Early enteral nutrition in critically ill patients is essential to preserve the function of villi in the small intestine, regulate immunity, and the systemic inflammatory response.1 Enteral nutrition support is often performed through tubes, being the nasogastric tube (NGT) the one most commonly used.2 Although the rate of complications associated with the insertion of NGTs is very low, some of them can be serious, especially with the NGT has been inserted in an anomalous position (like the airway).3–5 For this reason, the insertion of the NGT should be performed by trained personnel. Also, it is mandatory to confirm the correct position of the NGT using different techniques. The techniques available today are based on tests like the «bubbling» testing (auscultation of bubble sounds following the entry of air), pH stripes to test acidity or the interpretation of ultrasound images. However, the fact that these tests are rather unreliable added to the cost and poor interpretation of the last 2 make it necessary to have another low-cost and useful method at the patient’s bedside like the ultrasound that is widely available in the intensive care units (ICU) setting.
The objective of this study was to assess the diagnostic capabilities of the color Doppler ultrasound (CDU) to detect the position of the NGT in adult critically ill patients.
Back in 2019, a prospective and observational study was conducted at a high-complexity ICU for 4 months. This study was approved by the local ethics committee. Prior to their inclusion in the study, the patients or their families gave their written informed consent.
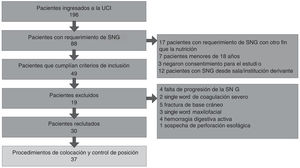
Patients over 18 with an indication for NGT insertion for total or supplementary enteral nutrition at the ICU setting were included
The following patients were excluded: a) patients with congenital or acquired anatomical disorders that would complicate the insertion of the NGT, b) epistaxis within the previous 7 days, c) facial trauma or basilar skull fracture, d) persistent vomiting, e) suspected or confirmed esophageal perforation, f) severe coagulation disorder, g) active digestive bleeding, and h) previous digestive tract surgery or immediate postoperative.
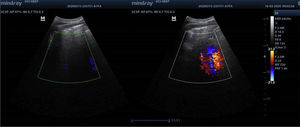
The most commonly used tube for enteral nutrition is the 125 cm long, 10-Fr caliber Silmag® gastrostomy tube (with 3.3 mm of external diameter). This NGT is a tungsten-weighted tube with a semi-rigid guidewire. Experienced medical personnel inserted it and after the instrumentation the stomach was observed to confirm the position of the NGT. The Mindray3C5P (2–5 MHz) convex ultrasound transducer (China) was used. Using an epigastric window, the gastric antrum was identified in bidimensional mode. After visualization of the gastric antrum, a bolus of 20 mL of air was injected through the NGT. At the same time, both in the epigastric window and in the duplex ultrasound (simultaneous two-dimensional mode and color Doppler ultrasound) the presence of a jet or the sudden appearance of a Doppler sign was confirmed (Fig. 1 and video of the Supplementary data). The ultrasounds were performed by trained intensivists in the use of this method. The position of the NGT was considered correct when air was instilled, and the jet was evident in the stomach. On the contrary, the position of the NGT was considered incorrect.
Immediately after performing the ultrasound, an X-ray was used to confirm and monitor the correct placement of the NGT that was interpreted by an expert radiologist in diagnostic imaging modalities and who had been blind to the NGT insertion and the ultrasound. The placement of the NGT was considered correct only through this method when the NGT distal border was found in the stomach.
Variables registered at admission: sex, age; Acute Physiology and Chronic Health Evaluation II (APACHE II), Simplified Acute Physiology Score II (SAPS II), and disease (clinical, trauma, surgical).
Variables selected on the day of NGT insertion: Sequential Organ Failure Assessment score (SOFA); mechanical ventilation (MV); tracheostomy; indication for NGT (oral-enteral nutrition, enteral nutrition, enteral-parenteral nutrition); days of ICU stay; ultrasound diagnosis of the position of the NGT; X-ray monitorization, and time until the diagnosis of each imaging modality.
A descriptive analysis of the qualitative variables was performed. These variables were expressed as frequencies and percentages. Quantitative variables were expressed as mean and standard deviation or, for asymmetric distributions, as median and interquartile range (p25–p75). The findings seen on the X-ray were considered the gold standard and used to estimate sensitivity, the positive predictive values (PPV), and the negative predictive values (NPV). The association between the variables (ultrasound diagnosis of the position of the NGT, and X-ray monitorization) was established using Spearman’s correlation coefficient. The Wilcoxon test was used to compare the necessary time to achieve the diagnosis of the position of the NGT using the 2 methods.
P values < .05 were considered statistically significant. The statistical analysis was performed using the statistical software SPSS® v.22.0.
