among intensive care unit (ICU) patients worldwide.1–5 The ICU as well as in-hospital mortality owing to sepsis and septic shock have also been significantly higher than other critical illness conditions over the past few decades.1–5 Until now, there have been three sepsis definitions endorsed by international societies, according to update knowledge in sepsis pathogenesis and pathophysiology. The first sepsis definition (Sepsis-1) was established in 1992, and focused on sepsis as a syndrome of infection, with systemic inflammatory response syndrome (SIRS concept).6 The second definition of sepsis by International Sepsis Definitions in 2001 (Sepsis-2) was also based on the SIRS concept, but tried to revise and included a list of more signs and symptoms, more so than SIRS.7 Signs and symptoms of sepsis according to Sepsis-2 definition was also classified into four categories which were: Predisposition, Insult/Infection, Response, Organ dysfunction; this in turn introduced the PIRO concept as a staging system of sepsis.7 However, the severity scoring system of sepsis was not unified, and so some authors tried to develop an individual score to predict mortality, based on the PIRO concept for both general sepsis patients,8–14 and a more specific group such as; hospital acquired pneumonia.15,16 Unfortunately, the PIRO scores are not widely used nowadays owing to their complexity.
The sepsis definition was change again in 2016, by the Third International Consensus Definitions for Sepsis and Septic shock (Sepsis-3), the changed sepsis into an organ dysfunction syndrome, rather than SIRS, as the organ failure concept is better in mortality prediction.17 This definition reintroduces Sequential Organ Failure Assessment (SOFA)18 score into clinical use. The more simplified score or quick SOFA (qSOFA) was introduced for clinician alert for sepsis.17 The later score was validated by Seymour et al. and reported better accuracy of discrimination in term of mortality other than SIRS, especially in non-ICU encounter situations.19 The external validity was also conducted by other authors, who also reported better performance.20–24
Proof of accuracy, between the different sepsis concepts on the same population, may be useful for further development of a unified sepsis score. Thus, our study aimed to compare the accuracy between severity scores from 3 different definition concepts (SIRS, PIRO and SOFA-based scores), in term of in-hospital mortality prediction among sepsis patients admitted to an intensive care unit.
MethodsWe conducted a retrospective cohort study analyzing data over a 10-year period (from January 1, 2007 to December 31, 2016), using electronic records along with the sepsis and severity scores database of a single medical ICU of a teaching hospital of Prince of Songkla University, Thailand. The protocol was approved by the institutional ethics committee on January 7, 2014 (Approval letter 57-366-14-4).
PopulationPatients 18 years of age or older, who was admitted to our medical ICU with a diagnosis of severe sepsis and septic shock were enrolled regardless of the infection source or acquisition type. We defined sepsis terminology following the criteria of Sepsis-2 definition, according to the starting study period. Patients whose diagnosis was only sepsis using the terminology in Sepsis-2 definition without organ dysfunction were excluded. Organ failure was defined by an increase in the SOFA score of at least 2 points in each organ system. Patients for whom the length of stay was less than 4h were also excluded, because it was too early to evaluate for change in either physiologic response or organ dysfunction.
Data CollectionData for all components of SIRS,6 Moreno PIRO,8 Rubulotta PIRO,9 Howell PIRO,10 and qSOFA19 (detail in Tables S1–S6), as described by the original articles, were collected from the electronic database and Hospital Information System (HIS) of our hospital. Database of the studying ICU was manually collected by a well-trained research assistant in our unit.3,25 Parameters of patient predisposition (underlying diseases, age, gender, chronic illness etc.) were based on the admission data. Severity of illness was defined using Acute Physiology and Chronic Health Evaluation II (APACHE-II) score.26 APACHE II and SOFA scores were derived from sepsis and severity scores database. Parameters of infection (infection source and acquisition type) were based on data from a final summary of hospital admission. Worst values of parameters within the first 24h of ICU admission, related to physiological change and laboratory data were used to calculate the scores. The primary outcome was all causes of in-hospital mortality. The secondary outcome was ICU mortality. All parameters were electronically recorded using Epidata 3.1.
