A 78-year-old woman with a history of smoking, hypertension, chronic obstructive pulmonary disease, and type 2 diabetes mellitus presented sudden death. After advanced life support, she recovered a pulse. On the EKG, a newly acquired right bundle branch block (RBBB) was detected and she was urgently transferred to the CT scanner to rule out a massive pulmonary embolism. During image acquisition, the patient became hypotensive and suffered another cardiac arrest.
Contrast-enhanced multidetector CT showed “passive” filling of the right cardiac chambers with contrast material occupying the lower part of the chambers.
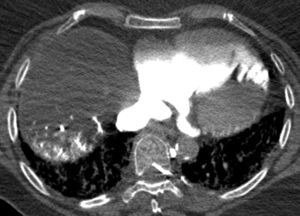
Retrograde flow of the contrast agent was also observed through the right atrium into the coronary sinus and the great cardiac vein, filling the cardiac veins of the left ventricle (Fig. 1), and from the inferior vena cava into the right hepatic vein and right hepatic lobe (Fig. 2).
These findings are pathognomonic of the absence of blood flow during the procedure.
After 30min advanced life support, the patient died.