Acute respiratory failure is one of the leading causes of death at the ICU setting. In recent years, in addition to optimizing invasive mechanical ventilation and medical treatment, the management of veno-venous extracorporeal membrane oxygenation (VV-ECMO) respiratory support has improved. Recent randomized trials suggest that this therapy should not be delayed in cases of severe refractory respiratory failure to conventional therapy.1,2
The survival rate of adult patients on elective or emergency VV-ECMO support is nearly 60%, meaning that it is essential to understand the management, type of cannulation, and potential complications of this respiratory support system, which is on the rise.2
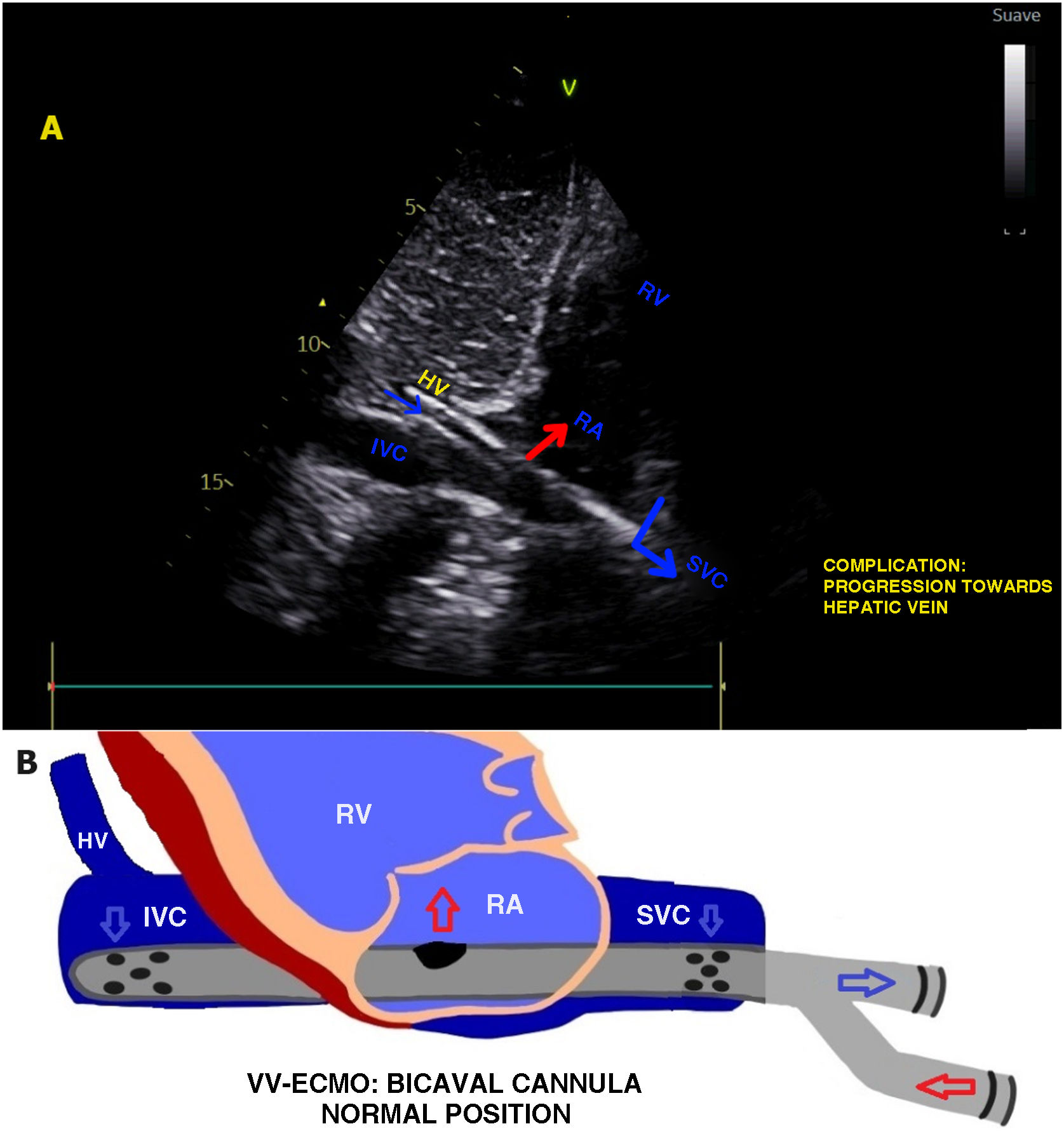
The double-lumen bicaval catheter, inserted through the jugular vein, is a rather safe option for patients who need VV-ECMO respiratory support, as it only requires 1 access site for the device. This type of cannula drains deoxygenated blood from the superior and inferior vena cavae to eventually reinfuse oxygenated blood into the right atrium toward the tricuspid valve (Fig. 1). The fluoroscopy and/or echocardiography-guided insertion is often performed using the Seldinger technique (percutaneous).3
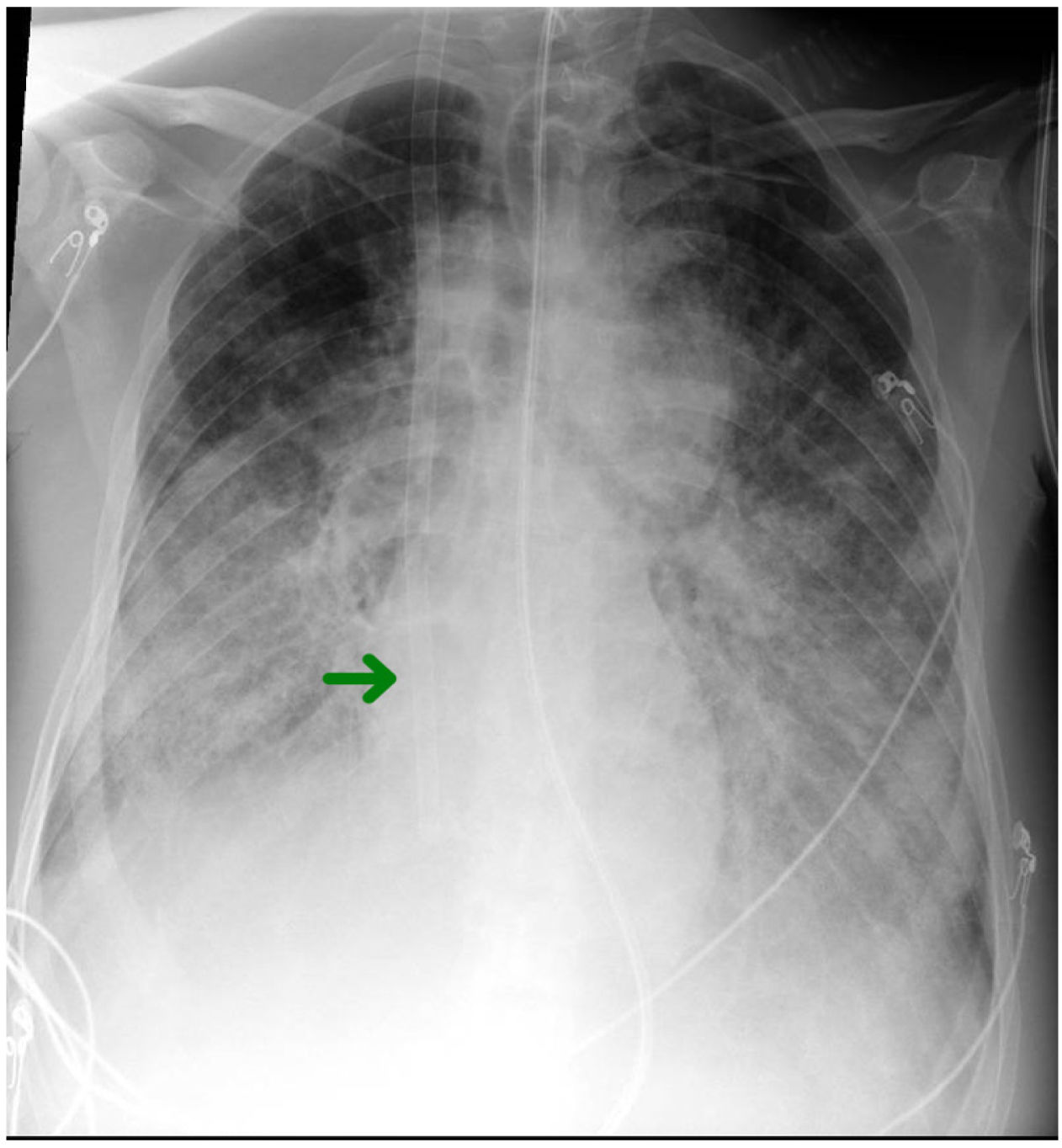
However, every technique has potential complications. In fact, up to 10% of all bicaval cannulas may experience migration or malapposition after insertion, with the distal end being able to progress into cardiac chambers, thus posing a risk of perforation, or even appearing to be in the normal position by fluoroscopy (in the inferior vena cava) while actually