Statistical analysisBaseline characteristic data were analyzed and represented with mean±SD, or median with interquartile range (IQR), according to data type and distribution. Student T-test was used for normal distribution data, and Wilcoxon's rank sum test for non-normal distribution data. We used the area under receiver operating characteristic curve (AUC) to determine discrimination among scores. Discrimination is an ability of the score to distinguish between survivors and non-survivors. Pair-wise comparison between the AUC of each score using method by the Delong et al.,27 and used Bonferroni correction for multiple comparisons of the AUC. Stata version 11 was used for all of statistical analysis. A p-value of less than 0.05 is accepted as a statistical significance. Serum lactate measurement, which is a component in Howell PIRO score,10 were available in our center only after 2011 owing to resource limitation before that period, causing 42.4% of missing data in serum lactate in our database. We also decided to perform sensitivity analysis for Howell PIRO score using the subgroup from the database collected after 2011.
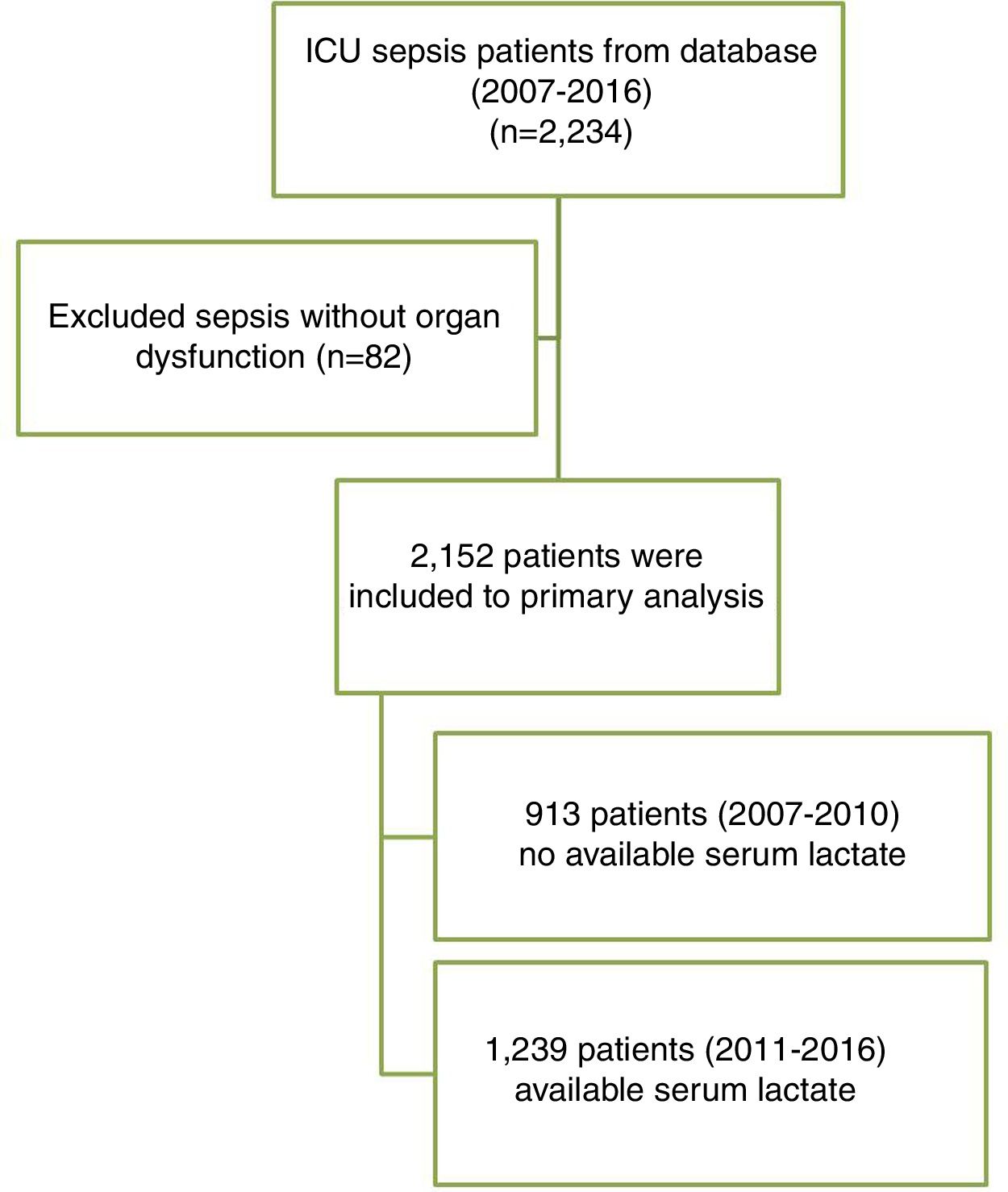
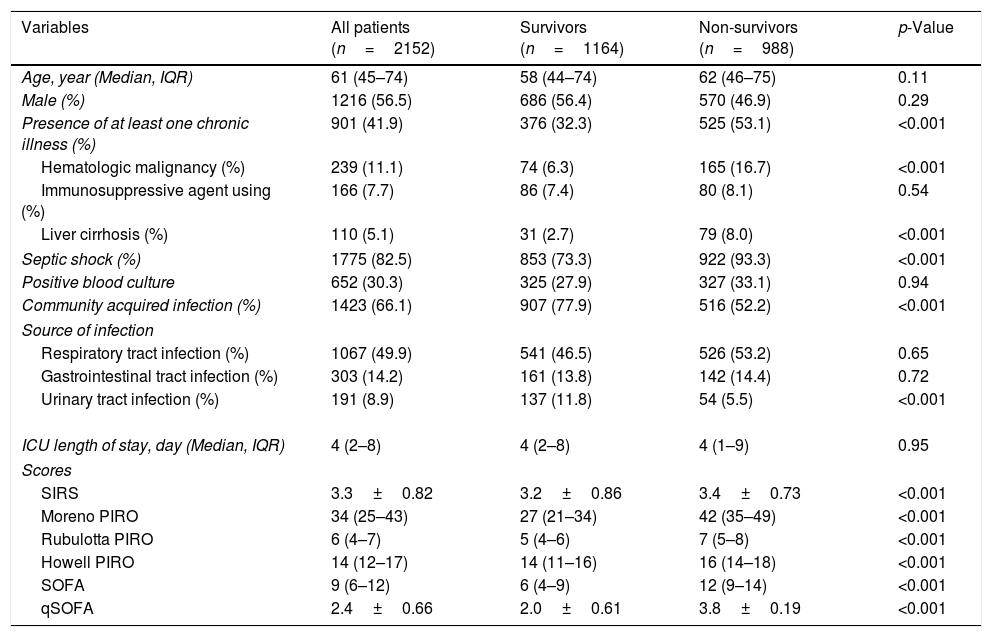
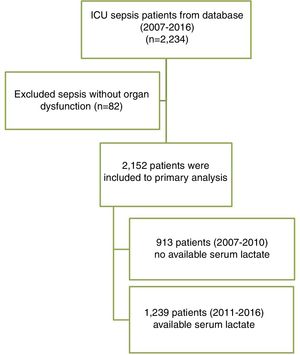
ResultsThere were 6986 patients in the database during the 10-year study period in our ICU. A total of 2234 patients had been diagnosed with severe sepsis and septic shock, using the Sepsis-2 criteria. After exclusion of 82 entries, which were diagnosed as sepsis without organ failure, 2152 patients were included into the primary analysis (Fig. 1). The mean APACHE-II score was 23.9±9.8. The ICU and hospital mortality was 33.3% and 45.9%, respectively. The baseline characteristics of the study population are presented in Table 1.
Patient characteristics data.
