To describe the characteristics and management of severe trauma disease in Spanish Intensive Care Units (ICUs). Registry of trauma in the ICU (RETRAUCI). Pilot phase.
DesignA prospective, multicenter registry.
SettingThirteen Spanish ICUs.
PatientsPatients with trauma disease admitted to the ICU.
InterventionsNone.
Main variables of interestEpidemiology, out-of-hospital attention, registry of injuries, resources utilization, complications and outcome were evaluated.
ResultsPatients, n=2242. Mean age 47.1±19.02 years. Males 79%. Blunt trauma 93.9%. Injury Severity Score 22.2±12.1, Revised Trauma Score 6.7±1.6. Non-intentional in 84.4% of the cases. The most common causes of trauma were traffic accidents followed by pedestrian and high-energy falls. Up to 12.4% were taking antiplatelet medication or anticoagulants. Almost 28% had a suspected or confirmed toxic influence in trauma. Up to 31.5% required an out-of-hospital artificial airway. The time from trauma to ICU admission was 4.7±5.3h. At ICU admission, 68.5% were hemodynamically stable. Brain and chest injuries predominated. A large number of complications were documented. Mechanical ventilation was used in 69.5% of the patients (mean 8.2±9.9 days), of which 24.9% finally required a tracheostomy. The median duration of stay in the ICU and in hospital was 5 (range 3–13) and 9 (5–19) days, respectively. The ICU mortality rate was 12.3%, while the in-hospital mortality rate was 16.0%.
ConclusionsThe pilot phase of the RETRAUCI offers a first impression of the epidemiology and management of trauma disease in Spanish ICUs.
Describir las características de la enfermedad traumática grave (ETG) y su atención en las unidades de cuidados intensivos (UCI) españolas.
DiseñoRegistro multicéntrico y prospectivo.
ÁmbitoTrece UCI españolas.
PacientesPacientes con ETG ingresados en UCI participantes.
IntervencionesNinguna.
Variables de interés principalesAspectos epidemiológicos, atención prehospitalaria, registro de lesiones, consumo de recursos, complicaciones y evolución final.
ResultadosSe incluyó a 2.242 pacientes con 47,1±19,02 años de edad media, 79% hombres. Fue trauma contuso en 93,9%. El Injury Severity Score fue de 22,2±12,1 y el Revised Trauma Score de 6,7±1,6. Fue no intencionado en el 84,4%. Las causas más frecuentes fueron accidentes de tráfico, caídas y precipitaciones. Un 12,4% tomaban antiagregantes o anticoagulantes y en casi un 28% se implicó el consumo de tóxicos. Un 31,5% precisaron una vía aérea artificial en medio prehospitalario. El tiempo medio hasta el ingreso en UCI fue de 4,7±5,3h. Al ingreso en UCI un 68,5% se encontraba estable hemodinámicamente. Predominó el traumatismo craneal y torácico. Hubo un importante número de complicaciones y en el 69,5% de los casos necesidad de ventilación mecánica (media 8,2±9,9 días). De ellos, un 24,9% precisaron traqueotomía. Las estancias en UCI y hospitalarias fueron respectivamente de mediana 5 (3–13) días y 9 (5–19) días. La mortalidad en UCI fue del 12,3% y la hospitalaria del 16%.
ConclusionesLa fase piloto del RETRAUCI muestra una imagen inicial de la epidemiología y atención del paciente con ETG ingresado en las UCI de nuestro país.
Severe trauma disease (STD) is a worldwide pandemic and one of the leading causes of death and disability, particularly in young adults.1 The prognosis of STD depends on a number of factors, such as the severity and energy of trauma, the physiological reserve of the patient, and the quality and promptness of the provided care. The latter are the modifiable factors.2 However, modification is only feasible if the reality of healthcare is adequately monitored, and this inevitably implies the existence a trauma registry (TR).2,3
Trauma registries can fully monitor the STD care process, and among other aspects their advantages include the monitoring of epidemiological trends, the promotion of public health and scientific production, the designing of individualized intervention plans, and the optimization of resources as functions related to the accreditation and elaboration of different scales related to trauma disease.4,5 The methodology used in the different registries is by no means uniform, however.6,7
Despite the above, and although there have been different regional initiatives in Spain,8–12 to date no registry has afforded national coverage of the patients admitted to Intensive Care Units (ICUs). The Trauma and Neurointensive Care Working Group (WG) of the Spanish Society of Intensive Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias [SEMICYUC]) has dedicated effort to the development of a severe TR that may serve as a vehicle for improving the documentation, care and investigation of STD in Spain.2 The RETRAUCI (Trauma Registry in the ICU [Registry TRAuma en UCI]) was started as a registry pilot initiative in a series of hospitals with a particular interest in severe trauma.
