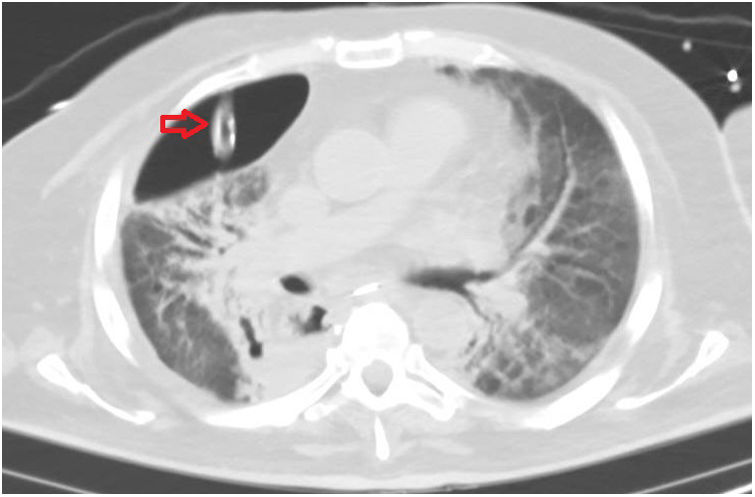
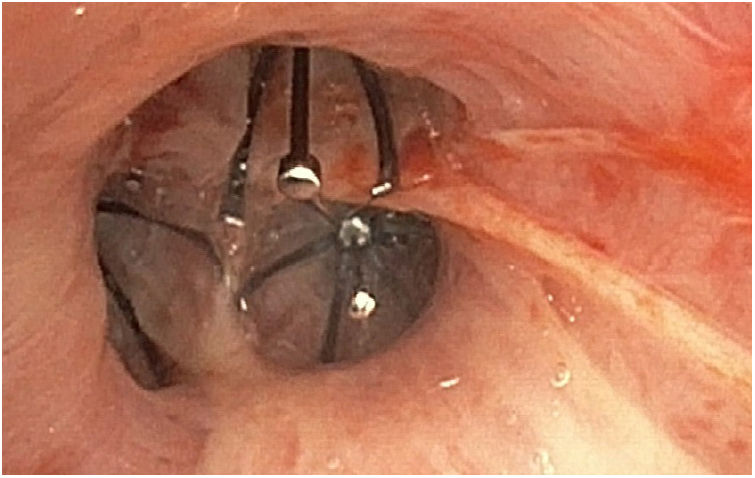
Fifty-four-year-old male with esophageal squamous cell carcinoma who underwent a total transhiatal esophagectomy with cervical esophagogastric anastomosis and right thoracotomy. Thirteen (13) days after the surgery, the patient showed anastomosis dehiscence complicated with refractory hypoxemia due to acute respiratory distress syndrome that required ICU admission and mechanical ventilation support. Due to difficulties weaning from mechanical ventilation, after thirty (30) days the patient developed one right pneumothorax that required chest drain (Fig. 1). Yet despite the use of pressure-controlled ventilation (BIPAP 15cmH2O, without PEEP), there was a persistent continuous pleural effusion, deep sedation, and change to a larger caliber drain with different levels of aspiration. Since weaning from mechanical ventilation was not possible and given the patient's clinical situation, thoracic surgery was ruled out. One fiberoptic bronchoscopy was performed with one occlusion balloon catheter that confirmed the presence of pleural effusion associated with the right upper lobe of the lung that led to an endobronchial occlusion procedure with valves in the three (3) bronchi of such lobe (Fig. 2). Eventually, this intervention allowed weaning from mechanical ventilation and removing the chest tube.
FundingThe authors received no funding whatsoever while conducting this study.
Please cite this article as: Tejero Aranguren J, Ruiz Ferrón F, Colmenero Ruiz M. Tratamiento endobronquial de neumotórax persistente en síndrome de dificultad respiratoria aguda. Med Intensiva. 2019;43:516.