Information is one the main needs for the families of critically ill patients, and handing out to them a leaflet or a welcome guide at admission contributes to reducing the levels of anxiety involved.1 Back in 2017, the Spanish Society of Intensive Care Nursing and Coronary Units (SEEIUC) published a set of recommendations on how to welcome family members to intensive care units (ICU) recommending the use of written guidelines with information on the characteristics and rules of the ICU, aspects regarding the patient, and questions associated with the family.2
The objective of this study was to describe the content of the welcome guides of Spanish ICUs based on the recommendations set forth by the SEEIUC.
This was a descriptive, cross-sectional, and multicenter trial conducted from September 2019 through February 2020 that included 280 Spanish ICUs of adult patients based on a list created by the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (SEMICYUC). The content of such recommendations was evaluated. The different welcome guides were obtained after contacting personnel from the different ICUs via e-mail, phone call or social media like Twitter or just by checking the hospital official website.
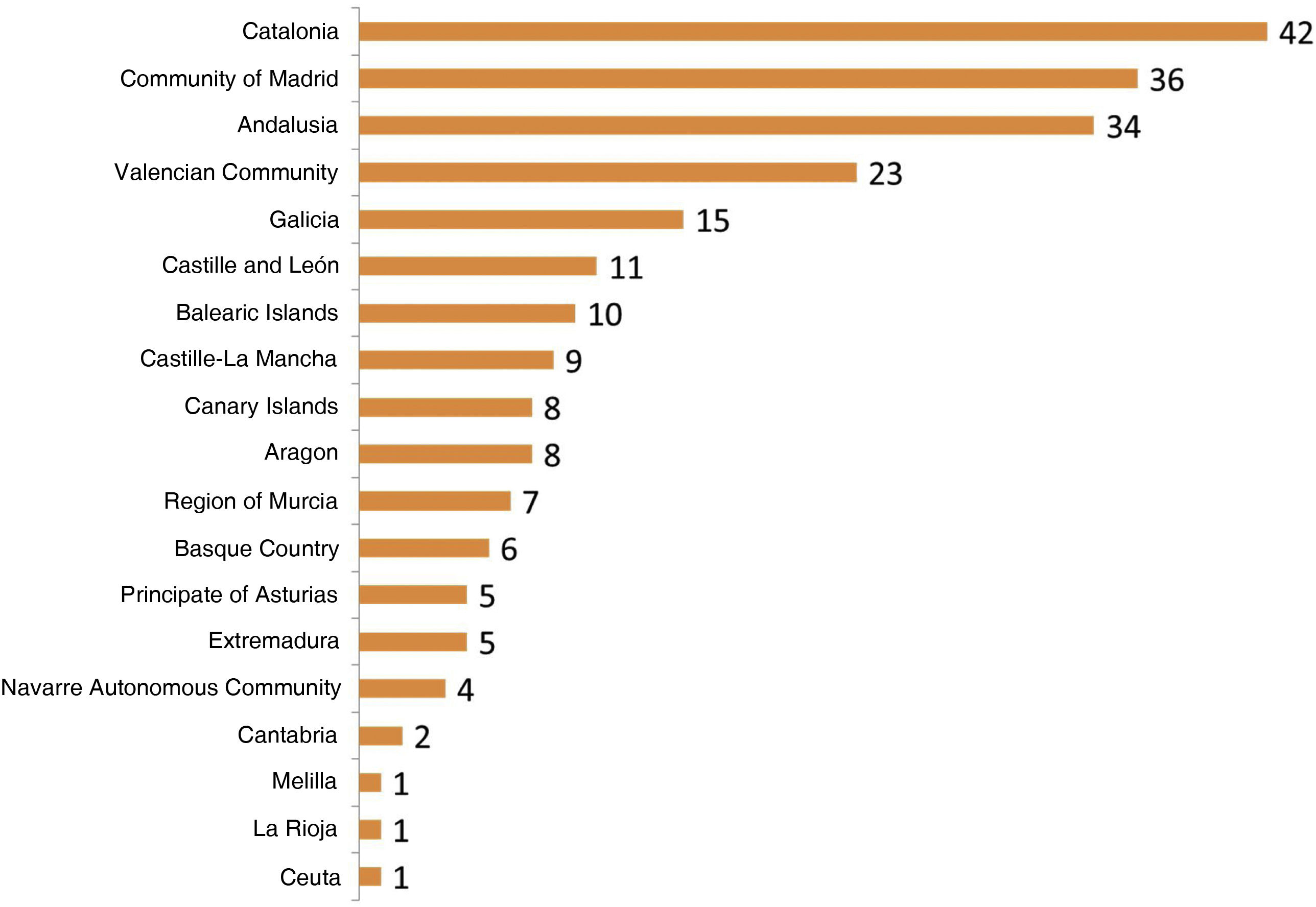
Data from 228 Spanish ICUs (81.4%) were eventually collected with representation from all the different Spanish autonomous communities (Fig. 1). A total of 75.4% of these were public ICUs while 24.6% were private. A total of 51.8% were teaching hospitals.