| Variables | All patients (n=2152) | Survivors (n=1164) | Non-survivors (n=988) | p-Value |
|---|---|---|---|---|
| Age, year (Median, IQR) | 61 (45–74) | 58 (44–74) | 62 (46–75) | 0.11 |
| Male (%) | 1216 (56.5) | 686 (56.4) | 570 (46.9) | 0.29 |
| Presence of at least one chronic illness (%) | 901 (41.9) | 376 (32.3) | 525 (53.1) | <0.001 |
| Hematologic malignancy (%) | 239 (11.1) | 74 (6.3) | 165 (16.7) | <0.001 |
| Immunosuppressive agent using (%) | 166 (7.7) | 86 (7.4) | 80 (8.1) | 0.54 |
| Liver cirrhosis (%) | 110 (5.1) | 31 (2.7) | 79 (8.0) | <0.001 |
| Septic shock (%) | 1775 (82.5) | 853 (73.3) | 922 (93.3) | <0.001 |
| Positive blood culture | 652 (30.3) | 325 (27.9) | 327 (33.1) | 0.94 |
| Community acquired infection (%) | 1423 (66.1) | 907 (77.9) | 516 (52.2) | <0.001 |
| Source of infection | ||||
| Respiratory tract infection (%) | 1067 (49.9) | 541 (46.5) | 526 (53.2) | 0.65 |
| Gastrointestinal tract infection (%) | 303 (14.2) | 161 (13.8) | 142 (14.4) | 0.72 |
| Urinary tract infection (%) | 191 (8.9) | 137 (11.8) | 54 (5.5) | <0.001 |
| ICU length of stay, day (Median, IQR) | 4 (2–8) | 4 (2–8) | 4 (1–9) | 0.95 |
| Scores | ||||
| SIRS | 3.3±0.82 | 3.2±0.86 | 3.4±0.73 | <0.001 |
| Moreno PIRO | 34 (25–43) | 27 (21–34) | 42 (35–49) | <0.001 |
| Rubulotta PIRO | 6 (4–7) | 5 (4–6) | 7 (5–8) | <0.001 |
| Howell PIRO | 14 (12–17) | 14 (11–16) | 16 (14–18) | <0.001 |
| SOFA | 9 (6–12) | 6 (4–9) | 12 (9–14) | <0.001 |
| qSOFA | 2.4±0.66 | 2.0±0.61 | 3.8±0.19 | <0.001 |
PIRO: Predisposition, Insult/Infection, Response, Organ dysfunction; qSOFA: quick sequential organ failure assessment; SIRS: systemic inflammatory response syndrome; SOFA: sequential organ failure assessment.
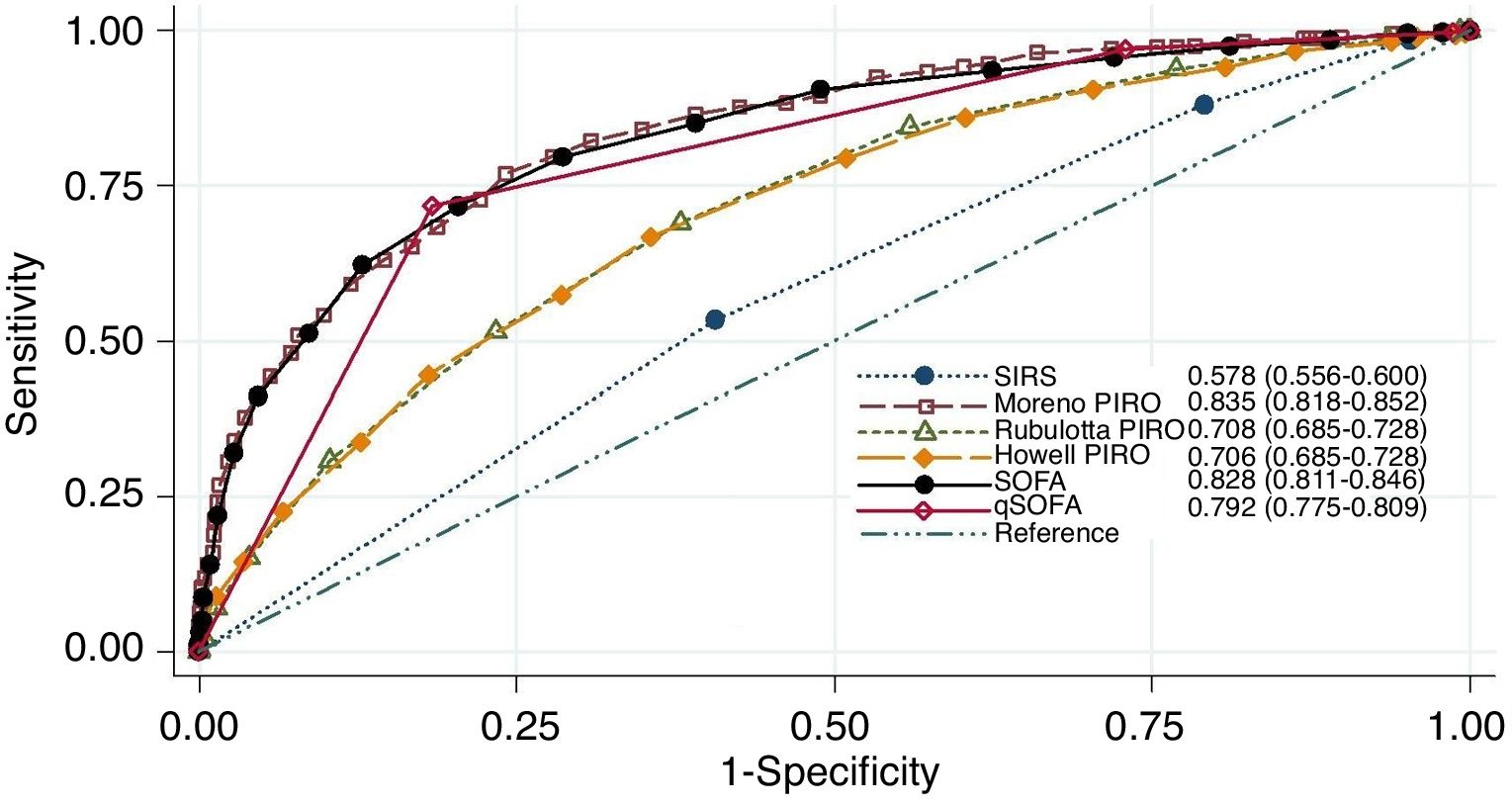
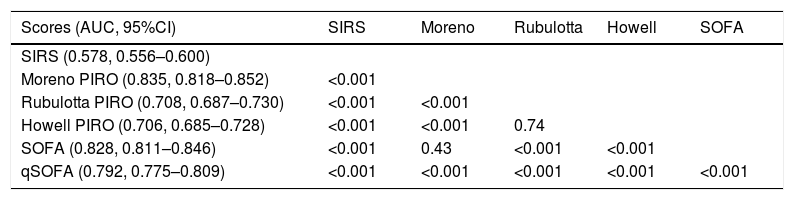
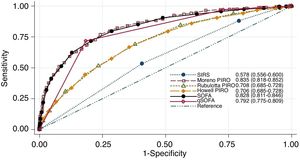
