Major injury is the sixth leading cause of death worldwide. Among those under 35 years of age, it is the leading cause of death and disability. Traffic accidents alone are the main cause, fundamentally in low- and middle-income countries.
Patients over 65 years of age are an increasingly affected group. For similar levels of injury, these patients have twice the mortality rate of young individuals, due to the existence of important comorbidities and associated treatments, and are more likely to die of medical complications late during hospital admission.
No worldwide, standardized definitions exist for documenting, reporting and comparing data on severely injured trauma patients. The most common trauma scores are the Abbreviated Injury Scale (AIS), the Injury Severity Score (ISS) and the Trauma and Injury Severity Score (TRISS).
Documenting the burden of injury also requires evaluation of the impact of post-trauma impairments, disabilities and handicaps. Trauma epidemiology helps define health service and research priorities, contributes to identify disadvantaged groups, and also facilitates the elaboration of comparable measures for outcome predictions.
El trauma grave es la sexta causa de muerte y la quinta de discapacidad en el mundo. En los menores de 35 años es la primera causa de muerte y discapacidad. Los accidentes de tráfico son los principales responsables en los países de ingresos medios-bajos, que son los más poblados.
Los pacientes mayores de 65 años son una cohorte creciente. Para niveles lesionales similares tienen el doble de mortalidad que los jóvenes, debido a su elevada comorbilidad y los tratamientos asociados.
No existen globalmente definiciones estandarizadas para documentar, informar y comparar datos en los traumatizados graves. Los más utilizados son el Abbreviated Injury Scale (AIS), el Injury Severity Score (ISS) y el Trauma and Injury Severity score (TRISS).
Las herramientas para la evaluación de la discapacidad postraumática deben mejorarse. Los estudios epidemiológicos son fundamentales para evaluar el impacto en la salud pública, mejorar las estrategias preventivas y evaluar las terapéuticas.
Severe or major trauma is a worldwide pandemic and one of the leading causes of death and disability. Its distribution at global, national and local level differs, however. Trauma is very heterogeneous in terms of its underlying causes, the types of injuries and their severity, and is characterized by considerable prognostic uncertainty. The risk factors of trauma are related to human behavior and to sociosanitary, occupational, economic, political and cultural variables. Its management in turn depends on a broad range of structures, organizations and clinical and surgical specialties. Lessening the burden of trauma disease is a complex task requiring a multidiscipline approach and great insistence in order to prevent it from continuing to be viewed as the “unattended epidemic”.1
Estimation of the global burden of disease in the world is an arduous and difficult task, and constitutes a stimulating scientific challenge and an urgent moral obligation. The Global Burden of Disease Study (GBD) 2010, auspiced by the World Health Organization (WHO), represents the most important systematic initiative to date for knowing the global distribution of the most prevalent diseases and traumatisms, as well as the risk factors for health.2 Despite logical doubts regarding the validity, reliability, transparency and plausibility of its estimations, the GBD is a solid epidemiological information source.3
In addition to mortality data, the GBD informs of the nonfatal sequelae (disabilities and handicaps) for the survivors–this being particularly useful in trauma patients, who are often healthy young individuals that suffer lifelong disabilities as a result of trauma. The study measures the burden of disease in terms of disability-adjusted life years (DALYs),4,5 a parameter that combines the life years lost as a result of premature death (years of life lost [YLLs]) with the life years of disability (years of life with disabilities [YLDs]). In this regard, DALY represents the difference between current life status and that of an ideal population living to an old age and free of diseases and disabilities.
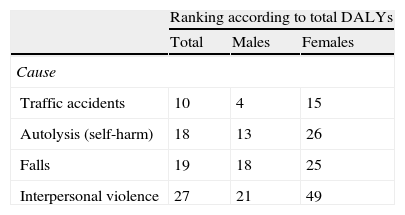
Global dataAccording to the GBD, in the year 20102,6 the global burden of disease was 2490 million DALYs (361/1000 inhabitants), of which traumatisms accounted for 278.6 million (11.2%). In turn, 29% of these injuries corresponded to traffic accidents, 12.6% to falls and 9.16% to interpersonal violence. Traffic accidents generate 3% of the global DALYs. Interpersonal violence is the leading cause of DALY in Central America–The Caribbean and in Sub-Saharan Africa.6 Globally, DALYs due to suicide are equivalent to one-half of those attributable to traffic accidents,2 with great variability between countries. Table 1 describes the global ranking (in terms of the number of DALYs) of the different causes of trauma contemplated by the GBD, distributed according to gender. In this regard, among males, traffic accidents are seen to rank in fourth position.