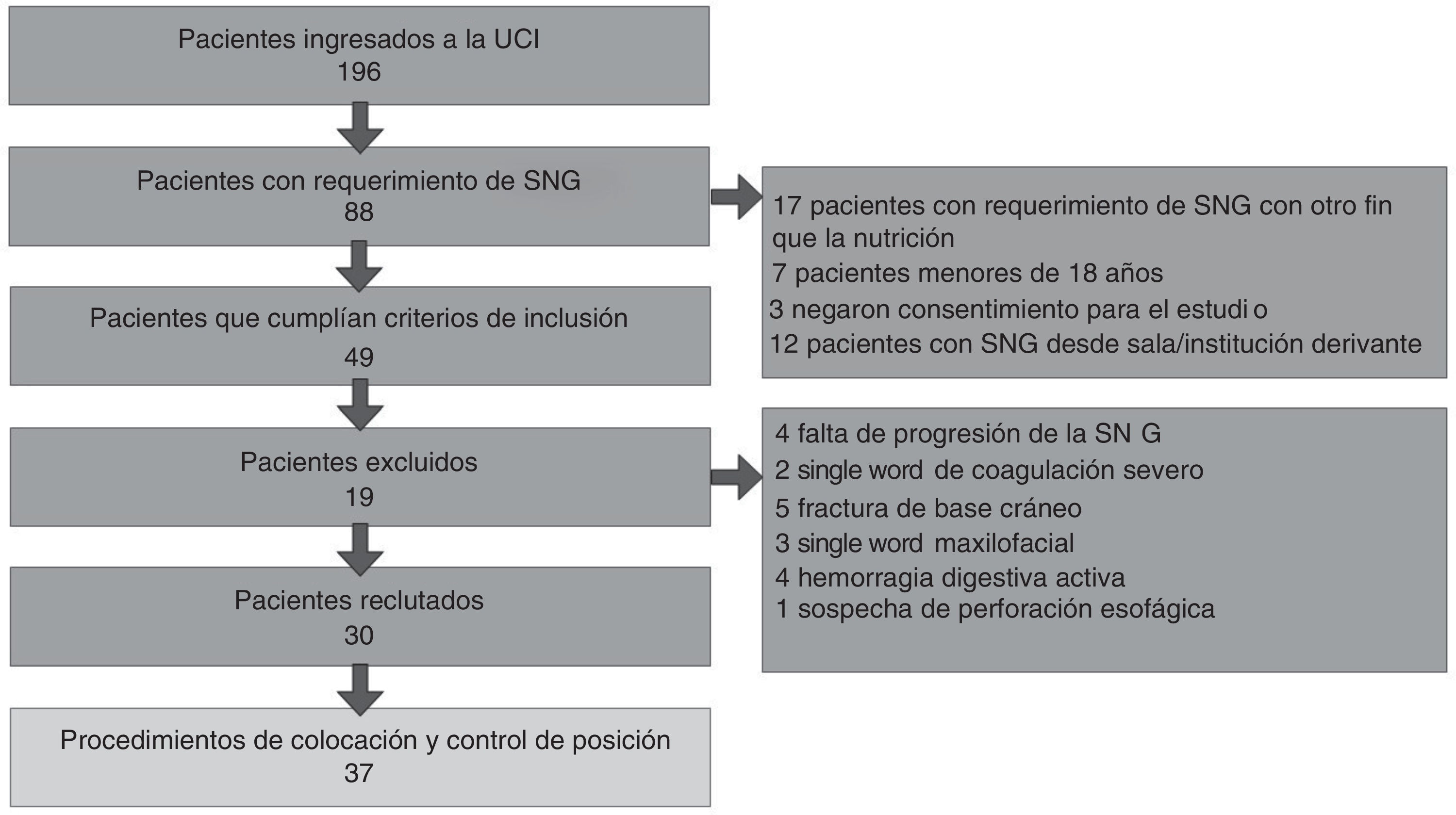
During the 4 months, a total of 196 patients were admitted to the ICU, 88 of whom required NGT insertion. A total of 17 of these patients were excluded because the NGT requirement was different from nutrition (Fig. 2).
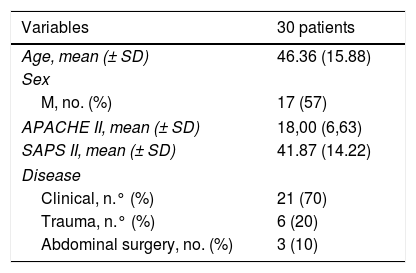
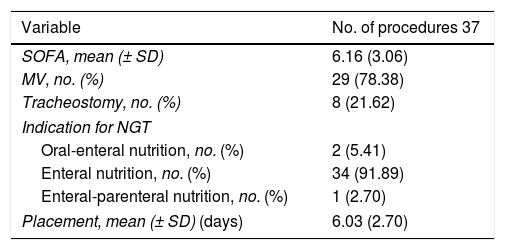
The demographic variables, APACHE II, SAPS II, and disease at ICU admission are shown on Table 1. The details of the variables registered at the moment when the NGT was inserted are shown on Table 2.