Mortality tended to be higher according to the score increasing, in all scores, except SIRS (Figures S1–S3). The Moreno PIRO score had the highest AUC for in-hospital mortality (0.835, 95%CI 0.818–0.852), followed by SOFA score (0.828, 95%CI 0.811–0.846), qSOFA (0.792, 95%CI 0.775–0.809), Rubulotta PIRO score (0.708, 95%CI 0.687–0.730), Howell PIRO score (0.706, 95%CI 0.685–0.728), and SIRS (0.578, 95%CI 0.556–0.600). However, the AUC of SOFA score was not statistically different with Moreno PIRO score (p=0.43). The AUC of SOFA and Moreno PIRO scores were significantly higher than that of other scores (Table 2 and Fig. 2). Nevertheless, the APACHE II score provide the higher AUC (0.883, 95%CI 0.868–0.897) than SOFA and other PIRO scores.
Area under receiving operating characteristic (AUC) and p-value comparison between sepsis based-scores for in-hospital mortality.
| Scores (AUC, 95%CI) | SIRS | Moreno | Rubulotta | Howell | SOFA |
|---|---|---|---|---|---|
| SIRS (0.578, 0.556–0.600) | |||||
| Moreno PIRO (0.835, 0.818–0.852) | <0.001 | ||||
| Rubulotta PIRO (0.708, 0.687–0.730) | <0.001 | <0.001 | |||
| Howell PIRO (0.706, 0.685–0.728) | <0.001 | <0.001 | 0.74 | ||
| SOFA (0.828, 0.811–0.846) | <0.001 | 0.43 | <0.001 | <0.001 | |
| qSOFA (0.792, 0.775–0.809) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
PIRO: Predisposition, Insult/Infection, Response, Organ dysfunction; qSOFA: quick sequential organ failure assessment; SIRS: systemic inflammatory response syndrome; SOFA: sequential organ failure assessment.
The SOFA score present the best discrimination with an AUC with 95%CI of 0.838, 0.820–0.855 to predict ICU mortality. There were no differences of AUCs between Moreno PIRO score and qSOFA (AUC with 95%CI 0.804, 0.785–0.823 and 0.787, 0.770–0.805, respectively), but their performance were statistically higher than other scores to predict ICU mortality (Table S7). The AUCs of each score to predict the ICU mortality are shown in Figure S4 and Table S7.