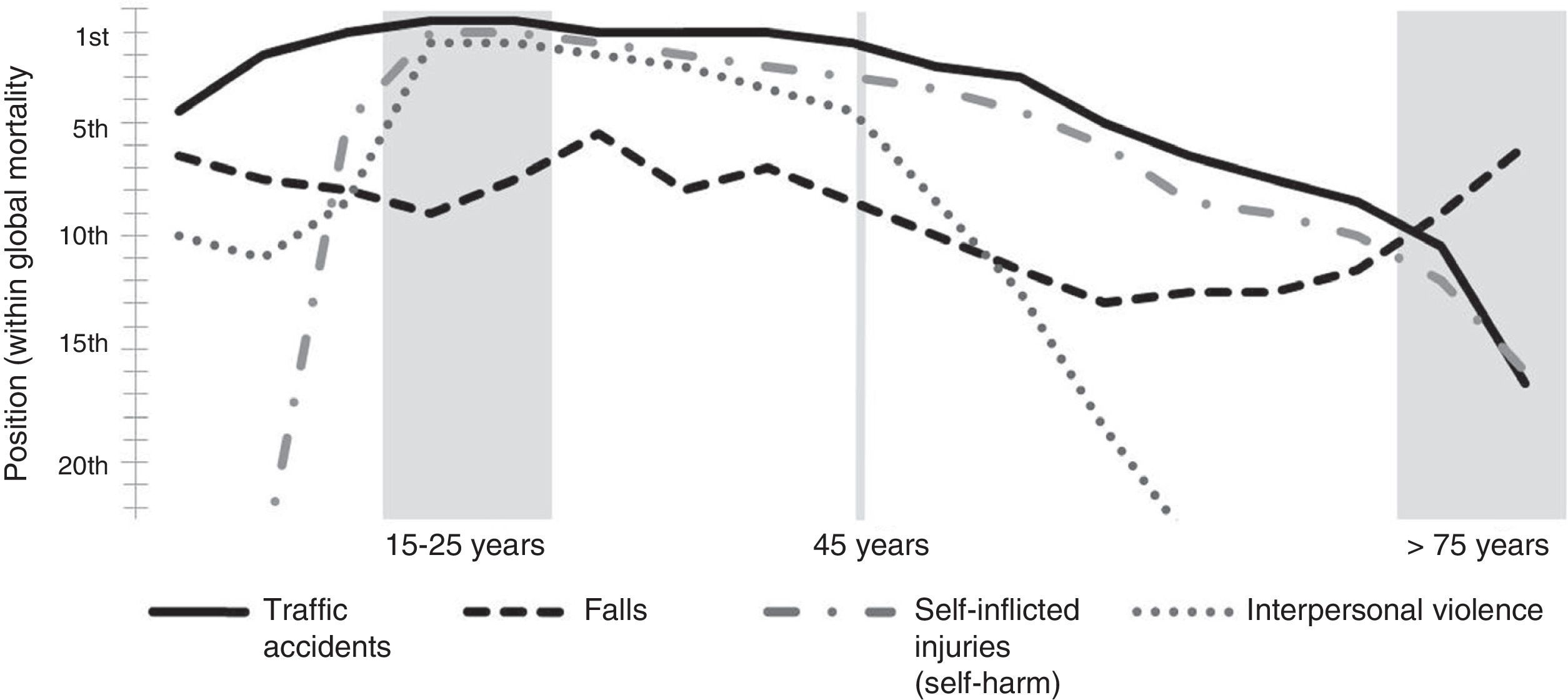
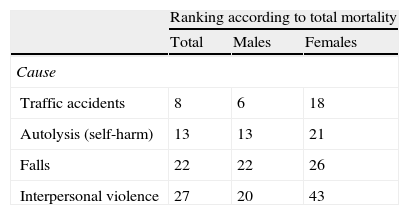
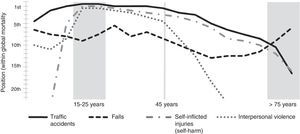
Regarding mortality, trauma globally is the sixth leading cause of death and the fifth ranking cause of moderate and severe disability. One out of every 10 deaths is a result of trauma in both sexes. In those under 35 years of age, it is the first cause of death and disability.6Table 2 shows the ranking of the different types of trauma as a cause of mortality. Among males, traffic accidents are seen to rank in sixth place. Fig. 1 relates the different age intervals and causes of trauma. In this regard, between 25 and 35 years of age, traffic accidents, violence and self-inflicted injuries (self-harm) occupy the leading positions among all causes of mortality. After the age of 45 years the figures decrease, and accidental falls gradually become more important–representing the predominant type of trauma after 75 years of age. Except in areas of conflict and in certain urban epidemic zones, e.g., in the United States (20–45%) or South Africa (up to 60%), penetrating traumatisms represent a small proportion (less than 15%).
Deaths due to trauma and the causes according to GBDa. Ranking with respect to global mortality.
| Ranking according to total mortality | |||
| Total | Males | Females | |
| Cause | |||
| Traffic accidents | 8 | 6 | 18 |
| Autolysis (self-harm) | 13 | 13 | 21 |
| Falls | 22 | 22 | 26 |
| Interpersonal violence | 27 | 20 | 43 |
Traumatisms are more frequent and are progressively increasing in middle- to low-income countries,7–9 which account for 90% of the world population, since these are regions characterized by chaotic industrialization, a dramatic rise in the number of motor vehicles, and frequent armed conflicts. Furthermore, in such countries the effects of the injuries are more serious, since their public health systems are still largely underdeveloped. These countries contribute 90% of the overall fatalities, with an enormous impact in terms of disability.
In Spain, the National Statistics Institute (INE)10 registered the death of 402,950 people in the year 2012. According to the distribution by chapters of the International Classification of Diseases (ICD-9-CM),11 deaths due to external causes totaled 14,005 (3.5% of the total), and represented the leading cause of mortality among individuals between 15 and 39 years of age (15.4/100,000 individuals). The number of deaths due to suicide (3532) was greater than that attributable to traffic accidents (1915).
Age and severe traumaThe aging of the population is generating a new and growing cohort of elderly trauma patients with a high prevalence of comorbidities12 that moreover require treatments such as antiplatelet drugs and anticoagulants, which logically complicate the evolution of trauma by increasing the risk of bleeding. In this respect, it should be noted that 5–15% of all subjects over 80 years of age suffer atrial fibrillation, which is generally treated with drugs of this kind.
