Asynchronies during mechanical ventilation are associated with worse prognosis and mortality.1 Double trigger (DT) is the second most common asynchrony after failed cycles.1–3 DT, and the resulting “breath-stacking” can cause pulmonary damage due to an increased tidal volume (TV), high transpulmonary and transvascular pressure, and mismatches in the pressure distribution of lung-dependent regions. Also, it can cause diaphragmatic injuries due to plyometric contractions during maintained insufflation, and also due to eccentric contractions during expiration.4,5 In reverse triggering (RT) (one of the 2 causes of double cycling) the ventilator mechanical cycle induces inspiratory effort in the patient attributed to reflex mechanisms and reported in sedated patients during the assist-control ventilation (ACV) modes.6,7 RT is a known cause for DT and breath-stacking.1,2,5 In these cases, sedation should be increased and relaxation induced to avoid harmful ventilation.4
The other cause for double cycling is the intense and maintained muscle effort made by the patient that, both in flow and in time, exceeds the one made by the ventilator, forcing a second cycle. In these cases, it is recommended to pass on to pressure control or support.5
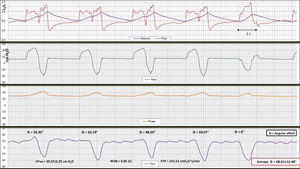
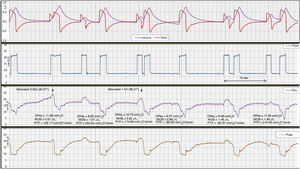
We present 2 cases of DT apparently due to RT questioning what we just described above. Two of our critically ill patients developed asynchronies at the beginning of ventilation weaning. After visual confirmation of the ventilator display, we monitored the airway [Paw]; esophageal [Pes]; gastric [Pgas]; and urinary vesical [Pves] pressures, and flow, confirming the presence of DT with breath-stacking in apparent association with RT. The first case reported is a 62-year-old male patient admitted with signs of subarachnoid hemorrhage complicated with infarct in the protuberance due to vasospasm. Monitorization was performed after 4 days on mechanical ventilation during assist-control mode with constant volume flow (CVF). The second case was a 57-year-old male patient in his first postoperative day after double lung transplantation due to histiocytosis X; in this case, monitorization was performed with pressure support ventilation (PSV).
Monitorization was performed at 1045Hz/channel for 60min. The parameters associated with respiratory effort and work of breathing were analyzed as well as the mismatch between the beginning of the mechanical cycle and the neural cycle (θ=mismatch in s/Ttot×360°), and the frequency of association of both phenomena, DT and RT.
DT due to RT was thought to be associated with the “entrainment” phenomenon where the stimulus of mechanical insufflation generated a neural reflex that caused diaphragmatic contraction.6 In principle, in the presence of patient’s respiratory driver, it was inhibited or dragged by this reflex mechanism.
Afterwards, DT has been categorized into 3 different variants:8 DT with the initial impulse generated by the patient (DTP), which is equivalent to the original DT. Also, DT with the initial impulse generated by the rate programmed in the ventilator followed by the patient’s neuromuscular impulse (DTV), which, in our opinion, could be called “double cycling with false reverse” where the neuromuscular impulse following the mechanical cycle would not be due to neuromechanical coupling or “entrainment”. A good example of this is the one described by Chen et al. as “pseudo-double-triggering”.9 And a variant of the latter due to auto-triggering of the ventilator (DTA). The last 2 variants are often referred to as DT due to RT (Blanch et al.,1 and Aquino Esperanza et al.5).
