To evaluate the ability of the TRISS and PS14 models to predict mortality rates in our medical system and population.
DesignA retrospective observational study was carried out over a 66-month period.
BackgroundThe study was conducted in the Trauma Intensive Care Unit (ICU) of a third level hospital.
PatientsAll severe trauma patients (Injury Severity Score≥16 and/or Revised Trauma Score<12) aged >14 years were included.
Variables of interestMedical care data were prospectively recorded. The “W” statistic (difference between expected and observed mortality for every 100 patients) and its significance were calculated for each model. Discrimination and calibration were evaluated by means of receiver operating characteristic (ROC) curves, and the Hosmer–Lemeshow test and GiViTI calibration belt, respectively.
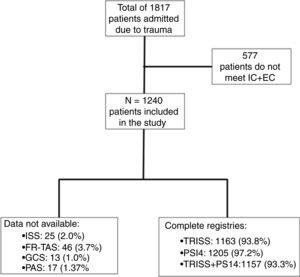
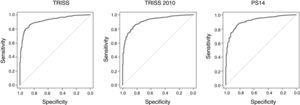
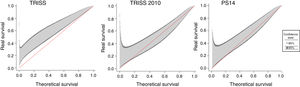
ResultsA total of 1240 patients were included. Survival at hospital discharge was 81.9%. The “W” scores for the TRISS, TRISS 2010 and PS14 models were +6.72 (P<.01), +1.48 (P=.08) and +2.74 (P<.01) respectively. Subgroup analysis revealed significant favorable results for some populations. The areas under the ROC curve for the TRISS, TRISS 2010 and PS14 models were 0.915, 0.919 and 0.914, respectively. There were no significant differences among them (P>.05). Both the Hosmer–Lemeshow test and GiViTI calibration belt demonstrated poor calibration for the three models.
ConclusionsThese models are suitable tools for assessing quality of care in a Trauma ICU, affording excellent discrimination but poor calibration. In our institution, survival rates higher than expected were observed.
Evaluar la capacidad de los modelos TRISS y PS14 para predecir la probabilidad de supervivencia en nuestro sistema de salud y población.
DiseñoDesarrollamos un estudio observacional retrospectivo durante un periodo de 66 meses.
ÁmbitoEl estudio se llevó a cabo en una UCI especializada en traumatología en un hospital urbano de alta complejidad.
PacientesSe incluyeron en el estudio los pacientes mayores de 14 años con traumatismo grave (definido como ISS≥16 y/o RTS<12).
Variables de interésSe calculó el estadístico W (diferencia entre la mortalidad—hospitalaria o a los 30 días para los modelos TRISS o PS14 respectivamente—calculada y observada por cada 100 pacientes) y su nivel de significación para cada modelo. Se realizó un análisis por subgrupos. La calibración y discriminación se evaluaron por medio del test de Hosmer-Lemeshoy y cinturón GiViTI y curvas ROC respectivamente.
ResultadosSe incluyeron 1.240 pacientes. La supervivencia global al alta fue de 81,9%. El estadístico W para los modelos TRISS, TRISS2010 y PS14 fue respectivamente +6,72 (p<0,01), +1,48 (p=0,08) y +2,74 (p<0,01). El AUROC para los citados modelos fue respectivamente 0,915, 0,919 y 0,914, sin que se encontraran diferencias significativas entre ellos. Tanto el test de Hosmer-Lemeshow como el cinturón de calibración GiViTI mostraron escasa calibración en los 3 modelos.
ConclusionesEstos modelos son una herramienta adecuada para la evaluación de la calidad asistencial en una UCI de traumatismo. En nuestro centro las tasas de supervivencia fueron mayores de lo predicho por los modelos.
Despite the progress made in care over the last few years, trauma continues to be the most common cause of death in people under 45 in most countries. An important percentage of these deaths can be prevented.
Monitoring quality of care and outcomes is essential to improve results. Major differences have been reported in the quality of care during the management of severe trauma among different countries and hospitals.