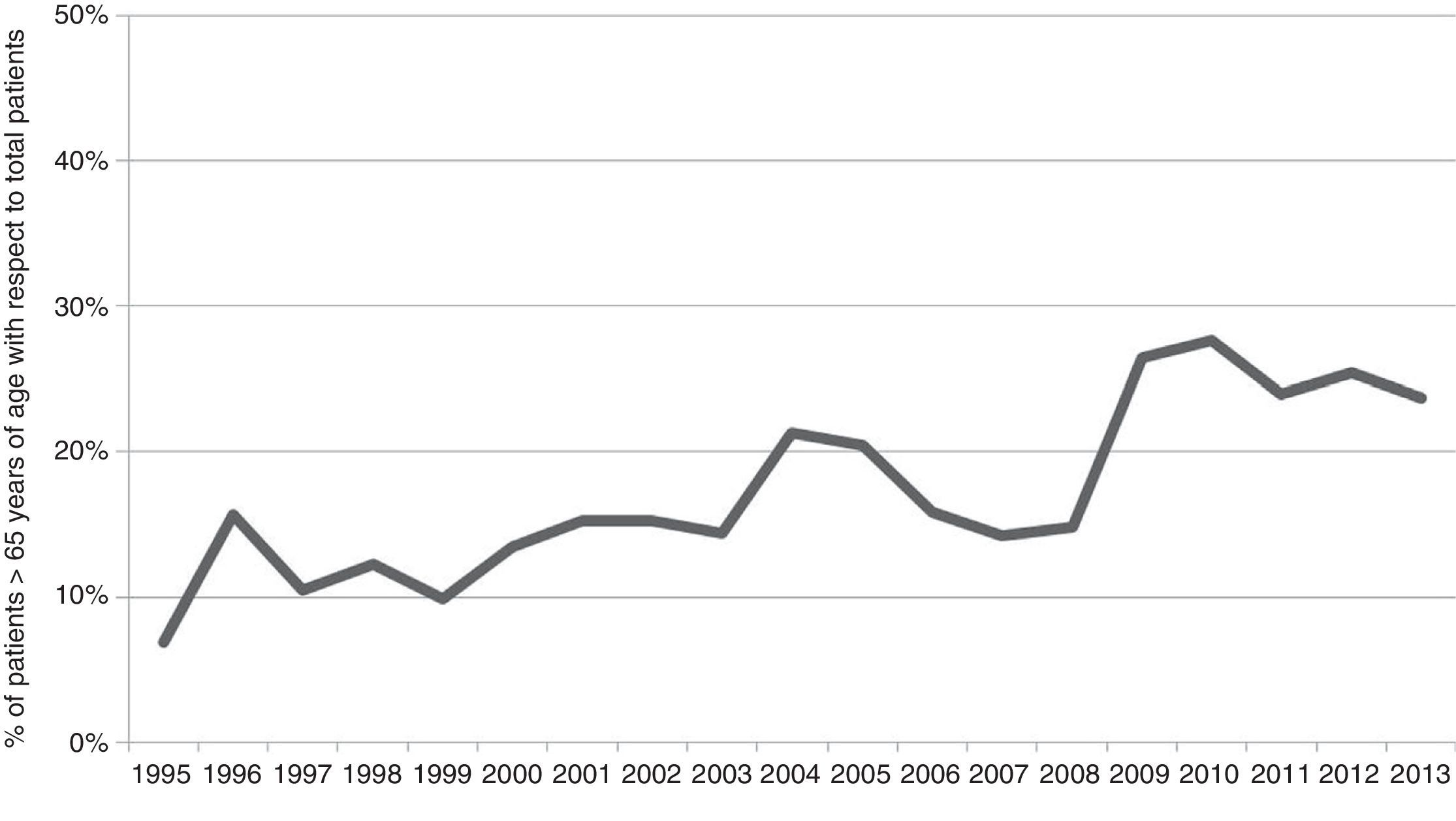
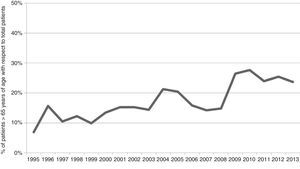
The literature usually tends to define old age in trauma as corresponding to 65 years of age. The population beyond this age currently accounts for up to 23% of all admissions due to severe trauma. Fig. 2 shows the gradual increase over the last 18 years in the number of patients over age 65 (Poliguitania registry).13 Trauma is the fifth leading cause of death in this population. Falls are responsible for 75% of the cases, and are attributable to multiple factors associated to aging, such as hearing problems, poor vision, instability, slow reactions, cognitive impairment and previous disabilities. The remaining 25% are related to traffic accidents. Penetrating traumatisms practically disappear in this population group.14
Primary injury assessment in elderly trauma patients is often deficient, and this leads to underdiagnosis. Among other reasons, such incorrect evaluation is due to the apparent trivial nature of the causal mechanisms, such as seemingly unimportant falls, the frequent comorbid conditions which result in anomalous cardiovascular responses, chronic treatment with beta-blockers, or the presence of a pacemaker.15
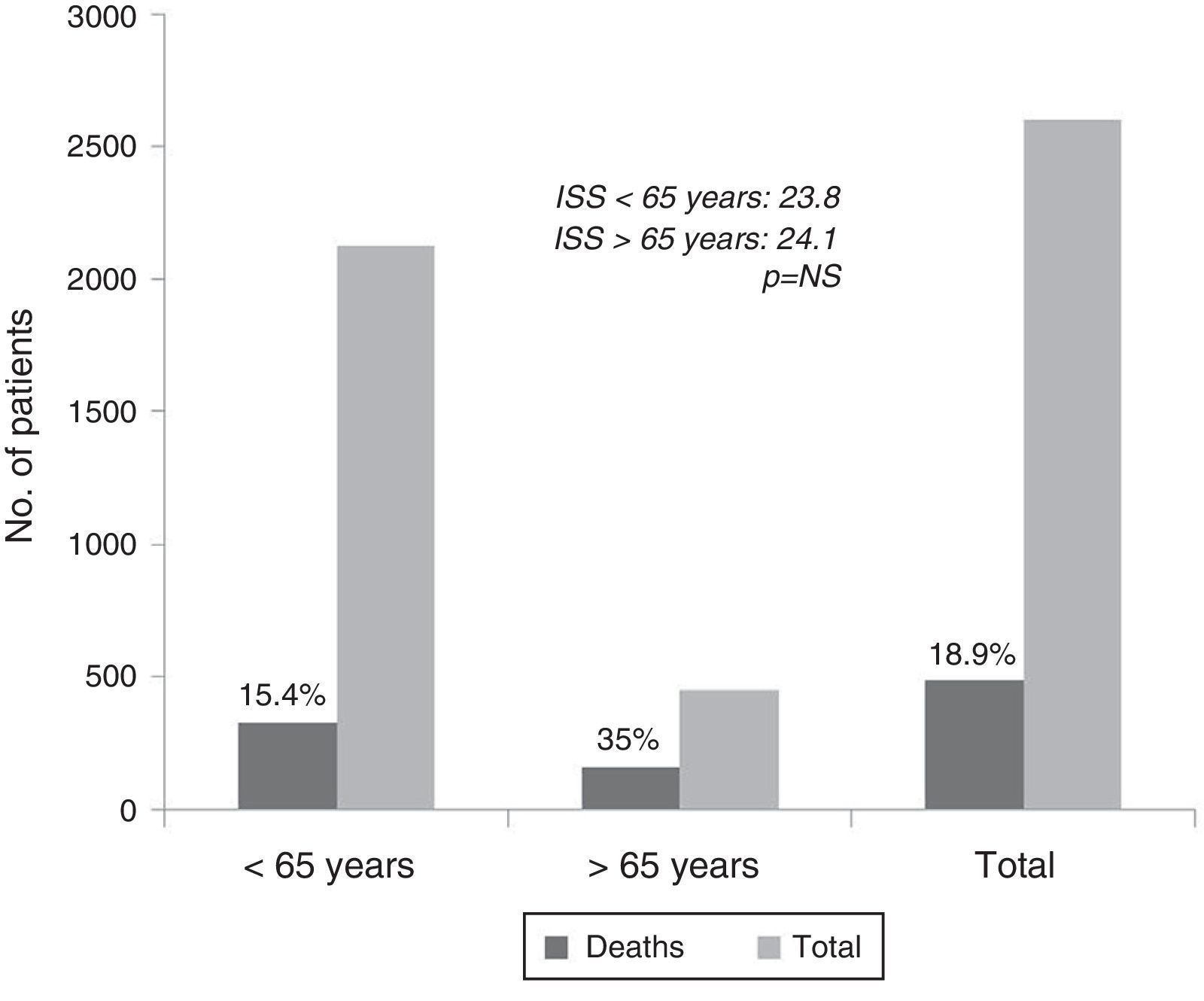
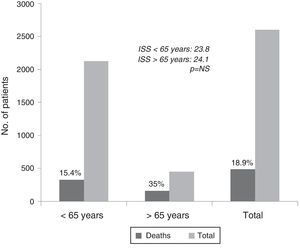
For similar levels of injury, elderly patients have twice the mortality rate and greater morbidity compared with young individuals. Fig. 3, with data on 2602 patients of the Poliguitania registry, shows the 35% mortality rate in the elderly to strongly contrast with the 15% mortality rate found in individuals under 65 years of age, particularly when considering that both groups presented the same degree of severity.13 Another observation of note is the fact that 19% of all the deceased subjects were taking acenocoumarol (Sintrom®) and/or antiplatelet drugs, and all of them were over 74 years of age. The explanations are an increased mortality rate due to bleeding complications in the acute phase, especially in traumatic brain injury (TBI) cases, and greater late mortality due to the appearance of late clinical complications such as sepsis and multiorgan failure (MOF).16 Consequently, elderly trauma patients require different screening, evaluation and treatment protocols than those used in younger individuals.