The aim of this study is to describe the characteristics of STD and its management in Spanish ICUs, based on the first results of the RETRAUCI pilot initiative.
Material and methodsThe registry was identified as a need in the course of the meetings of the Trauma and Neurointensive Care Working Group of the SEMICYUC. Finally, and after several preliminary meetings, data collection was started on 23 November 2012 in some selected centers. During this pilot phase, the data were entered by the supervising investigator in each center using a Microsoft Access spreadsheet. At the time of submission of this study, the online tool had already been activated (www.retrauci.org).13 Approval was obtained from the corresponding Ethics Committees.
Inclusion criteriaThe study included all patients admitted to an adult patients ICU due to STD during the study period, with a stay of over 24h. Cases involving shorter stays with a fatal outcome were also included.
Data collectionThe following data were collected:
- -
Epidemiological information, including age, gender, date and time of trauma and of admission to the ICU, intentionality, mechanism and type of trauma, previous use of antiplatelet or anticoagulant medication, and potential implication of different drugs of abuse.
- -
Aspects related to out-hospital care, including the type of initial medical care and the need for lung isolation measures.
- -
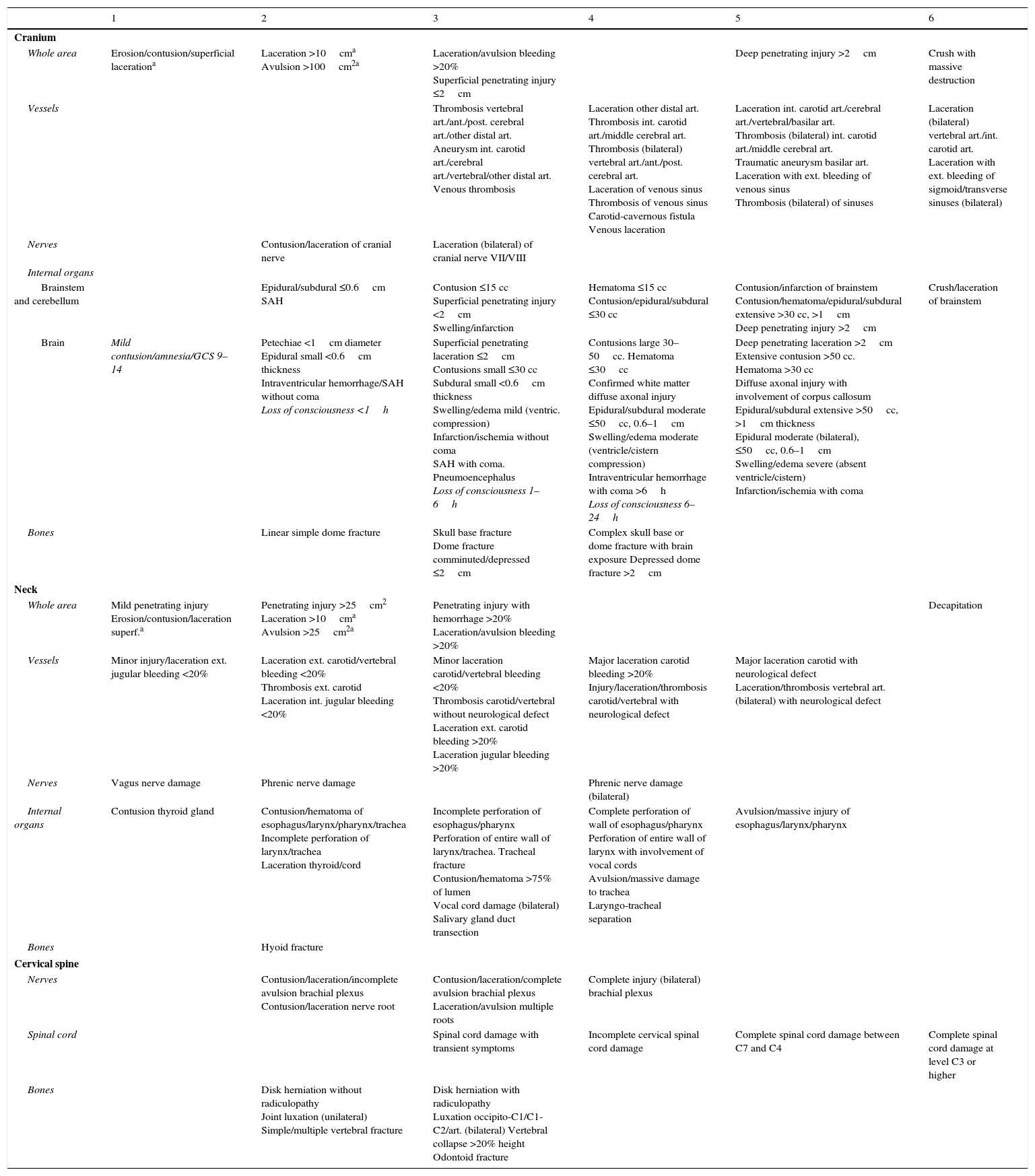
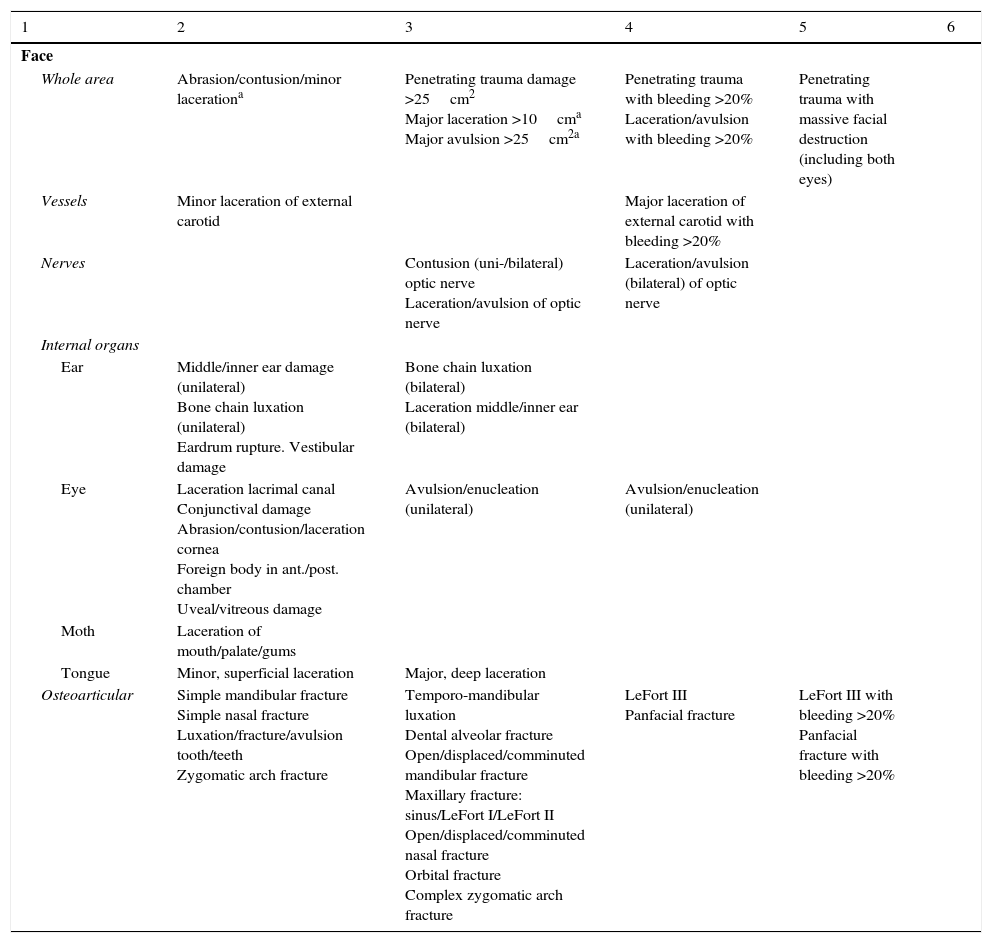
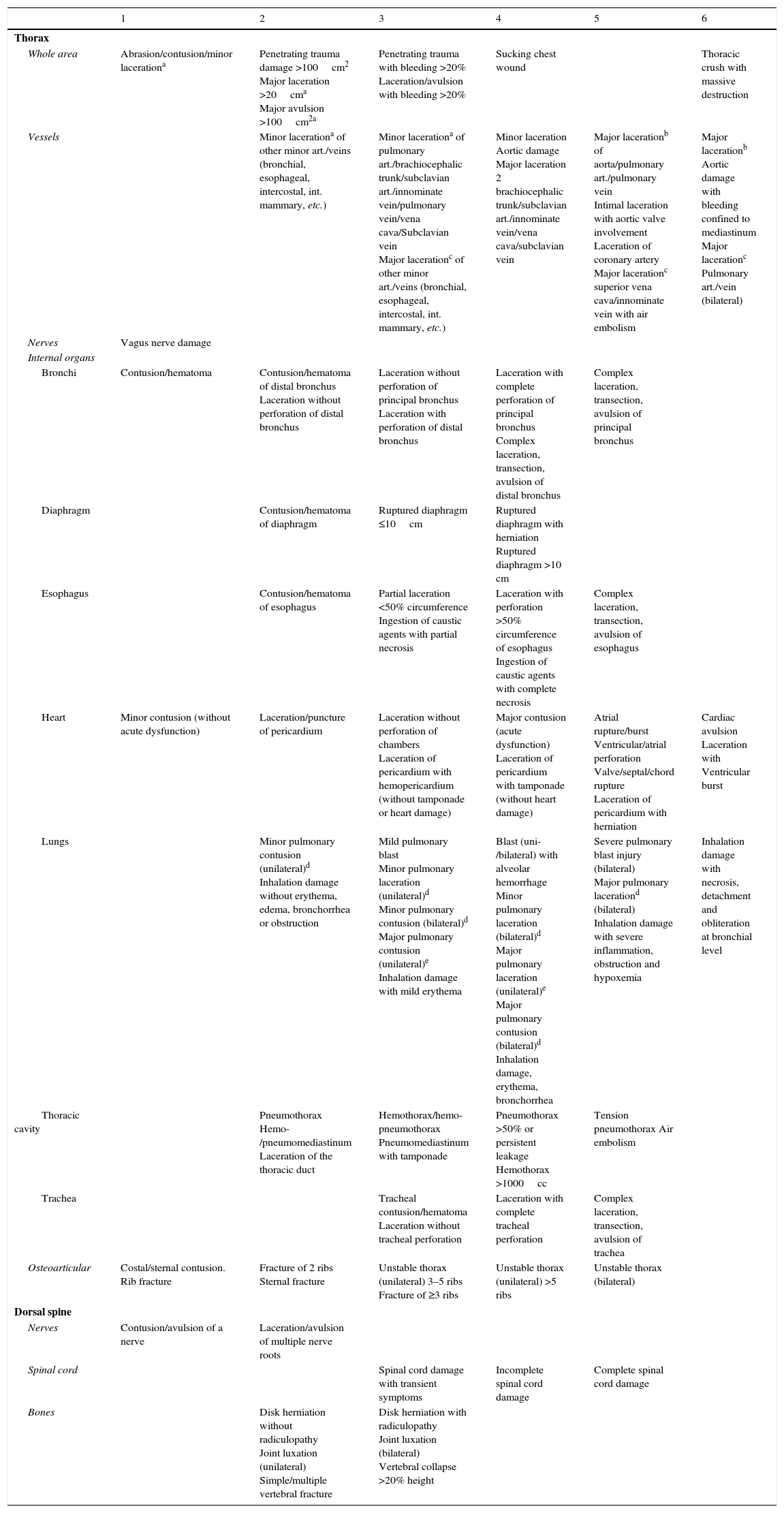
Registry of trauma injuries according to the Abbreviated Injury Scale (AIS),14 and calculation of different severity scores based on physiological (Revised Trauma Score [RTS])15 and anatomical aspects (Injury Severity Score [ISS]).16
- -
Complications during admission to the ICU, including the hemodynamic condition upon admission, the existence of coagulopathy, rhabdomyolysis, respiratory dysfunction, multiorgan failure syndrome, intracranial hypertension, renal failure and nosocomial infection. The definitions are described in Annex 1.
- -
Resource utilization, including blood product transfusions, number of urgent surgeries in the first 24h, and number of non-urgent surgeries, days on mechanical ventilation, pneumological monitoring, tracheotomy (percutaneous or surgical), arteriography for hemostasis and neuromonitoring techniques (ICP, SjO2, PtiO2 and NIRS).
- -
Evolution and final destination of the patients in ICU.
In 7 of the 13 centers that participated in the pilot phase (Annex 2), the injuries were coded with the 7 digits of the AIS in its updated version corresponding to the year 2008.17 In those centers where no complete coding with the 7 digits was made, a customized abridged version was used (Annex 3) for calculating the ISS.
Statistical analysisThe normal distribution of the variables was assessed using the Kolmogorov–Smirnov test. The quantitative variables followed a normal distribution, and were therefore reported as the mean±standard deviation. Categorical variables were reported as number (percentage).
The bivariate analysis (differences between 2 groups) of the categorical variables was based on the chi-squared test, using the Fisher exact test if the expected frequency of a variable was less than 5 in 2×2 tables. The Student's t-test was used in the case of quantitative variables. Analysis of variance (ANOVA) was used when comparing more than two variables. The SPSS version 20 statistical package (IBM Corporation, 2011) was used throughout. Statistical significance was considered for p<0.05.
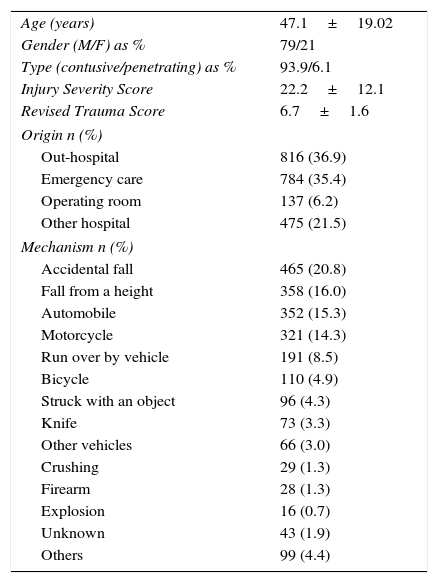
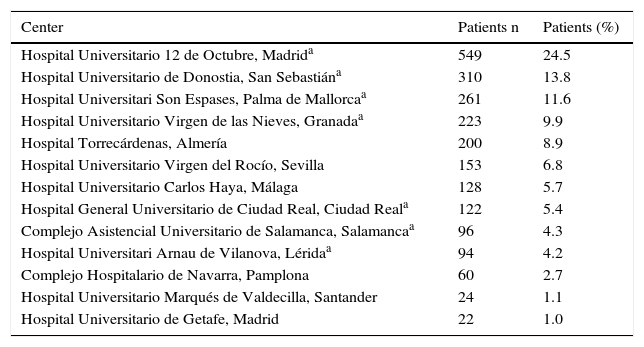
ResultsBetween 23 November 2012 and 31 January 2015 we included a total of 2242 patients admitted to the participating ICUs due to STD. The distribution of patients per participating center in the pilot phase is shown in Annex A. The characteristics of the patients included in the registry are summarized in Table 1. Of the included patients, 20.6% were over 65 years of age. Trauma was unintentional in 1890 cases (84.4%), intentional in 13.9% and unknown in 1.7%. Injury occurred in the context of a working accident in 154 patients (6.9%), a sports accident in 126 patients (5.6%), physical assault in 149 patients (6.7%), and attempted suicide in 162 patients (7.2%). Traffic accidents considered globally regardless of the type of vehicle, and falls, were the most frequent causes of trauma.