Demographic variables, APACHE II, SAPS II, and disease of the patients at the ICU admission.
| Variables | 30 patients |
|---|---|
| Age, mean (± SD) | 46.36 (15.88) |
| Sex | |
| M, no. (%) | 17 (57) |
| APACHE II, mean (± SD) | 18,00 (6,63) |
| SAPS II, mean (± SD) | 41.87 (14.22) |
| Disease | |
| Clinical, n.° (%) | 21 (70) |
| Trauma, n.° (%) | 6 (20) |
| Abdominal surgery, no. (%) | 3 (10) |
APACHE II, Acute Physiology and Chronic Health Evaluation II; F, female; ICU, intensive care unit; M, male; SAPS II, Simplified Acute Physiology Score II; SD, standard deviation.
Value of the variables registered at the time when the NGT was inserted.
| Variable | No. of procedures 37 |
|---|---|
| SOFA, mean (± SD) | 6.16 (3.06) |
| MV, no. (%) | 29 (78.38) |
| Tracheostomy, no. (%) | 8 (21.62) |
| Indication for NGT | |
| Oral-enteral nutrition, no. (%) | 2 (5.41) |
| Enteral nutrition, no. (%) | 34 (91.89) |
| Enteral-parenteral nutrition, no. (%) | 1 (2.70) |
| Placement, mean (± SD) (days) | 6.03 (2.70) |
MV, mechanical ventilation; NGT, nasogastric tube; SD, standard deviation; SOFA, Sequential Organ Failure Assessment score.
The position of the NGT was correct according to the CDU 32 times and according to the X-ray 31 times. In ambiguous cases, the correct placement of the NGT was identified in the lower third of the esophagus through X-ray. The position was considered incorrect according to both imaging modalities on 5 different occasions.
In this study, the sensitivity, PPV, and NPV estimated to achieve diagnosis on the CDU were 100%, 96.9%, and 100%, respectively. Also, a good correlation was found between the CDU and the X-ray (Spearman’s correlation coefficient, Rho, 0.898; P < .001).
With respect to the necessary time to achieve diagnosis of the correct position of the NGT, the median was 10 min (IQR, 9–15) for the DCU, and 90 min (IQR, 30–120) for the X-ray (P < .001).
Other authors have used ultrasound techniques to identify the NGT inside the gastric antrum with good sensitivity.6–9 Kim et al. used the two-dimensional ultrasound to guide the placement of the NGT and see it run down the cervical esophagus finding a 93% sensitivity and a 98% PPV.10 In approximately half of the cases, additional maneuvers were required to make the imaging modality more sensitive, and a high-resolution ultrasound probe was used for a better visualization of the esophagus, but this is something that may not be reproducible in ICUs with fewer resources.
Zatelli and Vezzali studied ultrasound images in multiple windows (including the instillation of fluid) after NGT insertion without CDU guidance, and they reported an 86.4% sensitivity, an 66,7% specificity, and a 97% PPV.6 Our study found higher sensitivity and specificity rates and a similar predictive value despite the lower number of windows. The advantage here is that the time required is shorter, and that the presence of the doctor is not mandatory during NGT insertion, meaning that it can be inserted by another healthcare professional for later checking. In contrast with the aforementioned study, we chose the instillation of air instead of saline solution due to the possibility of iatrogenesis due to an incorrect NGT insertion in the respiratory tract.
As far as we know, there are no studies on the use of CDU for this purpose. These are some of the limitations of our study we should mention: the small sample size, the populations that were not studied: obesity, pregnancy, hiatal hernia, GI surgery postoperative (because no cases in our sample were found), the use of a single ultrasound window, and the indirect visualization of the nasogastric tube. After the results obtained future studies should be conducted. They should compare the CDU to the two-dimensional mode; sensitivity and specificity changes to the combination of other ultrasound windows; and secondary variations to different velocities during bolus administration.
The CDU proved to be a fast, practical, cost-effective, and highly accurate imaging modality to check the position of the NGT in a small group of adult critically ill patients. Although the CDU may be considered the first-line imaging modality for guidance purposes, studies with larger populations are still needed to confirm these findings.
FundingThis study received no funding whatsoever.
Conflicts of interestNone reported.
We wish to thank Dr. Adalberto Baleani, Head of the Imaging Diagnostic Modalities Unit of Hospital Eva Perón.
Please cite this article as: Acosta Pedemonte NB, Bagilet DH, Rocchetti NS, Torresan GV, Rodríguez NA, Settecase CJ. La ecografía doppler color es un método preciso para evaluar la posición de la sonda nasogástrica en pacientes críticos. Med Intensiva. 2021;45:e11–e14.