Etiology of trauma. Principal causes- -
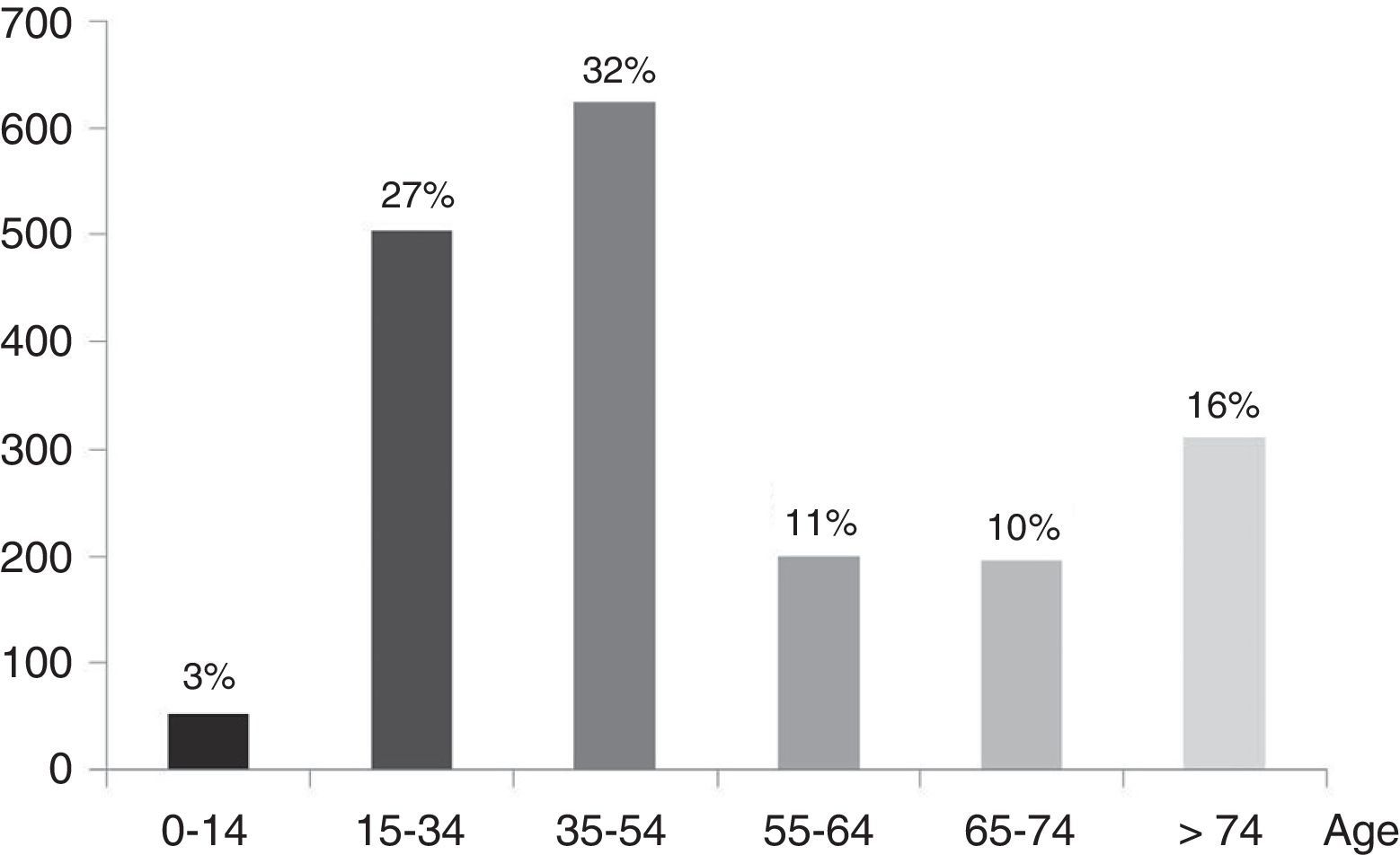
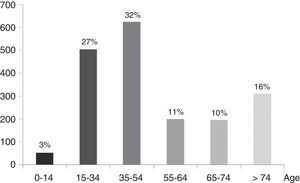
Traffic accidents: these are the cause of 35% of all global trauma fatalities (cars, industrial vehicles, motorcycles or bicycles, pedestrians), with 1.3 million deaths and 45 million disability cases each year. While the statistics are increasing in developing countries, the adoption of preventive strategies and the availability of adequate treatment have caused the figures to decrease in the developed countries.9 According to data of the INE,10 in the year 2012 a total of 1915 people died in Spain in traffic accidents (9.5% less than in the preceding year 2011). Such accidents represented 17.5% of all deaths in individuals between 15 and 24 years of age, 15% of all deaths between 25 and 34 years of age, and 9.85% of all deaths in people between 35–44 years of age. According to data from the Spanish traffic authorities (DGT),17 over one-half of the deaths correspond to the 15–54 years age interval (Fig. 4)–car accidents being responsible for the largest number of fatalities (Table 3).
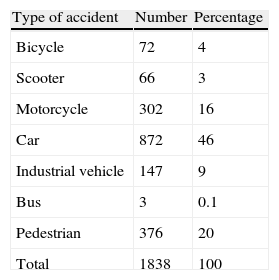
Table 3.Number of deaths due to traffic accidents in Spain during 2012. Distribution according to type of accident.
Type of accident Number Percentage Bicycle 72 4 Scooter 66 3 Motorcycle 302 16 Car 872 46 Industrial vehicle 147 9 Bus 3 0.1 Pedestrian 376 20 Total 1838 100 Data from the Spanish traffic authorities (DGT).
- -
Falls: these are the cause of up to 40% of all trauma cases,18 and increase in frequency with advancing age, reaching a peak toward 75 years of age.
Although the distribution of injuries is variable, the patterns or trends reflected by different national registries (GITAN,19 RETRATO,20 ETNA,21 POLIGUITANIA13) point to a predominance of severe head injuries (33–47%), followed by chest injuries (18–35%), trauma of the extremities (15–26%) and abdominal trauma (8–17%), as well as a number of more variable combinations of injured territories.
