To evaluate different characteristics of patients with acute coronary syndrome (ACS) without ST-segment elevation compared with transient ST-segment elevation.
DesignAn observational, prospective study.
SettingA 12-bed coronary care unit.
PatientsConsecutive patients of ACS without persistent ST-segment elevation.
Main variables of interestThe population was divided intro 2 groups according to the presence of transient ST-segment elevation. Variables of interest were age, cardiovascular risk factors, troponin I and glucose concentrations on admission, coronary anatomy, left ventricular ejection fraction, inhospital mortality and drugs.
ResultsPatients identified as ACS with transient ST-segment elevation were significantly younger, smokers and predominantly male. At the same time, they showed a minor peak elevation of troponin I, a higher ejection fraction and, mainly single-vessel coronary disease.
ConclusionsPatients with ACS with transient ST-segment elevation differ in the type of population, myocardial damage and coronary angiographic results with respect to patients with ACS without ST-segment elevation. More research is needed to clarify whether these differences imply a different therapeutic approach.
Evaluar características diferenciales de los pacientes con síndrome coronario agudo (SCA) sin elevación del segmento ST en comparación con elevación transitoria del segmento ST.
DiseñoEstudio prospectivo observacional.
ÁmbitoUnidad coronaria de 12 camas.
PacientesEnfermos consecutivos de SCA sin elevación persistente del segmento ST.
Principales variables de interésLa población se dividió en 2 grupos, en función de la presencia de elevación transitoria del segmento ST. Las variables de interés fueron: edad, factores de riesgos cardiovasculares, concentraciones de troponina I y glucemia al ingreso, anatomía coronaria, fracción de eyección del ventrículo izquierdo, mortalidad intrahospitalaria y fármacos intrahospitalarios.
ResultadosLos pacientes identificados con SCA y elevación transitoria del segmento ST eran significativamente más jóvenes, fumadores y con predominio del sexo masculino. A su vez, presentaban una elevación pico de troponina I menor, mayor fracción de eyección y principalmente enfermedad coronaria de un vaso.
ConclusionesLos pacientes con SCA con elevación transitoria del segmento ST presentan diferencias en cuanto al tipo de población, daño miocárdico y resultados angiográficos con respecto a los pacientes con SCA sin elevación del segmento ST. Son necesarias más investigaciones para esclarecer si dichas diferencias implicarían un manejo terapéutico diferente.
Acute coronary syndrome (ACS) with non-persistent ST-segment elevation is characterized by the briefness of the electrocardiographic changes. Transient or non-persistent ST-segment elevation is defined as elevation that resolves in less than 30min without reperfusion therapy of any kind.1 The current treatment guides advocate management very similar to that of ACS2 without ST-segment elevation, though the studies or publications in support of such recommendations, or which explore the differential characteristics between the two disorders, are still insufficient. The present study aims to further our knowledge of these aspects, which we feel may be of relevance for management and prognosis.
Patients and MethodsA prospective cohort study was carried out from November 2008 to October 2009, involving in-hospital patient follow-up and assessing all subjects admitted to the Coronary Unit of the Department of Cardiology of a tertiary Hospital with a diagnosis of ACS without persistent ST-segment elevation. The study population was divided into two groups according to the presence or absence of transient ST-segment elevation. ACS was diagnosed according to the criteria found in the literature,3 and the patients with ST-segment elevation >1mm on the first electrocardiographic tracing with resolution in less than 30min in the absence of reperfusion treatment were classified as presenting ACS with transient ST-segment elevation.
In both groups we analyzed demographic and basal clinical variables (age, sex, history of arterial hypertension, diabetes mellitus, dyslipidemia and smoking), laboratory test parameters (troponin I peak, blood glucose), hemodynamic variables (coronary anatomy, ejection fraction) and in-hospital mortality. The drug treatments used in both groups during hospital admission were also evaluated.4
The study was approved by the Clinical Research Ethics Committee of the center, and all patients signed the corresponding informed consent document.
The data were analyzed with the SPSS version 15.0 statistical package for Microsoft Windows. Qualitative variables are reported as percentages, while quantitative variables are expressed as the mean±standard deviation (SD). Normal sample distribution was assessed with the Kolmogorov–Smirnov test. Qualitative variables in turn were compared using the chi-squared test, while the Student t-test was used to compare quantitative variables. Two-tailed hypothesis contrasts were used, accepting statistical significance for p<0.05 in all cases.
