The ratio of partial pressure of oxygen to fractional inspired oxygen (PaO2/FiO2) is the standard in acute respiratory distress syndrome (ARDS).1 The invasiveness of arterial puncture for arterial blood gas testing along with the lack of continuous information have encouraged the use of less invasive tools such as pulse oximetry, which determines transcutaneous oxygen saturation (SaO2). Other advantages of pulse oximetry include its easy interpretation, high sensitivity in hypoxemia situations, and availability in any setting.2,3 However, it presents several disadvantages such as a) the possibility of error in measuring severe hypoxemia and in the classification and severity level of ARDS; b) the inaccuracy in patients with shock or SaO2 > 97%.2,3 Although the SaO2/FiO2 ratio has been proposed as a tool for the diagnosis and severity of ARDS,2,3 guidelines on the management of ARDS question the validity of this ratio.4 In patients with COVID-19 related pneumonia, several studies have shown a good correlation between SaO2/FiO2 and PaO2/FiO2.5,6 Based on this, SaO2/FiO2 could estimate the severity of ARDS in patients with COVID-19 related pneumonia.
However, for 2 variables to be used interchangeably, correlation and agreement analysis (along with the degree of agreement) are necessary.7–9 The objective of this study was to analyze the homogeneity between SaO2/FiO2 and PaO2/FiO2 ratios in patients with COVID-19 related pneumonia.
This was a retrospective and observational study conducted in 2 intensive care units from March 2020 through August 2021. The study was approved by the Drug Research Ethics Committee (code 66/20), and informed consent was not deemed necessary due to the study’s characteristics. Patients ≥18 years old, admitted due to COVID-19 related pneumonia, and requiring non-invasive ventilation (NIV) were included. At the beginning of NIV, gasometric analysis was performed using an ABL 90 FlexPLUS analyzer (RadiometerMedicalApS, Brønshøj, Copenhagen, Denmark). SaO2 was recorded after verifying the correct pulse oximetry signal on the Philips IntelliVue MX700 monitor. The recorded FiO2 came from the NIV devices used, the tables established by the manufacturer (in Venturi masks), or calculation [21 + Flow (L/min) × 3] in reservoir masks.10 First, Spearman’s correlation was analyzed; subsequently, due to the non-normality of the variables, logarithmic transformation was performed to turn them into parametric variables. Afterwards, the mean difference (or mean bias) and its standard deviation (SD) were determined using the Student’s t-test. Additionally, agreement analysis (Bland–Altman test)7,9 and its degree (with Kaplan–Meier curve)8 were analyzed for both ratios.
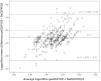
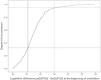
Out of 428 patients—mostly men—aged 59 with hypertension (Table 1 of the Supplementary data), who had received conventional oxygen therapy, 398 patients with both oxygenation variables at the beginning of NIV were selected: PaO2/FiO2 = 110 (84–141) and SaO2/FiO2 = 147 (120–176), respectively. The correlation between both determinations showed an R = 0.744, as seen in the scatter plot (Fig. S1). The comparison using Student’s t-test of the logarithms of both variables was significant [mean difference, −0.11 ± 0.13 standard deviation (SD), (95%CI, −0.13 to −0.10), P = 0.0001]. The agreement analysis and the degree of agreement are shown in Figs. 1 and 2. Like the studies published,5,6 a high positive correlation between both variables was found. However, the results shown in the agreement analysis (Fig. 1) question the homogeneity of both variables: first, several determinations were left outside the standard deviation margins when they should have been inside those margins; second, the mean difference of −0.11 for both determinations did not reach the value of 0 (indicating that both variables are equivalent); and third, there was a wide range between the limits of the standard deviations (0.25 to −0.47). Similarly, the degree of agreement was low (Fig. 2), with only approximately 30% (0.30 in Fig. 2) of the samples showed good agreement for the mean difference of 0.11 obtained previously (i.e., to achieve a 95% agreement between both determinations, there should be a difference of 0.30, which could lead to a significant discrepancy between the values of PaO2/FiO2 and SaO2/FiO2).
Blant–Altman concordance analysis between paO2/FiO2 and SaO2/FiO2. The figure represents the logarithm of the mean difference (Y-axis) between paO2/FiO2 and SaO2/FiO2 vs the average logarithm (X-axis) for these variables. Additionally, the difference has been established using the Student’s t-test with its 2 standard deviation margins (2SD) [−0.11 ± 2 (0.13)]. SD, standard deviation.
In conclusion, a good correlation between both parameters was seen, but the agreement and degree of agreement between both parameters were low, indicating the absence of similarity between both values. Therefore, the SaO2/FiO2 ratio would give us an approximate idea of the patient’s oxygenation level but still far from the true degree of hypoxemia, which could raise doubts for the decision-making process regarding intubation. In light of the results obtained, this study supports the need for further analysis beyond correlation, such as agreement and the degree of agreement, to determine the degree of similarity between both variables, which as observed, were not homogeneous.
The high demand for resources during the pandemic has led to the use of SaO2 for the management of ARDS. According to a proposed algorithm, a patient with SaO2 ≤ 97% (and a SaO2/FiO2 ≤ 315 despite oxygen therapy) would be labeled as having ARDS, and therefore requiring invasive mechanical ventilation.3,10 A multicenter, retrospective study (n = 1028 patients with COVID-19) found a good correlation between PaO2/FiO2 and SaO2/FiO2 as determinants of the degree of ARDS: a PaO2/FiO2 ≤ 200 and ≤100 would correspond to a SaO2/FiO2 ≤ 336 and ≤178,6 respectively. The question at stake is not the diagnosis of ARDS but whether with SaO2/FiO2 values ≤178 (severe hypoxemia), we would consider intubating a patient, or request arterial blood gas testing to corroborate such hypoxemia.
In conclusion, we could question the agreement of PaO2/FiO2 and SaO2/FiO2 ratios in our series of patients with COVID-19 related pneumonia, placing SaO2/FiO2 as a parameter for respiratory evolutionary monitoring but requiring a PaO2/FiO2 ratio to accurately determine the patient’s respiratory status.
FundingNone declared.
Conflicts of interestNone declared.





![Blant–Altman concordance analysis between paO2/FiO2 and SaO2/FiO2. The figure represents the logarithm of the mean difference (Y-axis) between paO2/FiO2 and SaO2/FiO2 vs the average logarithm (X-axis) for these variables. Additionally, the difference has been established using the Student’s t-test with its 2 standard deviation margins (2SD) [−0.11 ± 2 (0.13)]. SD, standard deviation.](https://static.elsevier.es/multimedia/21735727/0000004800000005/v1_202404281348/S2173572724000444/v1_202404281348/en/main.assets/thumbnail/gr1.jpeg?xkr=1dZuESKpnCAWr3yCSGZ24A==)