Epidemiological characteristics.
| Age (years) | 47.1±19.02 |
| Gender (M/F) as % | 79/21 |
| Type (contusive/penetrating) as % | 93.9/6.1 |
| Injury Severity Score | 22.2±12.1 |
| Revised Trauma Score | 6.7±1.6 |
| Origin n (%) | |
| Out-hospital | 816 (36.9) |
| Emergency care | 784 (35.4) |
| Operating room | 137 (6.2) |
| Other hospital | 475 (21.5) |
| Mechanism n (%) | |
| Accidental fall | 465 (20.8) |
| Fall from a height | 358 (16.0) |
| Automobile | 352 (15.3) |
| Motorcycle | 321 (14.3) |
| Run over by vehicle | 191 (8.5) |
| Bicycle | 110 (4.9) |
| Struck with an object | 96 (4.3) |
| Knife | 73 (3.3) |
| Other vehicles | 66 (3.0) |
| Crushing | 29 (1.3) |
| Firearm | 28 (1.3) |
| Explosion | 16 (0.7) |
| Unknown | 43 (1.9) |
| Others | 99 (4.4) |
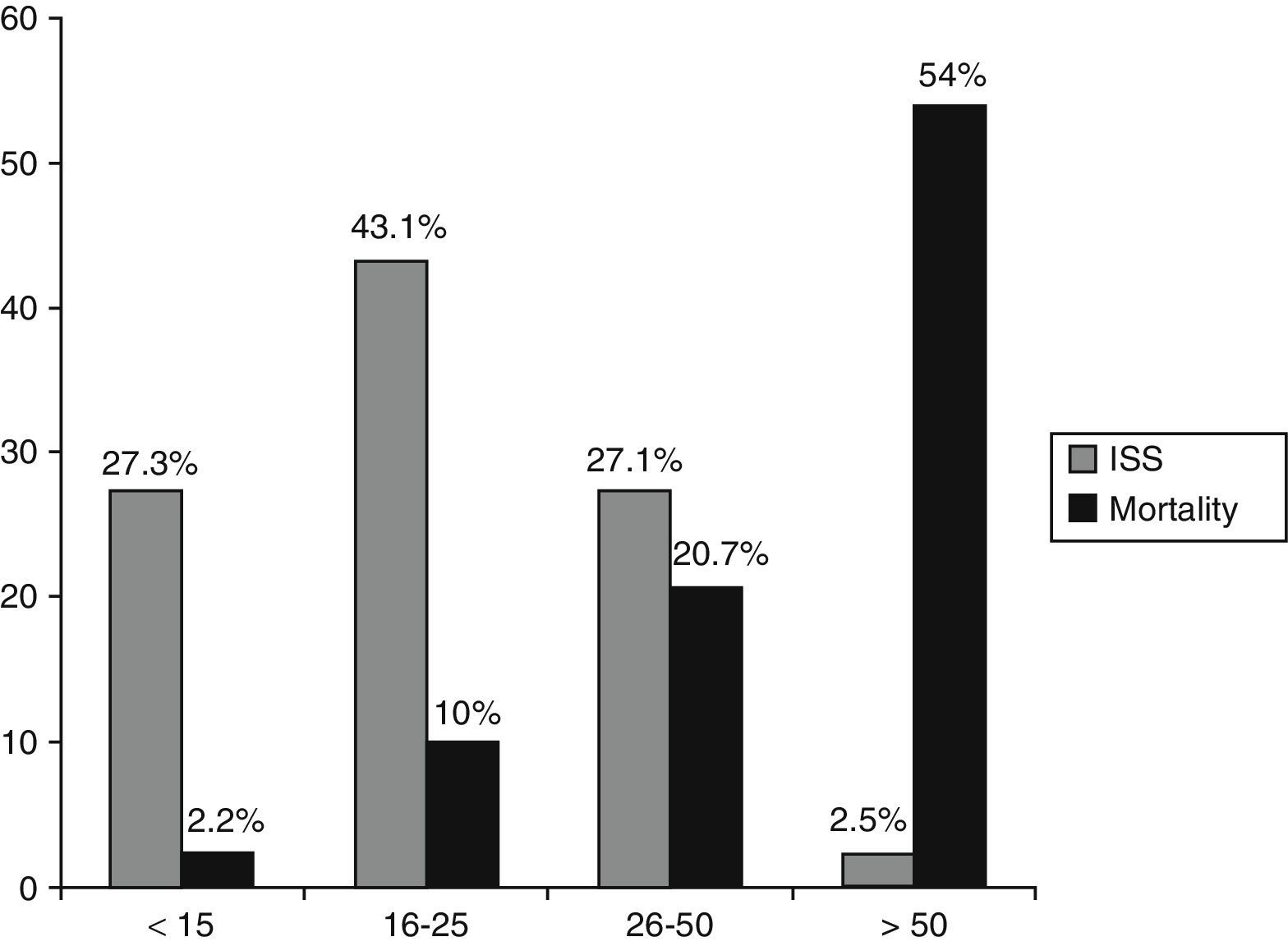
The percentage of patients with ISS>15 and RTS<6 was 72.7% and 26%, respectively.
A total of 12.4% of the subjects presented coagulopathy prior to trauma, 6.8% received antiplatelet medication, and 5.6% anticoagulant treatment. In 27.9% of the cases substance abuse was clinically suspected or confirmed by the laboratory tests.
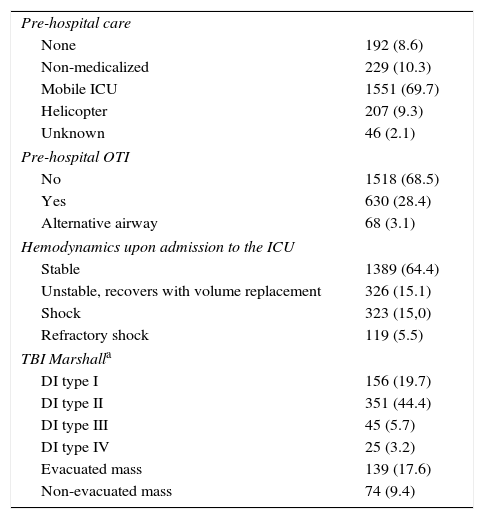
The type of initial out-hospital care, the need for orotracheal intubation or in situ alternative airway, the hemodynamic situation upon admission to the ICU, and the evaluation of brain injury based on the radiological data are summarized in Table 2.
First care n (%).
| Pre-hospital care | |
| None | 192 (8.6) |
| Non-medicalized | 229 (10.3) |
| Mobile ICU | 1551 (69.7) |
| Helicopter | 207 (9.3) |
| Unknown | 46 (2.1) |
| Pre-hospital OTI | |
| No | 1518 (68.5) |
| Yes | 630 (28.4) |
| Alternative airway | 68 (3.1) |
| Hemodynamics upon admission to the ICU | |
| Stable | 1389 (64.4) |
| Unstable, recovers with volume replacement | 326 (15.1) |
| Shock | 323 (15,0) |
| Refractory shock | 119 (5.5) |
| TBI Marshalla | |
| DI type I | 156 (19.7) |
| DI type II | 351 (44.4) |
| DI type III | 45 (5.7) |
| DI type IV | 25 (3.2) |
| Evacuated mass | 139 (17.6) |
| Non-evacuated mass | 74 (9.4) |
OTI: orotracheal intubation; DI: diffuse injury; TBI: traumatic brain injury; ICU: Intensive Care Unit.
The mean time from trauma to admission to the ICU was 4.7±5.3h. There were significant differences in the time from trauma to admission to the ICU according to the type of first medical care provided: no pre-hospital care (7.3±4.5h), non-medicalized care (5.8±3.4h), mobile ICU (4.2±5.6h), helicopter (4.3±3.4h) and unknown (7.6±4.8h) (p<0.0001). The post hoc analysis found the mobile ICU to show significant differences versus no pre-hospital care, non-medicalized care and unknown care, while helicopter transfer showed significant differences in the post hoc analysis versus no pre-hospital care and unknown care. Regarding the time of admission, 24.2% of the patients were admitted in the course of the morning shift (08:01–15:00h), 39.5% in the afternoon (15:01–22:00h), and 36.2% during the night shift (22:01–08:00h).