Head injuries are the prevalent presentation, with greater morbidity–mortality and more serious and lasting sequelae. Each year in the United States there are 1.7 million such injuries, of which 1.4 million are attended in Emergency Departments, with 275,000 hospital admissions and 52,000 deaths.22 In Europe, the mean annual incidence of head injuries is 235/100,000 inhabitants. In a systematic review of 23 European studies,23 the mean incidence varied between 20 and 536 per 100,000 inhabitants. This broad range is due to the different inclusion criteria used by the registries, the different definitions of severity–with the underestimation of some that are classified as mild or moderate–and the lack of high quality epidemiological data.24 In middle- and low-income countries, TBI is more frequent among younger individuals.25 In higher income countries the age of the affected individuals is greater, thanks to the adopted traffic safety measures that have lowered the accident rates among young people and the increase observed among elderly people is due to their improved life expectancy, greater mobility and increased comorbidity. The economic differences between and within countries also have an impact upon morbidity–mortality.26
Morbidity–mortality in TBI is conditioned to the use of modern treatments provided by coordinated multidisciplinary teams. Different clinical trials have demonstrated improvements in patient outcome. However, from the global epidemiological perspective, the situation has fluctuated over the years. In a metaanalysis of the last 150 years,27 the mortality rate was found to have decreased 50%, though in the period 1930–1970 the statistics did not improve, due to the increase in number of motor vehicles. In the following period 1970–1990, mortality decreased substantially thanks to the introduction of computed axial tomography (CAT) and improvements in intensive care. Finally, after 1990 the mortality rate has not decreased any further–in part because the patients who suffer TBI are now comparatively older, with greater comorbidities and with treatments involving antiplatelet drugs and anticoagulants. Another recent metaanalysis28 covering the period 1980–2011 has drawn similar conclusions.