Of the 3 components of the Donabedian's healthcare quality model (structure, process and, outcomes), the assessment of outcomes is probably the ideal method.1
A global measure of the outcomes in severe trauma care is mortality. It depends on the circumstances of trauma and care provided, which justifies the growing interest in the mortality prediction systems that combine multiple variables such as quality indicators. Although over the last 30 years multiple tools have appeared there is no unanimity as to what system is the best predictor of mortality.
Of the different models available the Trauma and Injury Severity Score (TRISS) is the most commonly used. It was developed from the Major Trauma Outcome Study2 in 1983 by the American College of Surgeons Committee on Trauma to develop a reference standard to assess the quality of care in the management of trauma. This tool consists of a multivariate logistic regression system that estimates a probability of survival (PS) from the mechanism, anatomical injuries (assessed by the Injury Severity Score [ISS]), physiological repercussion they produce (assessed by the Revised Trauma Score [RTS]) and the subject's functional reserve (assessed according to his age).
The coefficients applied to estimate PS have been updated from the National Trauma Data Bank that Schluter et al. database built back in 2009.3
Back in 2004, the Trauma Audit & Research Network developed a logistic regression model based on their own registry including age, sex, injury severity score (ISS) and score obtained on the Glasgow scale. In 2014 this model was updated, the coefficients changed, and comorbidity was added to the model (quantified by the modified Charlson Comorbidity Index [mCCI]). The details of the estimates of both models appear in the methodology.
Other European trauma registries that we should mention here are the German (German National Trauma Registry) and the Scandinavian ones (Scandinavian Networking Group for Trauma and Emergency Management). Since 2008 the foundations are being laid to create a new common European registry capable of unifying all existing registries (European Trauma Registry Network).
ObjectivesThe main objective is to confirm the utility of TRISS models (the original one and the one with updated coefficients) and PS14 at a trauma ICU of a tertiary care center.
The secondary objectives are to assess the validity of the survival prediction models mentioned before by calculating their discrimination and calibration, and studying the different profiles of patients (age, sex, type of trauma, and severity of anatomical injuries).
Patients and methodScopeThe study was conducted at the Emergency and Trauma Unit of the Intensive Medicine Service of the Hospital Universitario 12 de Octubre in Madrid, Spain. This unit is an ICU specialized in patients with traumatic disease both from urban and rural environments and assists between 400 and 450 patients every year. Of these, over 200 meet the severity criteria. It has 8 hospitalization beds, a 2-bed emergency care bay plus a resuscitation bay to provide initial trauma and vital emergency care according to standardized international schemes.
The Hospital Universitario 12 de Octubre is a tertiary care center that provides coverage to a population of over 600000 people. It has over 1200 beds, 3 40-bed ICUs, 32 operating rooms, 6 trauma teams, and permanent teams of specialties like general surgery, neurosurgery, maxillofacial, thoracic and heart surgery, interventional arteriography, etc.
Design and populationThis is an observational, retrospective study, from a prospective registry of a cohort of consecutive patients admitted due to trauma from January 2011 through June 2016. The following were established as inclusion criteria: admission due to severe trauma (defined by an ISS≥16 and/or an RTS<12) and age over 14 years. Patients who suffered a trauma more than 24h prior to admission are excluded.
The TRISS methodology is routinely used in the unit as one of the quality control methods.
Study variablesThe study variables were collected prospectively from a registry that included data with the healthcare provided since the accident happened, pre-hospital care, initial hospital care, and ICU admission resulting in final hospital discharge or death.
The demographic variables of our patients are age, sex, and comorbidity factors. The pre-hospital variables collected are the mechanism of trauma; the physiological parameters to estimate the RTS: systolic blood pressure, defined as the lowest one after the trauma during pre-hospital care, the lowest Glasgow Coma Score (GCS) prior to sedation, and the respiratory rate recorded in the pre-hospital care report. If the patient does not receive pre-hospital healthcare, the first physiological parameters are recorded upon arrival at the hospital.