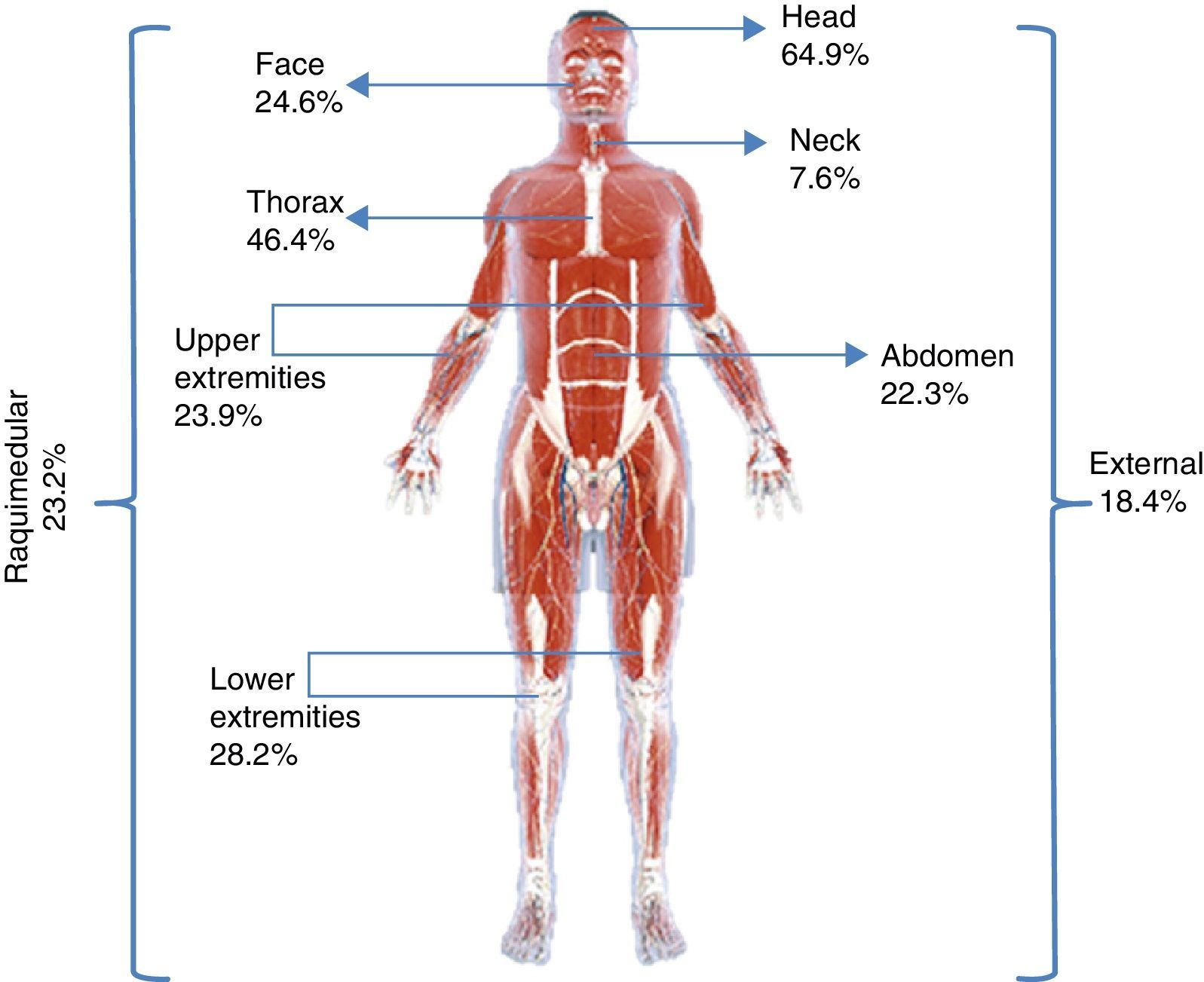
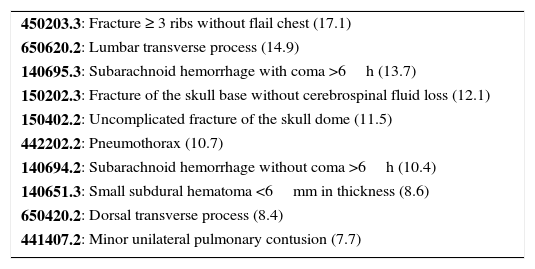
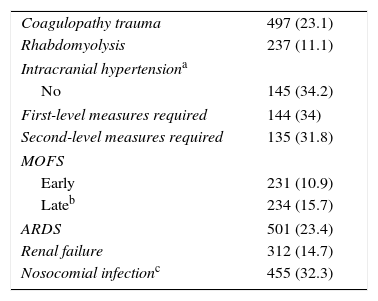
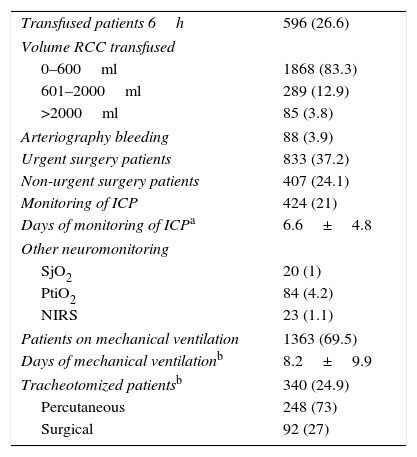
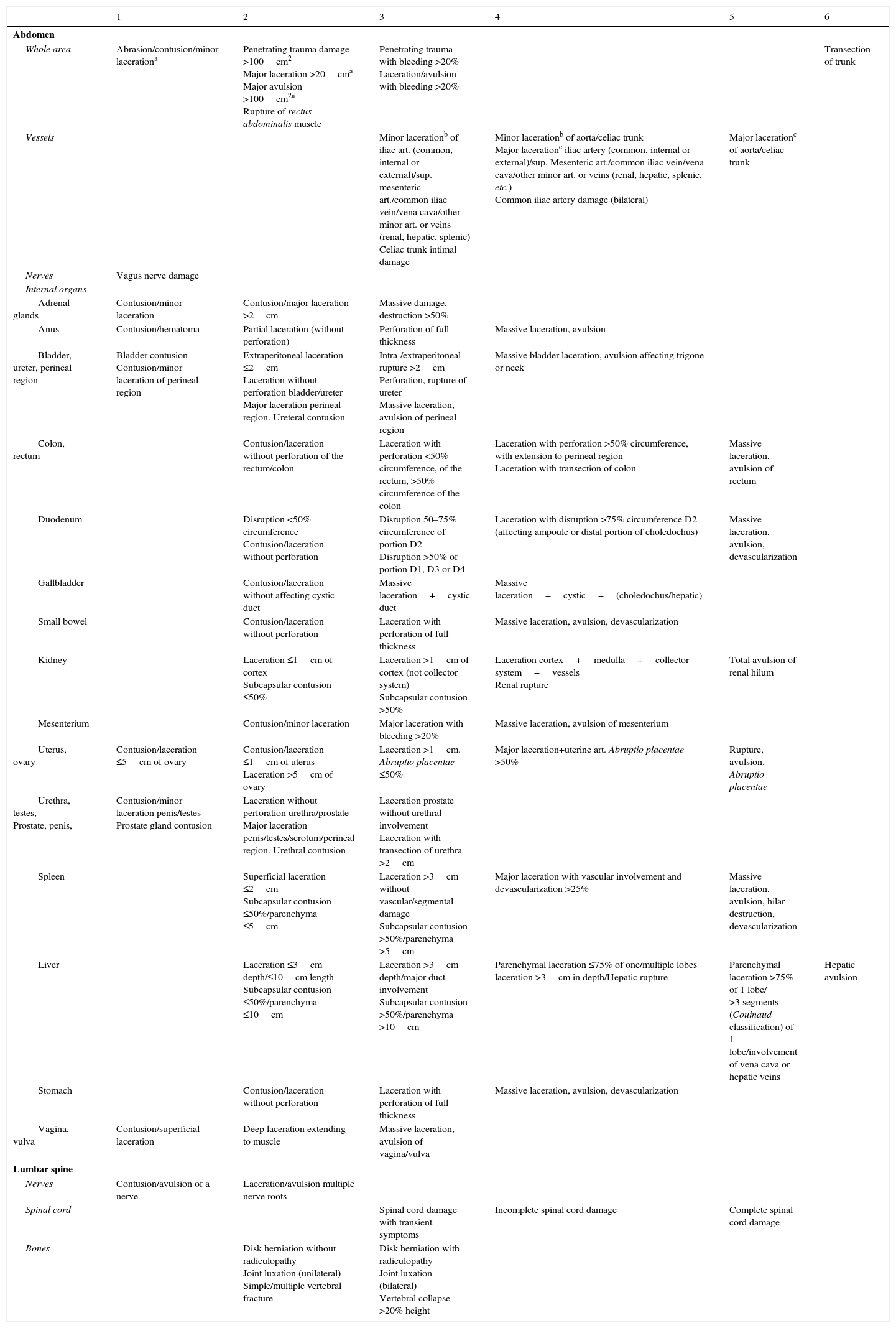
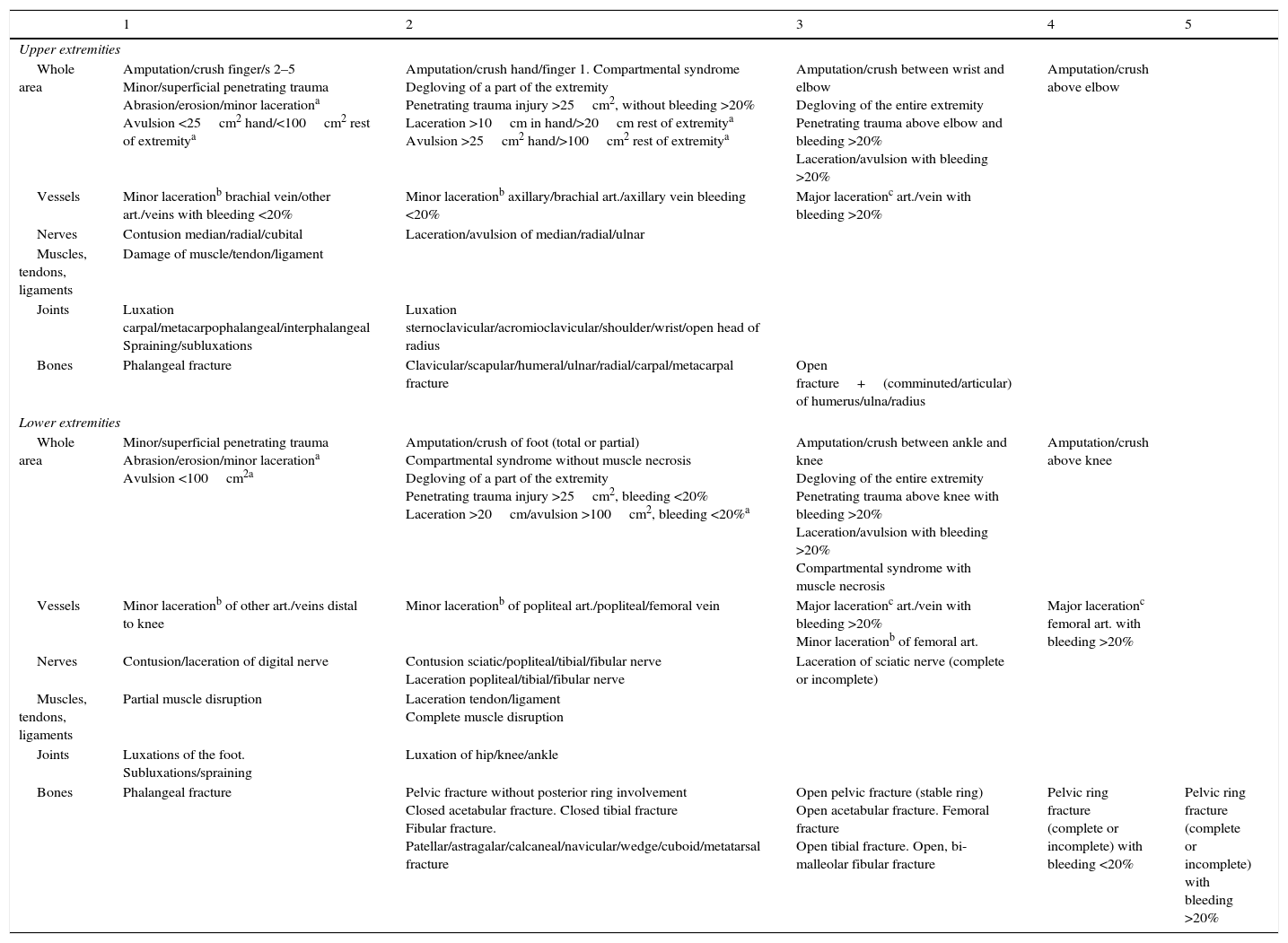
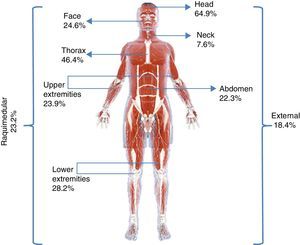
A total of 9890 injuries in 1665 patients were coded. The most commonly coded injuries according to the AIS are shown in Table 3, and the percentage injuries in each body region are indicated in Fig. 1. The percentage patients with each type of complication are shown in Table 4, while resource utilization on the part of the patients in the study sample is reported in Table 5.