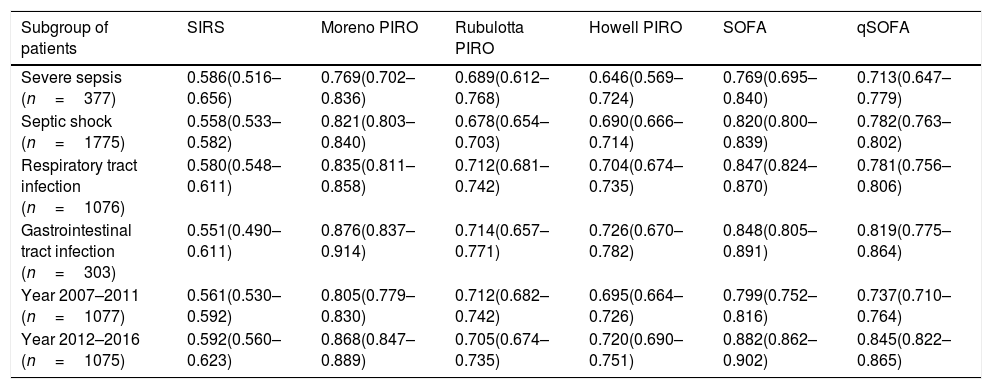
The discrimination of each score for subgroups analysis is shown in Table 3. There was similar predictive ability of SOFA and Moreno PIRO to predict hospital mortality in all subgroup of sepsis patients, as well as, the AUCs of both scores were statistically higher than SIRS and other PIRO scores to predict hospital mortality in all subgroup of our sepsis patients.
Comparison of the area under receiver operating characteristic curve (AUC) for sepsis based-scores for predict in-hospital mortality.
| Subgroup of patients | SIRS | Moreno PIRO | Rubulotta PIRO | Howell PIRO | SOFA | qSOFA |
|---|---|---|---|---|---|---|
| Severe sepsis (n=377) | 0.586(0.516–0.656) | 0.769(0.702–0.836) | 0.689(0.612–0.768) | 0.646(0.569–0.724) | 0.769(0.695–0.840) | 0.713(0.647–0.779) |
| Septic shock (n=1775) | 0.558(0.533–0.582) | 0.821(0.803–0.840) | 0.678(0.654–0.703) | 0.690(0.666–0.714) | 0.820(0.800–0.839) | 0.782(0.763–0.802) |
| Respiratory tract infection (n=1076) | 0.580(0.548–0.611) | 0.835(0.811–0.858) | 0.712(0.681–0.742) | 0.704(0.674–0.735) | 0.847(0.824–0.870) | 0.781(0.756–0.806) |
| Gastrointestinal tract infection (n=303) | 0.551(0.490–0.611) | 0.876(0.837–0.914) | 0.714(0.657–0.771) | 0.726(0.670–0.782) | 0.848(0.805–0.891) | 0.819(0.775–0.864) |
| Year 2007–2011 (n=1077) | 0.561(0.530–0.592) | 0.805(0.779–0.830) | 0.712(0.682–0.742) | 0.695(0.664–0.726) | 0.799(0.752–0.816) | 0.737(0.710–0.764) |
| Year 2012–2016 (n=1075) | 0.592(0.560–0.623) | 0.868(0.847–0.889) | 0.705(0.674–0.735) | 0.720(0.690–0.751) | 0.882(0.862–0.902) | 0.845(0.822–0.865) |
PIRO: Predisposition, Insult/Infection, Response, Organ dysfunction; qSOFA: quick sequential organ failure assessment; SIRS: systemic inflammatory response syndrome; SOFA: sequential organ failure assessment.
However, there were only 1239 patients having had their serum lactate values, so as to be included into subgroup analysis. In subgroup analysis, the AUC of Howell PIRO score was higher than the whole population (0.724 vs. 0.706). However, the performance of Howell PIRO to predict primary outcome was lower than Moreno PIRO and SOFA score and similarly to Rubulotta PIRO, as same as the entire population (Table S8).