A total of 89% of the ICUs involved (N = 203) had welcome guides available while 11% (N = 25) offered this information verbally or through posters hanging from the unit walls.
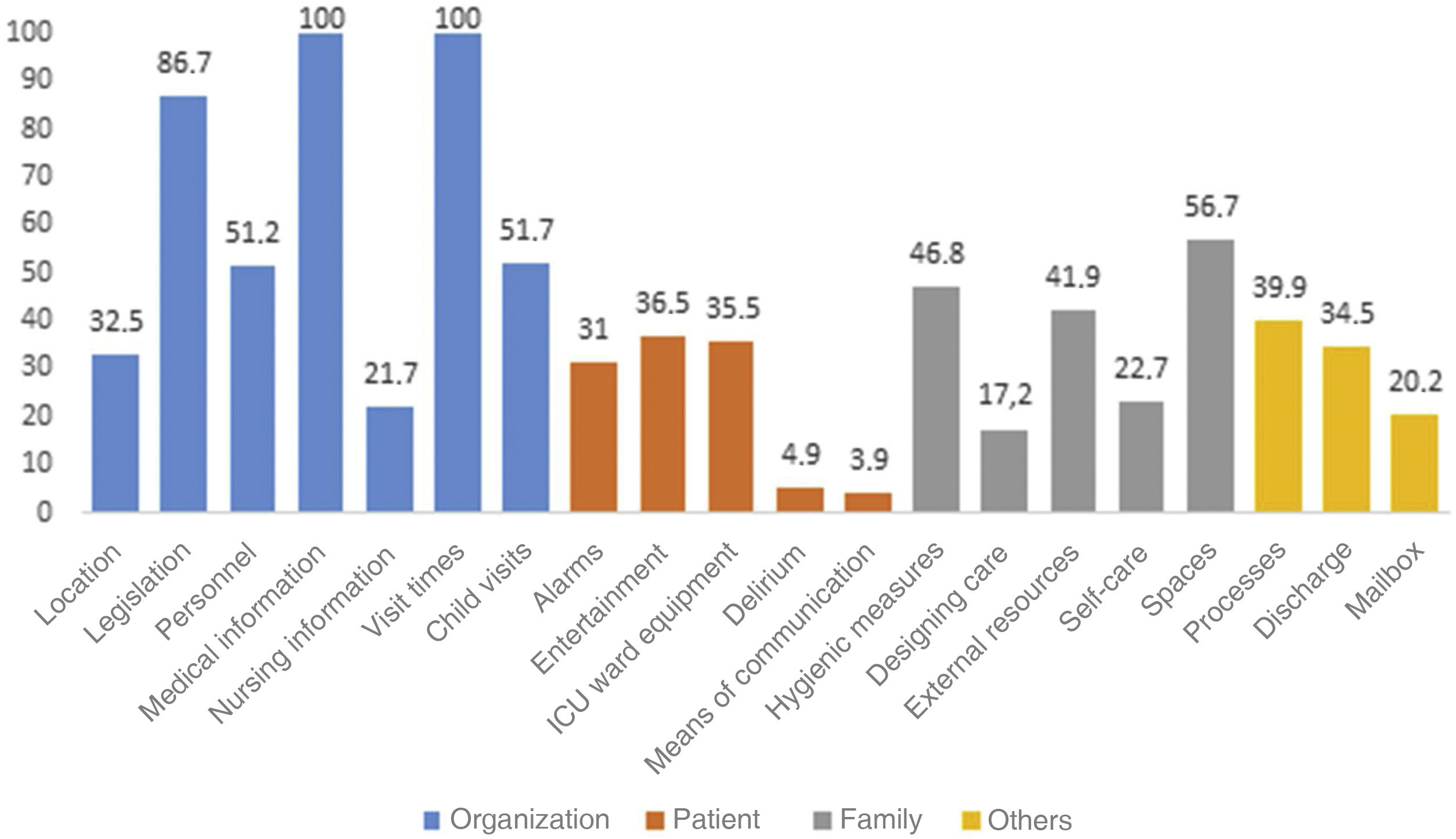
Fig. 2 shows the frequency with which recommendations appeared on the Spanish welcome guides. Fifty per cent of the content of most of these guides was never observed. In 2 ICUs the guides picked up all the recommendations.