Most frequent coded injuries in 1665 patients (%).
| 450203.3: Fracture ≥ 3 ribs without flail chest (17.1) |
| 650620.2: Lumbar transverse process (14.9) |
| 140695.3: Subarachnoid hemorrhage with coma >6h (13.7) |
| 150202.3: Fracture of the skull base without cerebrospinal fluid loss (12.1) |
| 150402.2: Uncomplicated fracture of the skull dome (11.5) |
| 442202.2: Pneumothorax (10.7) |
| 140694.2: Subarachnoid hemorrhage without coma >6h (10.4) |
| 140651.3: Small subdural hematoma <6mm in thickness (8.6) |
| 650420.2: Dorsal transverse process (8.4) |
| 441407.2: Minor unilateral pulmonary contusion (7.7) |
Complications associated to trauma, n (%).
| Coagulopathy trauma | 497 (23.1) |
| Rhabdomyolysis | 237 (11.1) |
| Intracranial hypertensiona | |
| No | 145 (34.2) |
| First-level measures required | 144 (34) |
| Second-level measures required | 135 (31.8) |
| MOFS | |
| Early | 231 (10.9) |
| Lateb | 234 (15.7) |
| ARDS | 501 (23.4) |
| Renal failure | 312 (14.7) |
| Nosocomial infectionc | 455 (32.3) |
MOFS: multiorgan failure syndrome; ARDS: acute respiratory distress syndrome.
Utilization of resources, n (%).
| Transfused patients 6h | 596 (26.6) |
| Volume RCC transfused | |
| 0–600ml | 1868 (83.3) |
| 601–2000ml | 289 (12.9) |
| >2000ml | 85 (3.8) |
| Arteriography bleeding | 88 (3.9) |
| Urgent surgery patients | 833 (37.2) |
| Non-urgent surgery patients | 407 (24.1) |
| Monitoring of ICP | 424 (21) |
| Days of monitoring of ICPa | 6.6±4.8 |
| Other neuromonitoring | |
| SjO2 | 20 (1) |
| PtiO2 | 84 (4.2) |
| NIRS | 23 (1.1) |
| Patients on mechanical ventilation | 1363 (69.5) |
| Days of mechanical ventilationb | 8.2±9.9 |
| Tracheotomized patientsb | 340 (24.9) |
| Percutaneous | 248 (73) |
| Surgical | 92 (27) |
RCC: red cell concentrates; NIRS: near-infrared spectroscopy; ICP: intracranial pressure; PtiO2: tissue oxygen pressure; SjO2: jugular bulb oxygen saturation.
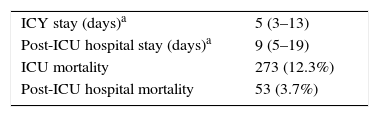
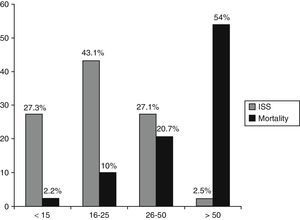
The in-ICU mortality rate was 12.3%, while the in-hospital mortality rate was 16%. The days of ICU stay and of post-ICU hospital stay, together with in-ICU mortality and post-ICU hospital mortality are reported in Table 6. A significant association was observed between the ISS score and mortality (p<0.0001) (Fig. 2). Of the survivors, 11.6% were transferred to another ICU after discharge, while 21.1% were moved to another hospital center.
Limitation of life support measures was applied to one degree or other in 6.9% of the overall patient sample. Specifically, limitation of life support was implemented in 55.1% of the 273 patients that died (156 patients). A total of 27.5% of those who died became organ donors.
DiscussionThe data presented in this study offer a first impression of the epidemiology and management of patients with STD admitted to the ICUs in Spain. The findings suggest that the introduction of a national TR is feasible, and may result in improved knowledge of STD in our setting and better patient care in the future.
The standard patient with STD in our setting is a middle-aged male with unintentional contusion injuries caused by a traffic accident or fall, and initially attended by a mobile ICU in the out-hospital setting, without the need for in situ orotracheal intubation in 70% of the cases. The patient is hemodynamically stable at the time of first care and mainly suffers brain (type II diffuse injury) and chest trauma. Three out of every four patients are admitted to the ICU in the course of the afternoon or night shift, and are therefore attended by less experienced personnel on duty. One out of every three patients require urgent intervention, while a similar proportion receive deferred care. These typical patients are associated to important resource utilization, and most of them receive mechanical ventilation during admission to intensive care, and suffer different complications. Intracranial hypertension is frequent in patients with brain injuries. Other neuromonitoring techniques are very little used. One out of every four patients on mechanical ventilation require a tracheotomy (preferentially percutaneous). The mortality rate is relatively low, though the stay in the ICU and in hospital is long.
The keeping of a TR is associated to improved knowledge of the epidemiology, processes and outcomes of the management of patients with STD,2–7 and over time the documentation of such information is associated to lesser mortality and disability in patients with STD.18 At this point it is still too early to assess this latter aspect in our registry. A controversial issue in relation to TRs is what parameters should be recorded and how optimum data collection can be ensured. In this regard, a recent Scandinavian study involving 783 patients from different geographical areas19 has found that certain physiological and time-related variables pose compilation difficulties.
In our case, this pilot phase has allowed us to modify the way in which certain variables are collected and to add some others that may be of interest. Such flexibility is necessary, since a TR must be adaptable to the setting in which it is kept and modifiable according to the results obtained and the variations in scientific evidence over time.7 Accordingly, and in comparison with the pilot phase presented herein, the latest version of the online access base contemplates among other modifications the time elapsed from the moment of trauma to hospital admission and from hospital admission to admission to the ICU; intoxication due to drugs and psychotropic agents of chronic use; the administration of new antiplatelet agents and anticoagulant drugs; pupil status and the performing of decompressive craniotomy; documentation of the patients admitted to the ICU as potential organ donors; the total red cell concentrate units transfused in the first 24h instead of the number of milliliters transfused in the first 6h; the number of fresh plasma bags and massive transfusions; the use of continuous renal replacement therapies; the introduction of a new definition of acute respiratory distress syndrome based on the Berlin criterion; and neurological assessment at discharge from the ICU. Furthermore, we will be able to gain more complete information referred to different trauma severity scores, with automatic calculation of the ISS and the New ISS, and of survival probability.20
The pilot phase of the RETRAUCI has allowed us to detect errors and opportunities for improvement in the documentation and follow-up of trauma patients in Spain, and has shown that starting the initiative is feasible. On the other hand, it has given us an initial impression of the epidemiology and management of patients with STD admitted to the ICUs in our country.
In future, and ideally, an analysis of the quality of life of patients with STD also should be contemplated,21 though the optimum timing of such an analysis is not clear,22 and moreover it will require a great effort on the part of the investigators – particularly on considering the usual structure of Spanish ICUs.
The RETRAUCI was created as a project of the Trauma and Neurointensive Care Working Group of the SEMICYUC, with the intention of continuing over time and of having an impact upon the evolution of patients with STD, in the same way as with other Working Groups of the SEMICYUC in patients with ischemic heart disease or sepsis, through the ARIAM and ENVIN registries. At the time of drafting of this article, and with the online tool already active, several additional centers have announced their participation. From this article we wish to invite all Spanish ICUs that attend trauma cases to participate in the RETRAUCI through the mentioned online tool, since doing so will undoubtedly contribute to improve survival, increase volume and quality, and positively affect the health of these patients. The data obtained by means of the RETRAUCI can afford reliable information for public and political institutions with legislative intent, as well as optimize the use of resources and social awareness.7,23
We must take note of the limitations of this study in particular, and of registries in general. Firstly, the information presented herein arises from a voluntary TR in which the participating centers have expressed interest in joining the initiative. Coverage is therefore limited, and this may lead to bias in evaluating the results, since the registry documents information from particularly motivated centers.2 Furthermore, this TR only contemplates those patients that are effectively admitted to the ICU. As such, it is not representative of STD in general, since it does not contemplate patients who die before reaching hospital, and which represent most of the fatalities due to severe trauma (mainly as a result of bleeding),1,24 or minor traumatisms that do not require admission to the ICU.