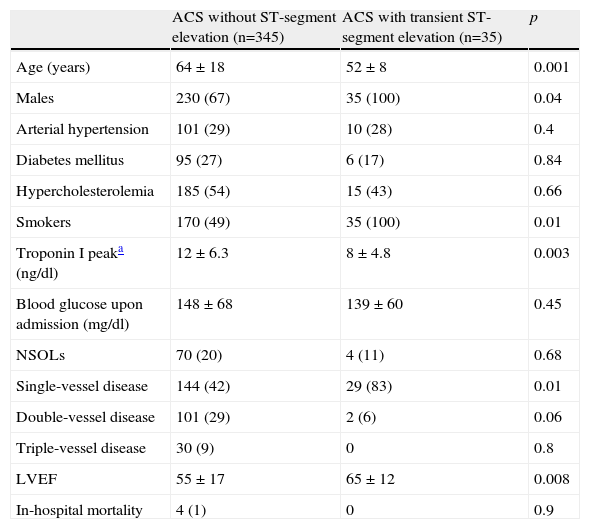
ResultsThe study involved a sample of 380 consecutive patients with ACS without persistent ST-segment elevation (Table 1). All patients were treated to the same extent with aspirin, nitroglycerin, clopidogrel, statins and glycoprotein IIb/IIIa inhibitors. Of the total patients, 35 (9.2%) were classified as presenting ACS with transient ST-segment elevation. In these subjects the mean ST-segment elevation was 4±2.5mm, with resolution of the electrocardiographic changes in 20±8min. The patients identified as presenting ACS with transient ST-segment elevation were significantly younger, smokers, and predominantly males. The laboratory test data in turn reflected a lesser troponin I peak elevation in this group of patients. Regarding the coronary angiographic results, the patients with ACS with transient ST-segment elevation showed a greater prevalence of single-vessel disease. The left ventricle ejection fraction as determined by transthoracic echocardiography in the first 48h after admission was greater in the group presenting ACS with transient ST-segment elevation. There were no statistically significant differences in in-hospital mortality.
Demographic, laboratory test and hemodynamic characteristics of the study population.
| ACS without ST-segment elevation (n=345) | ACS with transient ST-segment elevation (n=35) | p | |
| Age (years) | 64±18 | 52±8 | 0.001 |
| Males | 230 (67) | 35 (100) | 0.04 |
| Arterial hypertension | 101 (29) | 10 (28) | 0.4 |
| Diabetes mellitus | 95 (27) | 6 (17) | 0.84 |
| Hypercholesterolemia | 185 (54) | 15 (43) | 0.66 |
| Smokers | 170 (49) | 35 (100) | 0.01 |
| Troponin I peaka (ng/dl) | 12±6.3 | 8±4.8 | 0.003 |
| Blood glucose upon admission (mg/dl) | 148±68 | 139±60 | 0.45 |
| NSOLs | 70 (20) | 4 (11) | 0.68 |
| Single-vessel disease | 144 (42) | 29 (83) | 0.01 |
| Double-vessel disease | 101 (29) | 2 (6) | 0.06 |
| Triple-vessel disease | 30 (9) | 0 | 0.8 |
| LVEF | 55±17 | 65±12 | 0.008 |
| In-hospital mortality | 4 (1) | 0 | 0.9 |
LVEF: left ventricle ejection fraction; NSOLs: nonsignificant obstructive lesions; ACS: acute coronary syndrome.
Values are expressed as n (%) or mean±standard deviation.
The blood sample for troponin I was processed every 8h during the first day of admission, and then after 48, 72 and 96h. We considered the highest concentration of all the measurements to represent the troponin I peak.
In the present study, the patients showing ACS with transient ST-segment elevation exhibited differences versus the patients with ACS without ST-segment elevation in terms of the type of population, myocardial damage and the angiographic results. Thus, they constitute a special subgroup of individuals with characteristics of their own, clearly differentiated from those of other ACS presentations. Given the scarcity of previous clinical trials in this field, it remains to be established whether these differences imply the need for a different treatment approach in order to afford full benefits for this particular patient population.5,6
Classically, ST-segment elevation on the electrocardiographic tracing has been taken to represent complete occlusion of an epicardial coronary vessel.7 As a result, rapid resolution of this ECG change would indicate rapid resolution of the coronary event. This and the comparatively less pronounced changes in the myocardial damage markers, the predominance of single-vessel disease, and the comparatively greater left ventricle ejection fraction all suggest that there are underlying physiopathological differences involving atherothrombotic and vasospastic phenomena to one degree or other.8
There were no differences between the two groups in terms of in-hospital mortality; however, we consider that longer follow-up would be needed in order to establish possible prognostic differences.9–11 Probably the limited interest in patients of this kind and their low literature repercussion account for the scant importance and indifferentiation of ACS with transient ST-segment elevation found in the clinical practice guides.
We consider that further studies are needed in order to clarify these issues and to contribute new knowledge of this disorder.
Conflict of InterestThe authors have no conflicts of interest to declare.
Please cite this article as: Arroyo Úcar E, et al. Características diferenciales de los pacientes con síndrome coronario agudo sin elevación del segmento ST con respecto a los que tienen elevación transitoria del segmento ST. Med Intensiva. 2011;35:270–3.