Epidemiology of trauma mortalityThe two leading causes of mortality are neurological injuries and bleeding. Specifically, hemorrhage is responsible for 80% of all deaths that occur within the first few hours.29
In general, since the different registries are referred to patients that have been admitted to hospital centers, they fail to take into account that “in situ” mortality or death occurring during initial transport to hospital is by far the most frequent situation. A number of studies estimate that 38.5–55% of all deaths occur under such circumstances.30–32
Of the patients that die in hospital, 55% do so within the first 24h, with a higher Injury Severity Score (ISS) and a greater frequency of transfusions. Head injuries are the most common type of injury among those that die between the first and sixth day in hospital. Those that die after 7 days are 10 years older and have an ISS score 17 points lower than those who die on the first day of admission, and up to 60% of all deaths in such cases are attributable to complications such as sepsis and MOF.33,34 Elderly patients receiving antiplatelet drugs and anticoagulants are an important source of mortality due to mild falls with serious bleeding complications. Over the last decade there has been a decrease in mortality due to bleeding,35 resulting from the introduction of damage control strategies, improvements in diagnosis (especially angioCAT), and greater implication on the part of interventional radiology.
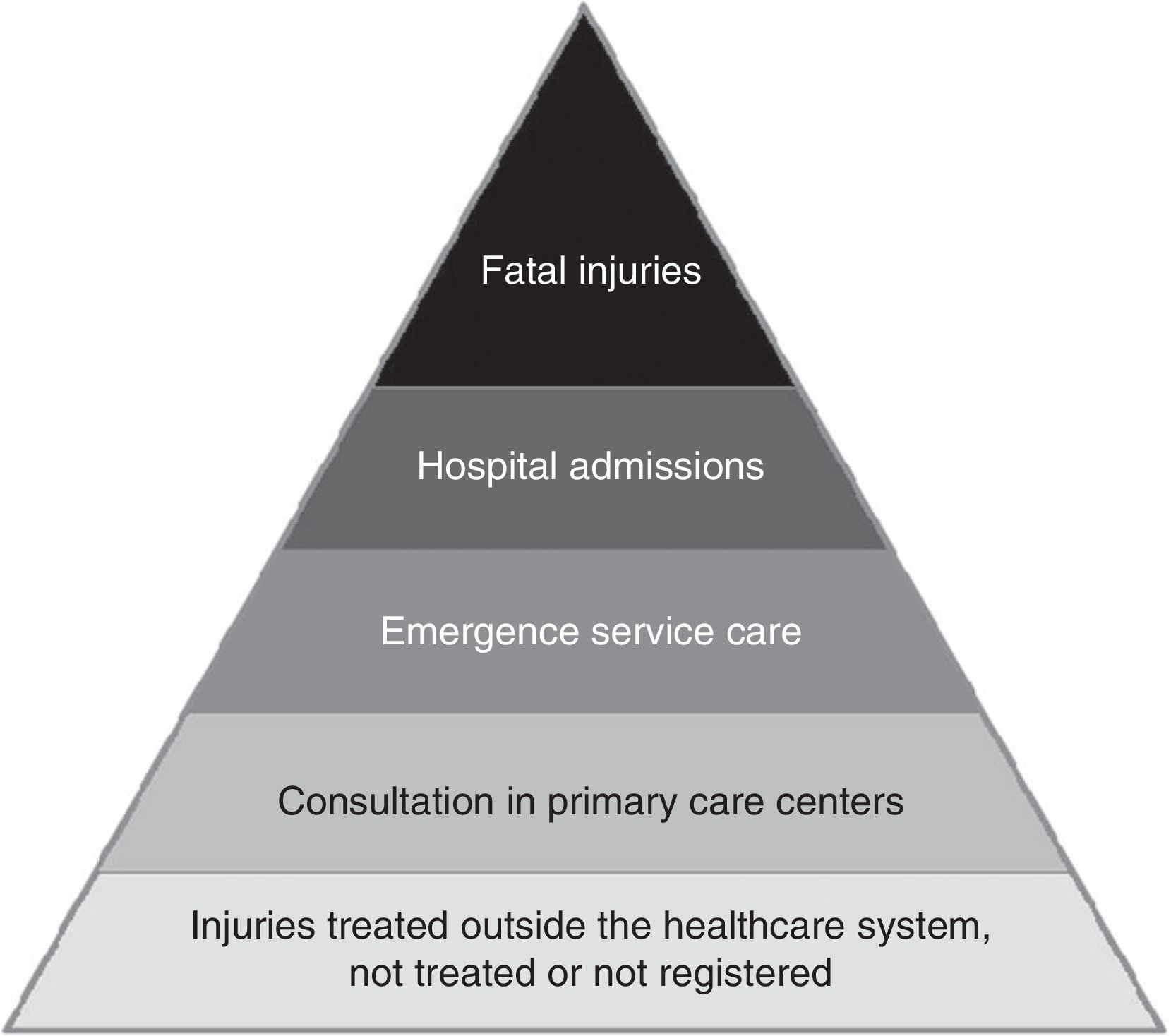
Epidemiology of disability: the disease burden of nonfatal traumatismsQuantification of the “disease burden” posed by trauma must include injuries ranging from mild to fatal, since fatalities represent only the tip of a pyramid, with a proportion of one death for every 10 hospital discharges and 190 visits to the Emergency Department. The relative number of fatal and nonfatal injuries, and their trajectory within the healthcare system, has been graphically depicted in the form of a pyramid (Fig. 5) that can be generated for different age ranges, different etiologies and major injury groups.
In addition to the above, it is important to mention the enormous long-term impact of the sequelae of nonfatal traumatisms for both the patients and their families. The most serious and lasting consequences are attributable to TBI. About 5.3 million patients in the United States36 and 7.7 million in Europe23 live with serious neurocognitive and psychosocial sequelae. Furthermore, these sequelae do not manifest only as disabilities among individuals with serious TBI, but also as a significant decrease in life expectancy37 and an acceleration of the cognitive deterioration inherent to aging–with earlier onset and faster progression of Alzheimer's disease among those who are genetically susceptible to the disorder.38
This long-term impact is very important in patients admitted to the Intensive Care Unit (ICU), since these are severe trauma cases. The functional alterations caused by the injuries are responsible for the disabilities manifesting as variable degree handicaps that often have a permanent impact upon patient's quality of life. The measurement of these effects is crucial. However, the injury scores commonly used in the ICU are only referred to mortality risk or to resource utilization, and do not inform about the long-term sequelae for the patients and their sociosanitary environment.