In sum, the pilot phase of the RETRAUCI offers a first impression of patients with STD admitted to ICUs in Spain, and represents the first initiative of this kind. The consolidation of a national TR is feasible and in future may contribute to reduce mortality and disability among such patients.
Authorship/collaboratorsLuis Terceros-Almanza (Hospital Universitario 12 de Octubre), Ruth Salaberria-Udabe (Hospital Universitario de Donostia), Javier Homar-Ramírez (Hospital Universitari Son Espases), Francisca Inmaculada Pino-Sánchez (Hospital Universitario Virgen de las Nieves), Cecilia Carbayo-Górriz (Complejo Hospitalario de Torrecárdenas), Carmen Corcobado-Márquez (Hospital General Universitario de Ciudad Real), Javier Trujillano-Cabello (Hospital Universitari Arnau de Vilanova), Eduardo Miñambres-García (Hospital Universitario Marqués de Valdecilla), Amanda Lesmes-González (Hospital Universitario de Getafe).
Financial supportThe registry receives financial support from the Fundación Mutua Madrileña during three years for the development of an online data collection tool, assigned to the principal investigator of the project (Dr. Chico-Fernandez, reference no. AP117892013), in representation of the Trauma and Neurointensive Care Working Group of the SEMICYUC.
Conflict of interestThe authors declare that they have no conflict of interest.
The authors of this study wish to express their profound gratitude to Vicente Gómez-Tello (coordinator of the Working Groups of the SEMICYUC, Hospital Moncloa, Madrid) and Andrés J. Chacón (project manager, Xferic) for their collaboration in developing the registry, and to Miguel Ferrero-Fernández (computing science engineer of the Computing Department, SEMICYUC) for his work in developing the online tool of the RETRAUCI.
| Center | Patients n | Patients (%) |
|---|---|---|
| Hospital Universitario 12 de Octubre, Madrida | 549 | 24.5 |
| Hospital Universitario de Donostia, San Sebastiána | 310 | 13.8 |
| Hospital Universitari Son Espases, Palma de Mallorcaa | 261 | 11.6 |
| Hospital Universitario Virgen de las Nieves, Granadaa | 223 | 9.9 |
| Hospital Torrecárdenas, Almería | 200 | 8.9 |
| Hospital Universitario Virgen del Rocío, Sevilla | 153 | 6.8 |
| Hospital Universitario Carlos Haya, Málaga | 128 | 5.7 |
| Hospital General Universitario de Ciudad Real, Ciudad Reala | 122 | 5.4 |
| Complejo Asistencial Universitario de Salamanca, Salamancaa | 96 | 4.3 |
| Hospital Universitari Arnau de Vilanova, Léridaa | 94 | 4.2 |
| Complejo Hospitalario de Navarra, Pamplona | 60 | 2.7 |
| Hospital Universitario Marqués de Valdecilla, Santander | 24 | 1.1 |
| Hospital Universitario de Getafe, Madrid | 22 | 1.0 |
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| Cranium | ||||||
| Whole area | Erosion/contusion/superficial lacerationa | Laceration >10cma Avulsion >100cm2a | Laceration/avulsion bleeding >20% Superficial penetrating injury ≤2cm | Deep penetrating injury >2cm | Crush with massive destruction | |
| Vessels | Thrombosis vertebral art./ant./post. cerebral art./other distal art. Aneurysm int. carotid art./cerebral art./vertebral/other distal art. Venous thrombosis | Laceration other distal art. Thrombosis int. carotid art./middle cerebral art. Thrombosis (bilateral) vertebral art./ant./post. cerebral art. Laceration of venous sinus Thrombosis of venous sinus Carotid-cavernous fistula Venous laceration | Laceration int. carotid art./cerebral art./vertebral/basilar art. Thrombosis (bilateral) int. carotid art./middle cerebral art. Traumatic aneurysm basilar art. Laceration with ext. bleeding of venous sinus Thrombosis (bilateral) of sinuses | Laceration (bilateral) vertebral art./int. carotid art. Laceration with ext. bleeding of sigmoid/transverse sinuses (bilateral) | ||
| Nerves | Contusion/laceration of cranial nerve | Laceration (bilateral) of cranial nerve VII/VIII | ||||
| Internal organs | ||||||
| Brainstem and cerebellum | Epidural/subdural ≤0.6cm SAH | Contusion ≤15 cc Superficial penetrating injury <2cm Swelling/infarction | Hematoma ≤15 cc Contusion/epidural/subdural ≤30 cc | Contusion/infarction of brainstem Contusion/hematoma/epidural/subdural extensive >30 cc, >1cm Deep penetrating injury >2cm | Crush/laceration of brainstem | |
| Brain | Mild contusion/amnesia/GCS 9–14 | Petechiae <1cm diameter Epidural small <0.6cm thickness Intraventricular hemorrhage/SAH without coma Loss of consciousness <1h | Superficial penetrating laceration ≤2cm Contusions small ≤30 cc Subdural small <0.6cm thickness Swelling/edema mild (ventric. compression) Infarction/ischemia without coma SAH with coma. Pneumoencephalus Loss of consciousness 1–6h | Contusions large 30–50cc. Hematoma ≤30cc Confirmed white matter diffuse axonal injury Epidural/subdural moderate ≤50cc, 0.6–1cm Swelling/edema moderate (ventricle/cistern compression) Intraventricular hemorrhage with coma >6h Loss of consciousness 6–24h | Deep penetrating laceration >2cm Extensive contusion >50 cc. Hematoma >30 cc Diffuse axonal injury with involvement of corpus callosum Epidural/subdural extensive >50cc, >1cm thickness Epidural moderate (bilateral), ≤50cc, 0.6–1cm Swelling/edema severe (absent ventricle/cistern) Infarction/ischemia with coma | |
| Bones | Linear simple dome fracture | Skull base fracture Dome fracture comminuted/depressed ≤2cm | Complex skull base or dome fracture with brain exposure Depressed dome fracture >2cm | |||
| Neck | ||||||
| Whole area | Mild penetrating injury Erosion/contusion/laceration superf.a | Penetrating injury >25cm2 Laceration >10cma Avulsion >25cm2a | Penetrating injury with hemorrhage >20% Laceration/avulsion bleeding >20% | Decapitation | ||
| Vessels | Minor injury/laceration ext. jugular bleeding <20% | Laceration ext. carotid/vertebral bleeding <20% Thrombosis ext. carotid Laceration int. jugular bleeding <20% | Minor laceration carotid/vertebral bleeding <20% Thrombosis carotid/vertebral without neurological defect Laceration ext. carotid bleeding >20% Laceration jugular bleeding >20% | Major laceration carotid bleeding >20% Injury/laceration/thrombosis carotid/vertebral with neurological defect | Major laceration carotid with neurological defect Laceration/thrombosis vertebral art. (bilateral) with neurological defect | |
| Nerves | Vagus nerve damage | Phrenic nerve damage | Phrenic nerve damage (bilateral) | |||
| Internal organs | Contusion thyroid gland | Contusion/hematoma of esophagus/larynx/pharynx/trachea Incomplete perforation of larynx/trachea Laceration thyroid/cord | Incomplete perforation of esophagus/pharynx Perforation of entire wall of larynx/trachea. Tracheal fracture Contusion/hematoma >75% of lumen Vocal cord damage (bilateral) Salivary gland duct transection | Complete perforation of wall of esophagus/pharynx Perforation of entire wall of larynx with involvement of vocal cords Avulsion/massive damage to trachea Laryngo-tracheal separation | Avulsion/massive injury of esophagus/larynx/pharynx | |
| Bones | Hyoid fracture | |||||
| Cervical spine | ||||||
| Nerves | Contusion/laceration/incomplete avulsion brachial plexus Contusion/laceration nerve root | Contusion/laceration/complete avulsion brachial plexus Laceration/avulsion multiple roots | Complete injury (bilateral) brachial plexus | |||
| Spinal cord | Spinal cord damage with transient symptoms | Incomplete cervical spinal cord damage | Complete spinal cord damage between C7 and C4 | Complete spinal cord damage at level C3 or higher | ||
| Bones | Disk herniation without radiculopathy Joint luxation (unilateral) Simple/multiple vertebral fracture | Disk herniation with radiculopathy Luxation occipito-C1/C1-C2/art. (bilateral) Vertebral collapse >20% height Odontoid fracture | ||||
| 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|
| Face | |||||
| Whole area | Abrasion/contusion/minor lacerationa | Penetrating trauma damage >25cm2 Major laceration >10cma Major avulsion >25cm2a | Penetrating trauma with bleeding >20% Laceration/avulsion with bleeding >20% | Penetrating trauma with massive facial destruction (including both eyes) | |
| Vessels | Minor laceration of external carotid | Major laceration of external carotid with bleeding >20% | |||
| Nerves | Contusion (uni-/bilateral) optic nerve Laceration/avulsion of optic nerve | Laceration/avulsion (bilateral) of optic nerve | |||
| Internal organs | |||||
| Ear | Middle/inner ear damage (unilateral) Bone chain luxation (unilateral) Eardrum rupture. Vestibular damage | Bone chain luxation (bilateral) Laceration middle/inner ear (bilateral) | |||
| Eye | Laceration lacrimal canal Conjunctival damage Abrasion/contusion/laceration cornea Foreign body in ant./post. chamber Uveal/vitreous damage | Avulsion/enucleation (unilateral) | Avulsion/enucleation (unilateral) | ||
| Moth | Laceration of mouth/palate/gums | ||||