lodged in suprahepatic veins, as shown in the example (Fig. 2 and Video). This complication results in decreased drainage flow due to the inability to suction the lower territory, thus leading to inadequate oxygenation of the patient. Therefore, the use of fluoroscopy, along with ultrasound control to confirm the proper position of the ECMO cannula and subsequent monitoring at the ICU setting is increasingly advised.4
As described by Martin-Villen et al. in their update on the role of ultrasound in critically ill patients on ECMO, thoracic ultrasound, along with echocardiography allows for an overall and more comprehensive monitoring of patients on VV-ECMO. These imaging modalities are useful and minimally invasive tools to assess the proper position and daily function of the cannula, the progression of lung disease, and biventricular function (especially right ventricular) for both respiratory and cardiac support.5
In conclusion, given the constant advances and increased use of support devices such as ECMO in intensive care units, a multimodal and multidisciplinary approach to these complex patients becomes essential. Proper training of intensivists in diagnostic tools and daily management, such as the ultrasound applied to critically ill patients, is becoming increasingly accessible in our ICUs with a clear positive impact on our patients’ morbidity and mortality rates.
FundingNone declared.
Author contributionsThe three authors, as a working team, have contributed equally to both the diagnosis and treatment of the patient, as well as in the preparation and drafting of this manuscript.
Conflicts of interestNone declared.