One of the ways to evaluate this issue has been to simply use the associated costs as a measurement instrument. However, a more useful approach is to use quality of life scales that evaluate and rate the sequelae. Such scales are gaining the recognition they deserve, because they are of help in developing strategies that reduce the disease burden of trauma. The most widely used approaches involve measurement of the limitations in activities of daily living, and which are used in application to a broad range of diseases. Other scales are more specifically targeted to trauma, and integrate within a single score patient mortality, changes in longevity, disability, functionality, pain and cognitive and emotional alterations with an impact upon quality of life. Mention will be made here of only some of them, such as the Quality of Well Being,39 the Health Utilities Index,40 Functional Capacity Index,41 and the Short-Form Health Survey.42 These scales were developed for individual or population-based application. Disability-adjusted life years (DALYs),3–5 commented at the start of this article, are intended for population-based application, and are more specifically oriented toward the efforts made by the WHO in defining the Global Burden of Disease (GBD). The fact that DALYs are advocated by the WHO has facilitated their introduction in teaching and research circles.
The important number of existing scales, in addition to those already described, reflects a lack of consensus regarding their use–a situation that results from the diversity of objectives and shortcomings in terms of reliability.
Tools for studying the epidemiology of trauma: traumatisms in Intensive Care UnitsThe estimations referred to the epidemiology of trauma43 are basically obtained from two sources: (a) data collected by the administrations, such as death certificates, mortality statistics, legal registries or hospital discharge reports; and (b) specialized registries compiled by the healthcare professionals involved in caring for these patients and which in general contribute information of greater quality and applicability.44
All these sources produce a valid and important volume of information. However, there are certain shortcomings in terms of the robustness of the estimates, mainly due to two reasons. On one hand, they do not cover all of the relevant population, since many countries do not conduct systematic documentation of the epidemiology of trauma. On the other hand, there are significant differences between trauma registries, with no globally accepted and standardized definitions for documenting, reporting and comparing data referred to severe trauma cases. As an example, consensus is lacking in aspects as basic as the definition of severe or major trauma. This is because different taxonomic systems are used in application to trauma, and even when the same system is employed, different defining cutoff points are used. There have been cooperative efforts to establish homogenization (Utstein),45 though no general consensuses have been established to date.
Improving information on the prevalence and incidence, and on the different injury and activity variables of severe trauma remains a priority concern at local, national and global level.
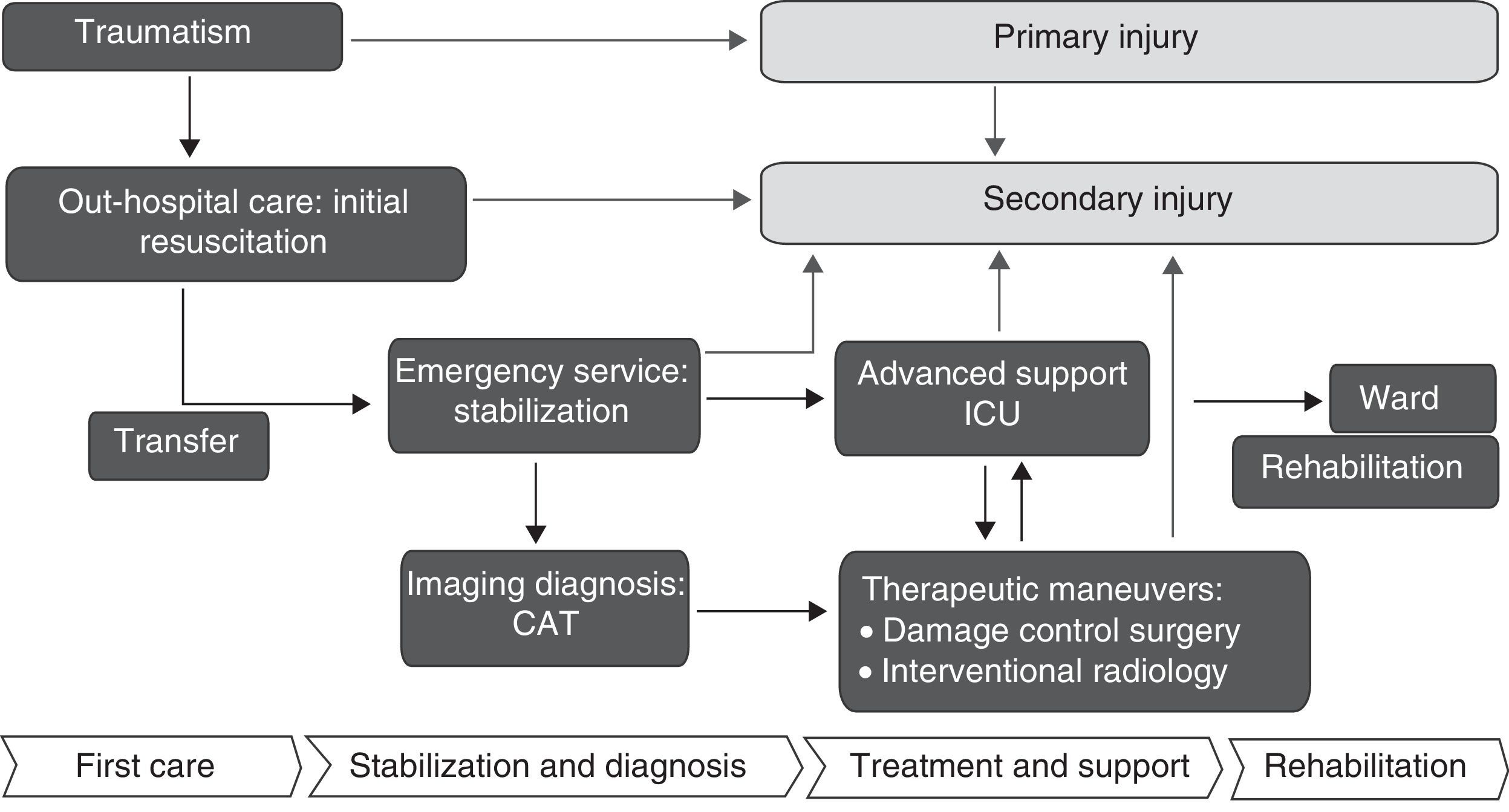
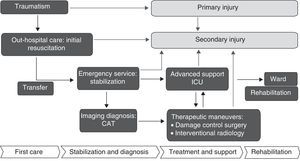
The conceptual setting for the epidemiological study of trauma should evaluate the physical and functional dimensions described in Fig. 6, with a study of the structures, injuries and activities characterizing the entire care process, and adopting a multidisciplinary and coordinated approach. Among the most important registries, mention should be made of the National Trauma Data Bank (NTDB)18,46 in the United States, the Trauma Audit Research Network (TARN)47 in the United Kingdom, the Registry of the German Society of Trauma Surgery (TR-DGU),48 and the European EUROTARN registry.49 In Spain there have been several provincial or regional registries with variable degrees of development and continuity, such as the GITAN,19 RETRATO,20 ETNA,21 and POLIGUITANIA registries.13 A very recent introduction has been the Spanish national severe trauma registry (RETRAUCI),50 under the auspices of the SEMICYUC.