| Tongue | Minor, superficial laceration | Major, deep laceration | |||
| Osteoarticular | Simple mandibular fracture Simple nasal fracture Luxation/fracture/avulsion tooth/teeth Zygomatic arch fracture | Temporo-mandibular luxation Dental alveolar fracture Open/displaced/comminuted mandibular fracture Maxillary fracture: sinus/LeFort I/LeFort II Open/displaced/comminuted nasal fracture Orbital fracture Complex zygomatic arch fracture | LeFort III Panfacial fracture | LeFort III with bleeding >20% Panfacial fracture with bleeding >20% | |
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| Thorax | ||||||
| Whole area | Abrasion/contusion/minor lacerationa | Penetrating trauma damage >100cm2 Major laceration >20cma Major avulsion >100cm2a | Penetrating trauma with bleeding >20% Laceration/avulsion with bleeding >20% | Sucking chest wound | Thoracic crush with massive destruction | |
| Vessels | Minor lacerationa of other minor art./veins (bronchial, esophageal, intercostal, int. mammary, etc.) | Minor lacerationa of pulmonary art./brachiocephalic trunk/subclavian art./innominate vein/pulmonary vein/vena cava/Subclavian vein Major lacerationc of other minor art./veins (bronchial, esophageal, intercostal, int. mammary, etc.) | Minor laceration Aortic damage Major laceration 2 brachiocephalic trunk/subclavian art./innominate vein/vena cava/subclavian vein | Major lacerationb of aorta/pulmonary art./pulmonary vein Intimal laceration with aortic valve involvement Laceration of coronary artery Major lacerationc superior vena cava/innominate vein with air embolism | Major lacerationb Aortic damage with bleeding confined to mediastinum Major lacerationc Pulmonary art./vein (bilateral) | |
| Nerves | Vagus nerve damage | |||||
| Internal organs | ||||||
| Bronchi | Contusion/hematoma | Contusion/hematoma of distal bronchus Laceration without perforation of distal bronchus | Laceration without perforation of principal bronchus Laceration with perforation of distal bronchus | Laceration with complete perforation of principal bronchus Complex laceration, transection, avulsion of distal bronchus | Complex laceration, transection, avulsion of principal bronchus | |
| Diaphragm | Contusion/hematoma of diaphragm | Ruptured diaphragm ≤10cm | Ruptured diaphragm with herniation Ruptured diaphragm >10 cm | |||
| Esophagus | Contusion/hematoma of esophagus | Partial laceration <50% circumference Ingestion of caustic agents with partial necrosis | Laceration with perforation >50% circumference of esophagus Ingestion of caustic agents with complete necrosis | Complex laceration, transection, avulsion of esophagus | ||
| Heart | Minor contusion (without acute dysfunction) | Laceration/puncture of pericardium | Laceration without perforation of chambers Laceration of pericardium with hemopericardium (without tamponade or heart damage) | Major contusion (acute dysfunction) Laceration of pericardium with tamponade (without heart damage) | Atrial rupture/burst Ventricular/atrial perforation Valve/septal/chord rupture Laceration of pericardium with herniation | Cardiac avulsion Laceration with Ventricular burst |
| Lungs | Minor pulmonary contusion (unilateral)d Inhalation damage without erythema, edema, bronchorrhea or obstruction | Mild pulmonary blast Minor pulmonary laceration (unilateral)d Minor pulmonary contusion (bilateral)d Major pulmonary contusion (unilateral)e Inhalation damage with mild erythema | Blast (uni-/bilateral) with alveolar hemorrhage Minor pulmonary laceration (bilateral)d Major pulmonary laceration (unilateral)e Major pulmonary contusion (bilateral)d Inhalation damage, erythema, bronchorrhea | Severe pulmonary blast injury (bilateral) Major pulmonary lacerationd (bilateral) Inhalation damage with severe inflammation, obstruction and hypoxemia | Inhalation damage with necrosis, detachment and obliteration at bronchial level | |
| Thoracic cavity | Pneumothorax Hemo-/pneumomediastinum Laceration of the thoracic duct | Hemothorax/hemo-pneumothorax Pneumomediastinum with tamponade | Pneumothorax >50% or persistent leakage Hemothorax >1000cc | Tension pneumothorax Air embolism | ||
| Trachea | Tracheal contusion/hematoma Laceration without tracheal perforation | Laceration with complete tracheal perforation | Complex laceration, transection, avulsion of trachea | |||
| Osteoarticular | Costal/sternal contusion. Rib fracture | Fracture of 2 ribs Sternal fracture | Unstable thorax (unilateral) 3–5 ribs Fracture of ≥3 ribs | Unstable thorax (unilateral) >5 ribs | Unstable thorax (bilateral) | |
| Dorsal spine | ||||||
| Nerves | Contusion/avulsion of a nerve | Laceration/avulsion of multiple nerve roots | ||||
| Spinal cord | Spinal cord damage with transient symptoms | Incomplete spinal cord damage | Complete spinal cord damage | |||
| Bones | Disk herniation without radiculopathy Joint luxation (unilateral) Simple/multiple vertebral fracture | Disk herniation with radiculopathy Joint luxation (bilateral) Vertebral collapse >20% height | ||||
Minor vascular laceration: superficial/intimal, without affecting entire circumference and with bleeding <20%.
Major vascular laceration: rupture of entire circumference, complete transection and with bleeding >20%.
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| Abdomen | ||||||
| Whole area | Abrasion/contusion/minor lacerationa | Penetrating trauma damage >100cm2 Major laceration >20cma Major avulsion >100cm2a Rupture of rectus abdominalis muscle | Penetrating trauma with bleeding >20% Laceration/avulsion with bleeding >20% | Transection of trunk | ||
| Vessels | Minor lacerationb of iliac art. (common, internal or external)/sup. mesenteric art./common iliac vein/vena cava/other minor art. or veins (renal, hepatic, splenic) Celiac trunk intimal damage | Minor lacerationb of aorta/celiac trunk Major lacerationc iliac artery (common, internal or external)/sup. Mesenteric art./common iliac vein/vena cava/other minor art. or veins (renal, hepatic, splenic, etc.) Common iliac artery damage (bilateral) | Major lacerationc of aorta/celiac trunk | |||
| Nerves | Vagus nerve damage | |||||
| Internal organs | ||||||
| Adrenal glands | Contusion/minor laceration | Contusion/major laceration >2cm | Massive damage, destruction >50% | |||
| Anus | Contusion/hematoma | Partial laceration (without perforation) | Perforation of full thickness | Massive laceration, avulsion | ||
| Bladder, ureter, perineal region | Bladder contusion Contusion/minor laceration of perineal region | Extraperitoneal laceration ≤2cm Laceration without perforation bladder/ureter Major laceration perineal region. Ureteral contusion | Intra-/extraperitoneal rupture >2cm Perforation, rupture of ureter Massive laceration, avulsion of perineal region | Massive bladder laceration, avulsion affecting trigone or neck | ||
| Colon, rectum | Contusion/laceration without perforation of the rectum/colon | Laceration with perforation <50% circumference, of the rectum, >50% circumference of the colon | Laceration with perforation >50% circumference, with extension to perineal region Laceration with transection of colon | Massive laceration, avulsion of rectum | ||
| Duodenum | Disruption <50% circumference Contusion/laceration without perforation | Disruption 50–75% circumference of portion D2 Disruption >50% of portion D1, D3 or D4 | Laceration with disruption >75% circumference D2 (affecting ampoule or distal portion of choledochus) | Massive laceration, avulsion, devascularization | ||
| Gallbladder | Contusion/laceration without affecting cystic duct | Massive laceration+cystic duct | Massive laceration+cystic+(choledochus/hepatic) | |||
| Small bowel | Contusion/laceration without perforation | Laceration with perforation of full thickness | Massive laceration, avulsion, devascularization | |||
| Kidney | Laceration ≤1cm of cortex Subcapsular contusion ≤50% | Laceration >1cm of cortex (not collector system) Subcapsular contusion >50% | Laceration cortex+medulla+collector system+vessels Renal rupture | Total avulsion of renal hilum | ||
| Mesenterium | Contusion/minor laceration | Major laceration with bleeding >20% | Massive laceration, avulsion of mesenterium | |||
| Uterus, ovary | Contusion/laceration ≤5cm of ovary | Contusion/laceration ≤1cm of uterus Laceration >5cm of ovary | Laceration >1cm. Abruptio placentae ≤50% | Major laceration+uterine art. Abruptio placentae >50% | Rupture, avulsion. Abruptio placentae | |
| Urethra, testes, Prostate, penis, | Contusion/minor laceration penis/testes Prostate gland contusion | Laceration without perforation urethra/prostate Major laceration penis/testes/scrotum/perineal region. Urethral contusion | Laceration prostate without urethral involvement Laceration with transection of urethra >2cm | |||