In the early hospital care anatomical injuries were identified and coded using the Abbreviated Injury Scale (AIS) codes from the Association for the Advancement of Automotive Medicine from 2005 updated in 2008. The maximum AIS (MAIS) were collected from the different anatomical regions and the ISS was calculated within the first 24h.
The patients were followed from the moment they were admitted to the ICU until hospital discharge or death. Their progression and stay at the ICU, and their progression and stay at the hospital floor were recorded.
Most of the study variables were collected prospectively and entered into a Microsoft Access database. Comorbidity was added to the registry to estimate the mCCI. The next step was to review the patients’ past medical histories to identify the 21 diseases to which the index assigns a not null score.
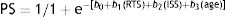
Estimating the probability of survival for each modelIn the TRISS model the probability of survival is estimated using the following equation:
b0 is an independent constant. b1, b2, and b3 respectively are the coefficients associated with RTS, ISS, and age, that take different values in closed and penetrating traumas.RTS is a linear combination of the 3 elements that make up the RTS (respiratory rate, GCS, and systolic blood pressure).
The probability of survival of the PS 14 model is estimated with the following expression:
where b is the sum of the coefficients corresponding to each score on the Glasgow coma score, age, sex, and mCCI, a modification of the ISS using the fractional polynomial method.Ethical aspectsData analysis was conducted following an extract of the main registry kept by the leading researcher that does not include the patients’ personal details to guarantee confidentiality. Approval was obtained from the ethics committee of the research (#CEI 17/188).
Management of data and statistical analysisCategorical variables were expressed as absolute frequencies and relative frequencies. Quantitative variables with normal distribution were expressed as mean±standard deviation. Quantitative variables without a normal distribution were expressed as median with interquartile range 25–75.
To compare the survival observed and predicted the method developed in the Major Trauma Outcome Study was used (final outcome-based evaluation).4 According to this method, such comparison is conducted using Kendall's W-statistic that indicates the difference of survivors for every 100 patients included with respect to the number predicted by the model. It can take positive values if the survival observed is greater than the one estimated, and negative values if the survival registered is lower than the one predicted. Using the Z-statistic it is possible to estimate the confidence intervals of Kendall's W-statistic.
To estimate the validity of the models 2 components were taken into account: discrimination and calibration. Regarding the former, the areas under the ROC curve were calculated in the different models, and they were compared to one another using the DeLong statistical test. To estimate calibration, the Hosmer–Lemeshow goodness of fit test was used.
To identify the intervals where there are calibration errors in the models, calibration was studied using the GiViTI calibration belt. This analysis looks into the relation between the outcomes observed and calculated through the adjustment of one polynomial function upon which an 80% and 95% confidence interval is calculated. Defective calibration intervals are described for the models when the 95% confidence interval does not contain the bisector.5
The statistical software package for Windows SPSS 22.0 and R 3.4.3 were used.
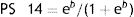
ResultsDuring the period of study 1817 trauma patients were admitted to the unit (Fig. 1). Of these patients, 1240 (68.24%) met the inclusion criteria. All the patients’ personal information and demographic data are shown in the main registry. However, based on the information of their past medical history, the reports from other centers and pre-hospital services, it is not possible to estimate the ISS in 25 patients, the RTS in 48 patients, the TRISS in 77 patients, and the PS14 in 35 patients, which in relative terms means losses <10%.
The patients included in the study are mostly males (80%) with an mean age of 40 years (29.7–55.0) (Table 1).