Taxonomy of injuriesMany classifications can be found in the literature, though the present review will focus on the most widely used systems.
The most widely used classifications comprise the trauma injury descriptions of the ICD-9-CM and the Abbreviated Injury Scale (AIS):
- 1.
International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes (800-959.9): The ICD has the advantage of using diagnoses routinely used in hospitals, with coding by the administration. This coding system has been used to develop the survival-predicting International Classification of Disease-9 based Injury Severity Score (ICISS),51 subsequently improved upon through the incorporation of new indices, though consensus regarding its use has not been reached. From 1 October 2014, the current ICD-9 codes become obsolete and will be replaced by the newly updated tenth edition of the classification (ICD-10-CM).
- 2.
Abbreviated Injury Scale (AIS):52 The AIS is the most widely accepted instrument. It comprises a dictionary with over 2000 entries describing each injury with a 6-digit number to which a rating of severity is added on a scale of 1–6 (1=minor and 6=fatal). The system was introduced in 1969, and since then has been revised and updated on several occasions (1995, 1998, 2005, 2008). The use of the different versions of the dictionary in long-duration registries covering periods that include the successive updates affects evaluation of the severity of the injuries–a fact that may affect description and comparability.53 The Injury Severity Score (ISS)54 determines the severity of the patient, and is calculated from the three most serious injuries of different body regions raised to the square and summed. After more than 20 years in use, a simple modification was proposed, known as the New Injury Severity Score (NISS),55 which significantly improves upon the predictive capacity of the previous ISS. It is based on the selection of the coded three most serious injuries, even if within one same AIS territory–in contrast to the ISS, which only selects the most serious injury of the three different most seriously affected territories, and therefore underestimates severity in some cases. The AIS reflects the threat to life represented by each injury, whereas the ISS reflects the threat to life for each patient according to the multiplicity of injuries. The pre-hospital period is analyzed by the physiological Revised Trauma Score (RTSp),56 which affords a weighted grouping of respiratory frequency, systolic blood pressure and the Glasgow Coma Score (GCS). The Trauma and Injury Severity Score (TRISS)57 in turn predicts survival and is based on the ISS, the RTS, patient age, and the blunt (contusional) or penetrating mechanism of injury involved. It uses coefficients derived from the Major Trauma Outcome Study (MTOS),58 fundamented on a large trauma database in the United States. For over 20 years it has been the reference for the description and comparison of trauma care centers. The use of this instrument is currently subject to controversy because of its age, considering the improvements there have been in the diagnostic and therapeutic procedures over the years. Indeed, both the German (DGU) and the British registries (TARN) have developed their own predictive models.
The consideration of accidental trauma as something unavoidable that happens by chance is incorrect. The excellent results obtained in the prevention of traffic accidents in Spain, and the reduction of accidents at work through the adoption of occupational risk prevention regulations are clear evidence of this.
Epidemiology is an effective tool for evaluating changes in morbidity–mortality, helping us to improve preventive strategies, detect risk groups, improve the quality of clinical practice guides, and favor coordination among the implicated teams. We moreover consider that the ethical dimension of the health indices should not be overlooked. Each country individually must decide the most feasible steps and with the greatest impact.59
Epidemiology contributes to the reduction of morbidity–mortality in a number of ways:
- -
Determination of the burden of disease with a view to planning the necessary services and prioritizing resource assignment. Identification of risk factors and risk groups. Integration of disabilities.
- -
Control and prevention of disease through the primary prevention of accident risk (behavioral changes, informative and legal campaigns against alcohol and drugs, control of firearms, strategies for the prevention of falls in the elderly, speed limits) and secondary prevention measures (to lessen the severity of the injuries caused by accidents, based on the use of different systems: safety belts, helmets, the use of non-inflammable materials, etc.).
- -
Improvement of injury coding and unification of the definitions used: development of prognostic indices.
- -
Help in the creation of hospital, local and regional trauma commissions, supporting the implementation of “Trauma Systems” requiring the creation and maintenance of a registry as a basic tool for correct functioning.
The authors declare that they have no conflicts of interest.
The authors thank the personnel of the Department of Intensive Care Medicine of Donostia University Hospital for their collaboration in this study.
Please cite this article as: Alberdi F, García I, Atutxa L, Zabarte M, Grupo de Trabajo de Trauma y Neurointensivismo de SEMICYUC. Epidemiología del trauma grave. Med Intensiva. 2014;38:580–588.