Medical information appeared in 100% of the guides. Daily information was provided in 99% of them and schedules were included in 97.5% of the guides. Also, in 47.3% of the guides, information on hospital admission was provided, in 69.5% if there were relevant changes regarding the patient, and in 21.7% upon family request.
Nursing information appeared in 21.7% of the guides. In 65.9% information schedules were specified, and in 38.6% this information schedule matched the visit times.
In 3% of the guides (N = 6) doctor-nurse information appeared altogether.
Regarding visit times, 8 ICUs (3.9%) had no time restrictions, that is, they had an open doors policy. In 96.1% of the ICUs some type of restriction was seen, although 42.4% complemented it with a flexible schedule or accompaniment.
During visit hours, 46.8% of the ICUs allowed access to minors although 25.6% of these ICUs had some type of age-based restriction. In 4.9% of the ICUs minors were not allowed while 48.3% of the ICUs had not child restrictions whatsoever.
Regarding patient situation, the means of communication available to each ICU and delirium were the two less mentioned topics in the guides, with 3.9% and 4.9%, respectively. The most highly mentioned recommendation regarding the family situation were the spaces available like the waiting room or the cafeteria with 56%.
Handing out an informative guide upon the critically ill patient’s arrival to the ICU is a common practice in Spain. Its content, however, is not very representative of most aspects recommended by the SEEIUC. Two similar, though older, clinical trials conducted in the United Kingdom,3 and France4 also found significant mismatches between their manuals of recommendations and what the leaflets had to say about it. Therefore, it seems that the evolution experienced at the ICU setting over the last decade has not translated into written documents regarding welcoming the families of critically ill patients. On the other hand, writing down all recommendations can be expensive for the centers or over-informative for the families especially when talking about patients with short ICU stays. An alternative to this would be to combine the leaflet with extended information from the hospital official website as it is the case with several Italian ICUs.1
The most recurring aspects picked by the guides were medical information, visit times, and rules and regulations at the ICU setting. This content responds to an old model where families with a passive role were considered external elements with highly restricted visit times and no involvement in the patient’s healthcare process whatsoever. Policy on visits is still restrictive despite multiple recommendations on the benefits of opening the doors to the patients and their families.5 However, almost half of the leaflets speak about making time schedules more flexible, which is why we think the tide is changing in Spain. However, it is surprising to see that the tendency to widen time visits is not accompanied by tools to facilitate patient-family communication, a common problem of critically ill patients. Also, it is surprising to see that very few ICUs proposed citizen participation despite being a common family demand.6,7 This increased time offered to the families has more to do with watching and accompanying the patient than with collaborating and being involved in the healthcare process like the IC-HU Project: Humanizing Intensive Care suggests.8 This is a project that triggered a paradigm shift at the Spanish ICUs.
On the other hand, access of minors to the ICU is still a controversial issue, and healthcare professionals justify this prohibition on the psychological impact or risk of infection involved,9 though this has proven unfounded.10 Child visits is a barrier that should be broken always with individualized planning among the family, the healthcare professional, and the patient.
Regarding information on the healthcare process, the doctor is the one handing all information out to the family while, but nurse is the big absentee here from the entire formal information process7 despite being the closest healthcare professional to the patient and his family.
In conclusion, the content of welcome guides shows a reality that is far from the recommendations established by the SEEIUC and the humanization of care proposed. Yet such proposals need to be included by updating the guides, something that many ICUs are already doing. What is not made available and remains unknown to the families will never be sought by these.
Authors’ contributionsBoth authors contributed equally to the study design, data curation and analysis, and to the process of drafting the manuscript.
Conflicts of interestAuthors declared that this study received no specific funding from any public, private or non-government organizations.
Authors declared no conflicts of interest whatsoever.
We wish to thank all those people who, anonymously and from their own working stations—nurses, nurse technicians, doctors, sales representatives, unionists, supervisors, friends or acquaintances—made their contributions so this project could become a reality.