Note that RT is accompanied by an even higher transpulmonary volume and pressure as shown in Fig. 1 that is potentially harmful both at pulmonary and diaphragmatic level. In our case, the high intensity of the patient’s respiratory driver very much puts into question the reflex origin of this phenomenon
Registry of flow, volume, airway pressure (Paw), vesical pressure (Pves), and esophageal pressure (Pes) in assist-control ventilation mode and continuous flow in the first case. Note the first 4 DTV-type double cycling consecutive cycles. There is an intense patient’s respiratory driver in all the cycles, evident in the delta esophageal pressure (DPes), although at a lower rate than the one programmed in the ventilator. In cycle #5 the patient-triggered mechanical assist inspiration without DT or RT is evident. Figure shows 2 very well-defined respiratory drivers, (one the machine’s and the other the patient’s). Both of a similar intensity (patient’s WOB in 0.85J/L and PTP of 222.53cm H2Os/L). The patient’s inspiratory effort is similar in all the cycles (assisted in cycle #5, and the first 4, DTVs), which is suggestive of a patient’s vigorous respiratory driver (approximate DPes at 30cmH2O) less common and regular compared to the machine one but, in any case, an inexistent driver or a driver “dragged” by the ventilator. The measurement of angular mismatch (θ=68.41°±12.48°) between the patient’s cycle and the ventilator cycle is very different, which also goes against a reflex mechanism. No mismatch in the last assisted cycle reported. In this case the DT-RT 1:1 ratio appeared in 60% of the registry. In the remaining registry it was variable with a 1:2 and 1:3 ratio. In this case, the increased TV of DTV went from 500 cc to almost double. At the same time, the I/E ratio went down to 1:1, a probably unwanted effect. This registry depicts the need for close monitoring when administering presumably protective mechanical ventilation.
The existence of RT in the presence of a patient’s vigorous respiratory driver unrelated to a reflex or entrainment phenomenon has not been fully described to this date except that the denomination DTV does not mean “reflex” RT at all.8 In our opinion, this phenomenon could be called false RT or «pseudo»-RT, and it deserves further investigation.
To this date, this complex interaction between ventilator and patient has only been reported in ventilated patients in ACV mode both with volume and pressure control. For the very first time ever we discussed the existence of this interaction also during the spontaneous ventilation mode represented by case #2 during ventilation with PSV (Fig. 2).
Registry (flow and volume) of Paw, Pes, and Pves signs during pressure support ventilation in case #2. In this case, we presented ventilation with double cycling defined as DTA due to auto-triggering of the ventilator preceding the patient’s respiratory driver (reverse triggering in a general sense). In this case, the patient’s cycle does not start by contracting the inspiratory muscles, but by releasing intense active expiration, as confirmed by vesical pressure. The contraction of the diaphragm comes after active exhalation release. To think that this respiratory driver that includes forced exhalation release and the patient’s inspiratory effort is the product of some reflex does not seem very likely. In this case the correlation between the mechanical and the neural cycles is variable. The parameters associated with inspiratory effort are: DPes: 11.55±1.22cmH2O, note the higher DPes in double triggering; WOB, 1.06±0.42J/L; PTP, 183.95±27.59cmH2Os/min; in this case, work of breathing was associated with the volume generated by cycle stacking corresponding to double cycling. Also, the appearance of double cycling varied.
Due to the different pathophysiology of these 2 types of double cycling we followed the opposite road to the one proposed for their equivalents previously described. In the first case reported, instead of relaxation, pressure support ventilation was suggested. It gradually reduced the intensity of the patient’s respiratory driver and improved synchrony with the ventilator.
In the second example presented, we took the opposite road by increasing external support because, in our patients, active expiration is often the last resource to keep spontaneous ventilation which, although exhausting, does not last long and is not very effective.
In our opinion, the first case shows DT without RT since it is a simple mismatch of 2 different respiratory drivers being the neural one powerful enough to increase TV. The second case does not appear in the medical literature available and should be considered a possibility that can be suspected through abdominal palpation.
The management of this asynchrony should be individualized. In the first case, a short course of CPAP therapy was suggested to see the patient’s spontaneous respiratory driver before returning to relaxation and increasing sedation. We should mention that advanced monitoring is very important here, when available, for the identification of complex interactions between patient and ventilator acting accordingly to reduce the deleterious effects that can come up.10
Conflicts of interestNone reported.
Please cite this article as: Benítez Lozano JA, de la Fuente Martos C, Serrano Simón JM. Doble trigger y ¿falso? reverse trigger. Med Intensiva. 2021;45:e15–e17.