| Spleen | Superficial laceration ≤2cm Subcapsular contusion ≤50%/parenchyma ≤5cm | Laceration >3cm without vascular/segmental damage Subcapsular contusion >50%/parenchyma >5cm | Major laceration with vascular involvement and devascularization >25% | Massive laceration, avulsion, hilar destruction, devascularization | ||
| Liver | Laceration ≤3cm depth/≤10cm length Subcapsular contusion ≤50%/parenchyma ≤10cm | Laceration >3cm depth/major duct involvement Subcapsular contusion >50%/parenchyma >10cm | Parenchymal laceration ≤75% of one/multiple lobes laceration >3cm in depth/Hepatic rupture | Parenchymal laceration >75% of 1 lobe/ >3 segments (Couinaud classification) of 1 lobe/involvement of vena cava or hepatic veins | Hepatic avulsion | |
| Stomach | Contusion/laceration without perforation | Laceration with perforation of full thickness | Massive laceration, avulsion, devascularization | |||
| Vagina, vulva | Contusion/superficial laceration | Deep laceration extending to muscle | Massive laceration, avulsion of vagina/vulva | |||
| Lumbar spine | ||||||
| Nerves | Contusion/avulsion of a nerve | Laceration/avulsion multiple nerve roots | ||||
| Spinal cord | Spinal cord damage with transient symptoms | Incomplete spinal cord damage | Complete spinal cord damage | |||
| Bones | Disk herniation without radiculopathy Joint luxation (unilateral) Simple/multiple vertebral fracture | Disk herniation with radiculopathy Joint luxation (bilateral) Vertebral collapse >20% height | ||||
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| Upper extremities | |||||
| Whole area | Amputation/crush finger/s 2–5 Minor/superficial penetrating trauma Abrasion/erosion/minor lacerationa Avulsion <25cm2 hand/<100cm2 rest of extremitya | Amputation/crush hand/finger 1. Compartmental syndrome Degloving of a part of the extremity Penetrating trauma injury >25cm2, without bleeding >20% Laceration >10cm in hand/>20cm rest of extremitya Avulsion >25cm2 hand/>100cm2 rest of extremitya | Amputation/crush between wrist and elbow Degloving of the entire extremity Penetrating trauma above elbow and bleeding >20% Laceration/avulsion with bleeding >20% | Amputation/crush above elbow | |
| Vessels | Minor lacerationb brachial vein/other art./veins with bleeding <20% | Minor lacerationb axillary/brachial art./axillary vein bleeding <20% | Major lacerationc art./vein with bleeding >20% | ||
| Nerves | Contusion median/radial/cubital | Laceration/avulsion of median/radial/ulnar | |||
| Muscles, tendons, ligaments | Damage of muscle/tendon/ligament | ||||
| Joints | Luxation carpal/metacarpophalangeal/interphalangeal Spraining/subluxations | Luxation sternoclavicular/acromioclavicular/shoulder/wrist/open head of radius | |||
| Bones | Phalangeal fracture | Clavicular/scapular/humeral/ulnar/radial/carpal/metacarpal fracture | Open fracture+(comminuted/articular) of humerus/ulna/radius | ||
| Lower extremities | |||||
| Whole area | Minor/superficial penetrating trauma Abrasion/erosion/minor lacerationa Avulsion <100cm2a | Amputation/crush of foot (total or partial) Compartmental syndrome without muscle necrosis Degloving of a part of the extremity Penetrating trauma injury >25cm2, bleeding <20% Laceration >20cm/avulsion >100cm2, bleeding <20%a | Amputation/crush between ankle and knee Degloving of the entire extremity Penetrating trauma above knee with bleeding >20% Laceration/avulsion with bleeding >20% Compartmental syndrome with muscle necrosis | Amputation/crush above knee | |
| Vessels | Minor lacerationb of other art./veins distal to knee | Minor lacerationb of popliteal art./popliteal/femoral vein | Major lacerationc art./vein with bleeding >20% Minor lacerationb of femoral art. | Major lacerationc femoral art. with bleeding >20% | |
| Nerves | Contusion/laceration of digital nerve | Contusion sciatic/popliteal/tibial/fibular nerve Laceration popliteal/tibial/fibular nerve | Laceration of sciatic nerve (complete or incomplete) | ||
| Muscles, tendons, ligaments | Partial muscle disruption | Laceration tendon/ligament Complete muscle disruption | |||
| Joints | Luxations of the foot. Subluxations/spraining | Luxation of hip/knee/ankle | |||
| Bones | Phalangeal fracture | Pelvic fracture without posterior ring involvement Closed acetabular fracture. Closed tibial fracture Fibular fracture. Patellar/astragalar/calcaneal/navicular/wedge/cuboid/metatarsal fracture | Open pelvic fracture (stable ring) Open acetabular fracture. Femoral fracture Open tibial fracture. Open, bi-malleolar fibular fracture | Pelvic ring fracture (complete or incomplete) with bleeding <20% | Pelvic ring fracture (complete or incomplete) with bleeding >20% |
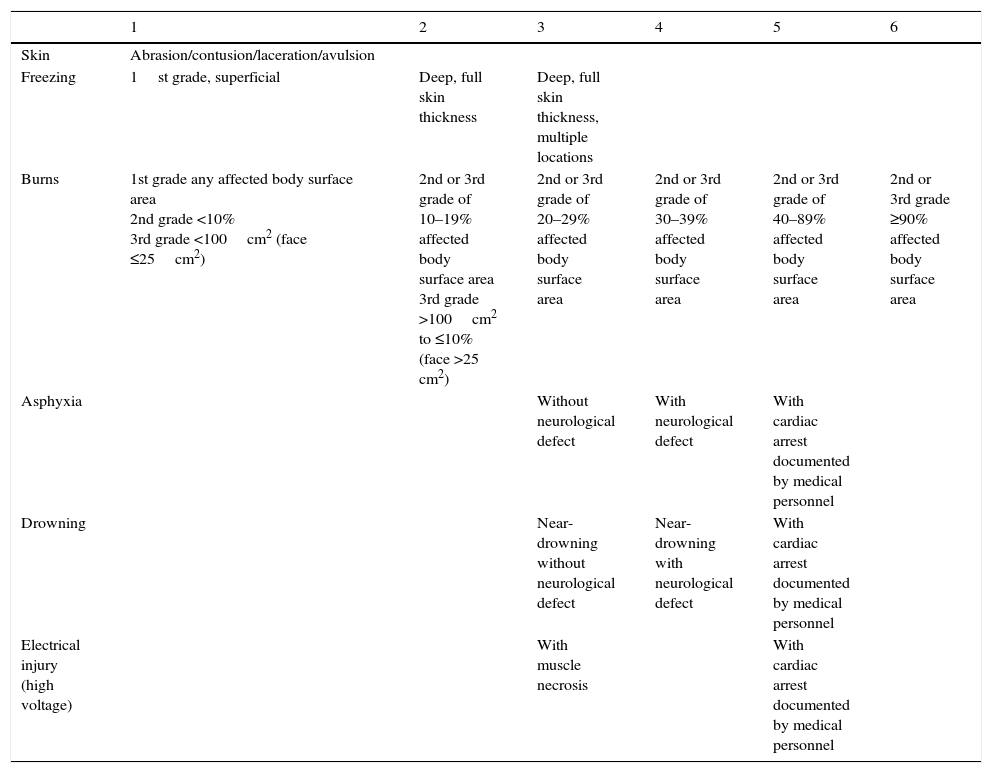
Code in skin and soft tissues:
- Isolated skin damage (without underlying disease) is counted for calculation of the ISS in the region of the skin and soft tissues.
- Skin damage occurring associated to other injuries is coded in the corresponding region, except open fractures, which are coded in the corresponding region and skin damage in the region of the skin and soft tissues.
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| Skin | Abrasion/contusion/laceration/avulsion | |||||
| Freezing | 1st grade, superficial | Deep, full skin thickness | Deep, full skin thickness, multiple locations | |||
| Burns | 1st grade any affected body surface area 2nd grade <10% 3rd grade <100cm2 (face ≤25cm2) | 2nd or 3rd grade of 10–19% affected body surface area 3rd grade >100cm2 to ≤10% (face >25 cm2) | 2nd or 3rd grade of 20–29% affected body surface area | 2nd or 3rd grade of 30–39% affected body surface area | 2nd or 3rd grade of 40–89% affected body surface area | 2nd or 3rd grade ≥90% affected body surface area |
| Asphyxia | Without neurological defect | With neurological defect | With cardiac arrest documented by medical personnel | |||
| Drowning | Near-drowning without neurological defect | Near-drowning with neurological defect | With cardiac arrest documented by medical personnel | |||
| Electrical injury (high voltage) | With muscle necrosis | With cardiac arrest documented by medical personnel |
In addition to the injuries described here, code in skin and soft tissues:
- Isolated skin damage (without underlying disease) is counted for calculation of the ISS in the region of the skin and soft tissues.
- Skin damage occurring associated to other injuries is coded in the corresponding region, except open fractures, which are coded in the corresponding region and skin damage in the region of the skin and soft tissues.
- •
Hemodynamic situation upon admission
- •
Stable: systolic blood pressure >90mmHg during initial trauma care.
- •
Unstable, restored with volume replacement: presentation of systolic blood pressure <90mmHg, requiring only volume replacement (crystalloids or colloids) for normalization.
- •
Shock: presentation of blood pressure <90mmHg requiring volume replacement, blood products and vasoactive drug support for normalization.
- •
Refractory shock: presentation of hypotension refractory to volume replacement measures (crystalloids or colloids), blood products or vasoactive drug support. Activation of massive bleeding protocol at time of initial care.
- •
Coagulopathy: Prolongation of the prothrombin and activated partial thromboplastin times to over 1.5 times the control values, or fibrinogen <150mg/dl or thrombocytopenia (<100,000) at determination in the first 24h after admission.
- •
Rhabdomyolysis: laboratory test determination of CPK >5000U/l.
- •
Respiratory dysfunction: presence of PO2/FiO2 during admission <300.
- •
Early multiorgan failure syndrome: defined as involvement of two or more organs with score of ≥3 on the Sequential-related Organ Failure Assessment (SOFA) scale in the first 72h after trauma.
- •
Late multiorgan failure syndrome: defined as involvement of two or more organs with score of ≥3 on the SOFA scale beyond the first 72h after trauma.
- •
Intracranial hypertension: intracranial pressure increase of >20mmHg, maintained for at least 5min, and requiring guided management.
- •
Renal failure: creatinine elevation of ≥1.5 times the initial value, reduction of glomerular filtration rate by 25% or more, and lowering of urine flow to under 0.5ml/kg/h during 6h or more.
- •
Nosocomial infection: infection acquired in hospital, with the development of symptoms beyond 48h of admission.
Please cite this article as: Chico-Fernández M, Llompart-Pou JA, Guerrero-López F, Sánchez-Casado M, García-Sáez I, Mayor-García MD, et al. Epidemiología del trauma grave en España. REgistro de TRAuma en UCI (RETRAUCI). Fase piloto. Med Intensiva. 2016;40:327–347.
Part of the information contained in this article was presented as a communication at the X Congreso Panamericano e Ibérico de Medicina Crítica y Terapia Intensiva (Madrid, Spain) and at the XXVII Annual Congress of the European Society of Intensive Care Medicine (Barcelona, Spain).