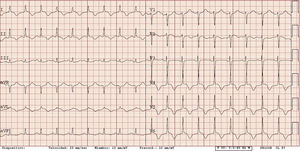
A 49-year-old woman with a history of intravenous drug abuse in the past and treated with buprenorphine presented due to diarrhea and abdominal pain. She had suspended buprenorphine 36h ago. In the emergency room she developed typical sudden onset chest pain with manifestations of heart failure with arterial hypotension. The chest X-rays showed lung edema (Fig. 1). The laboratory tests indicated troponin I elevation (1.7μg/l; reference range 0–0.5), with increased NT-proBNP (17,480pg/ml). The ECG tracing is shown in Fig. 2.
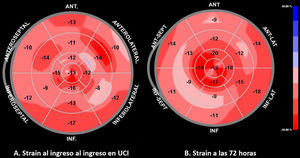
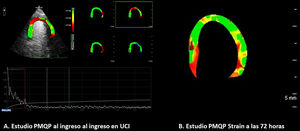
The patient was admitted to intensive care, and echocardiography (video 1) with strain assessment evidenced severe hypokinesia of the middle and apical segments, with an ejection fraction of 38% and diminished global longitudinal strain (−12.4%), associated to loss of the physiological apical gradient (in normal strain the apical segments show greater values than at middle and basal level – the normal global longitudinal strain being −20%±2%) in the polar map (Fig. 3A). The echocardiographic parametric quantitative myocardial perfusion study with echocontrast (SonoVue®) is shown in Fig. 4A. The condition was treated as acute coronary syndrome without ST-segment elevation, with volume depletion and inotropic therapy with levosimendan. Coronary angiography after 36h revealed no obstructive coronary disease (video 2). The troponin I peak was 4.9μg/l. After 72h the patient was hemodynamically stable and without signs of heart failure. The echocardiogram showed normalization of the segmental alterations, with an ejection fraction of 55% (video 3). The strain polar map indicated recovery of the apical gradient but with a slightly decreased global longitudinal strain (−14.2%; Fig. 3B). The parametric quantitative myocardial perfusion study showed improved septoapical perfusion (Fig. 4B). The ECG tracing obtained at that time is shown in Fig. 5.
Please cite this article as: Keituqwa Yáñez I, Nicolás Franco S, Arcís Conesa A. Valoración ecocardiográfica integral en un caso de miocardiopatía de takotsubo por privación de opiáceos. Med Intensiva. 2019;43:591–592.