DiscussionTo the best of our knowledge, this is the first comparison of severity scores derived from all sepsis definition concepts. We found both the SOFA and Moreno PIRO score had the highest mortality discrimination, additionally they were also higher than the value reported in original articles of both scores (AUC of SOFA and Moreno PIRO score in original article was 0.7419 and 0.772,8 respectively). This finding may be owing to the higher mortality in our center, compared with worldwide epidemiologic data.2 Although, we hypothesized that both SOFA and Moreno PIRO scores still preserve their good performance, even in a more severe sepsis patients. This statement may not be true for other scores, as their AUC did not result in as good results, as in their original articles.9,10,19 Actually, components of organ dysfunction in the Moreno PIRO score8 was derived from the original SOFA, hence, may explain why the Moreno PIRO score is better than other PIRO scores. Even though these results may not directly conclude that the organ failure concept is better than other concepts for sepsis, we found that scores that, focus around organ failure seem to have better mortality discrimination than other scores.
In this study, we aimed to compare between different sepsis definitions. Thus, we excluded patients without organ dysfunction, in order to unify the study population into the same terminology, which preserves severe sepsis in Sepsis-1 and Sepsis-2 definition is actually the same as sepsis in Sepsis-3 definition. Fortunately, sepsis patients without organ dysfunction were the minority our study population (only 3.6%), and may not have affected the primary outcome.
Previous studies from other investigators had conflicted results. MacDonald et al. compared Howell PIRO, SOFA, and Mortality in ED Sepsis (MEDS) in 240 sepsis patients, who visited an emergency department, and found that the Howell PIRO score performed better than the SOFA score, and similarly to the MEDS score to predict 30-day mortality.28 We hypothesized that the SOFA score may have better performance in an ICU setting, rather than in an emergency department setting, which is too early to detect changes in organ functions during the diseases course. Thus, the PIRO concept that includes predisposition factors in the score should be used in this setting. The study also included infections with no organ dysfunction (18% of study population), which is not considered to be sepsis nowadays. Another study from de Groot et al. also found that the performance of Howell PIRO, qSOFA, MEDS, Modified Early Warning Score (MEWS), National Early Warning Score (NEWS) in an emergency department setting were poor and the AUC ranged from 0.56 to 0.64 in older patients, significantly lower than the good AUC range from 0.72 to 0.86 in younger patients (lower than 70 years). The qSOFA had a lower AUC than that of the Howell PIRO score.29 Although some of the study populations in this study were within the older age group, most of them were younger than 70 years of age. The difference in both the study population and setting may explain the different results. The study of de Groot et al. also reported lower mortality (9.5%)29 compare with ours, and qSOFA discrimination may not as good as our results. Tafelski et al. compared the accuracy between three PIRO scores, based on a model of the critically-ill in an ICU, and they found that Moreno PIRO and Howell PIRO were statistically different compared with Rubulotta PIRO.30 Most of the patients in this study were in the organ dysfunction group, much like our study, but hospital mortality was 16.2% lower than our results. Different PIRO scores may have different accuracy dependant on population settings and sepsis severity.
Our findings also support that among the more severe sepsis patients, use of SOFA score, which focus on organ dysfunction has more advantage in mortality prediction. Moreover, SOFA score is more simplified and easier to use than Moreno PIRO score, even though all of them have a comparable discrimination performance. We support the use of the SOFA score more so, than the Moreno PIRO score for risk prediction in ICU sepsis patients.
The limitation of our study was that it only included sepsis patients admitted into a medical ICU of a university teaching hospital; these results may some limitation in application in other sepsis patients in other ICU or sepsis in wards or emergency department. Secondly, our results had a higher prevalence of septic shock and high mortality rate; these findings may not be generalized to less severely-sepsis patients. More studies are required to clarify prognostic determination among these different phenotypes of sepsis patients. Thirdly, the accuracy of these scores for predicting mortality in sepsis patients diagnosed according to Sepsis-2 criteria may not be the same as those diagnosed using the new Sepsis-3.
ConclusionSeverity scores derived from the Sepsis-3 concept that consists of organ dysfunction and organ failure assessment have better discrimination performance than other concepts. Our findings support SOFA score for risk prediction in medical-based ICU sepsis patients.
Authors contributionThe study concept and design was created by all authors. TS and BK collected data and performed the statistical analysis. TS drafted the manuscript. BK has reviewed and revised manuscript. All authors read and approved the final manuscript.
Conflict of interestNone.
This study was supported by a research grant from the Faculty of Medicine, Prince of Songkla University. The authors would like to acknowledge Mr. Andrew Tait, of the International Affairs Department, Faculty of Medicine, Prince of Songkla University for his help in editing the manuscript.