Subgroup analysis of age, type of trauma, damage to anatomical region, and injury severity score (ISS) for the updated TRISS and PS14 models.
| N (%) | Survivors | ∑Pi | Dead | W | Z | P | |||
|---|---|---|---|---|---|---|---|---|---|
| TRISS model | Age | <55 | 873 (75.1) | 776 | 746.07 | 97 | 3.4284 | –3.7974 | P<.01 |
| ≥55 | 290 (24.9) | 202 | 206.69 | 88 | −1.6172 | 0.7854 | .4322 | ||
| <26 | 210 (18.1) | 189 | 182.71 | 21 | 2.9952 | −1.7220 | .0851 | ||
| >70 | 114 (9.8) | 59 | 79.108 | 55 | −17.6386 | 5.1753 | P<.01 | ||
| Sex | Males | 925 (79.5) | 790 | 762.73 | 135 | 2.9481 | −3.1021 | P<.01 | |
| Women | 238 (20.5) | 188 | 190.02 | 50 | −0.8487 | 0.4465 | .6552 | ||
| Type | Closed | 1.062 (91.3) | 889 | 866.28 | 173 | 2.1394 | −2.4073 | P<.05 | |
| Penetrating | 101 (8.7) | 89 | 86.47 | 12 | 2.5050 | −0.8824 | .3775 | ||
| MAIS | TBI MAIS>3 | 402 (34.6) | 265 | 268.13 | 137 | −0.7786 | 0.4267 | .6696 | |
| Thoracic t. MAIS>3 | 234 (20.12) | 186 | 164 | 48 | 9.4017 | −4.3693 | P<.01 | ||
| Abdominal t. (MAIS>2) | 171 (14.7) | 136 | 127.49 | 35 | 4.9766 | −2.0800 | P<.05 | ||
| Spinal t. (MAIS>3) | 59 (5.1) | 46 | 41.19 | 13 | 8.1525 | −2.1255 | P<.05 | ||
| Pelvic t. (MAIS>3) | 201 (17.28) | 176 | 157.89 | 25 | 9.0100 | −4.3107 | P<.01 | ||
| ISS | ISS <16 | 135 (11.61) | 131 | 129.88 | 4 | 0.8296 | −0.5347 | .5929 | |
| ISS 16–24 | 298 (25.6) | 290 | 285.83 | 8 | 1.3993 | −1.2994 | .1938 | ||
| ISS 25–34 | 176 (15.1) | 148 | 146.38 | 28 | 0.9205 | −0.3866 | .6990 | ||
| ISS >34 | 237 (20.4) | 146 | 121.35 | 91 | 10.4008 | −3.9992 | P<.01 | ||
| PS14 model | Age | <55 | 902 (74.9) | 799 | 776.07 | 103 | 2.5421 | −2.5865 | P<.01 |
| ≥55 | 303 (25.2) | 211 | 198.85 | 92 | 4.0099 | −2.0144 | P<.05 | ||
| <26 | 216 (17.9) | 195 | 193.19 | 21 | 0.8380 | −0.4958 | .6200 | ||
| >70 | 122 (10.1) | 64 | 61.1 | 58 | 2.3770 | −0.6827 | .4948 | ||
| Sex | Males | 963 (79.9) | 819 | 789.11 | 144 | 3.1038 | −3.3630 | P<.01 | |
| Women | 242 (20.1) | 191 | 187.815 | 51 | 1.3161 | −0.6660 | .5054 | ||
| Type | Closed | 1.102 (91.5) | 919 | 881.87 | 183 | 3.3693 | −3.7820 | P<.01 | |
| Penetrating | 103 (8.55) | 91 | 95.058 | 12 | −3.9398 | 1.7345 | .0828 | ||
| MAIS | TBI MAIS>3 | 421 (34.9) | 277 | 264.22 | 144 | 3.0356 | −1.6388 | .1013 | |
| Thoracic t. MAIS>3 | 242 (20.1) | 193 | 186.109 | 49 | 2.8475 | −1.4345 | .1514 | ||
| Abdominal t. (MAIS>2) | 172 (14.3) | 138 | 137.42 | 34 | 0.3372 | −0.1349 | .8927 | ||
| Spinal t. (MAIS>3) | 62 (5.1) | 49 | 47.31 | 13 | 2.7258 | −0.7382 | .4604 | ||
| Pelvic t. (MAIS>3) | 206 (17.1) | 183 | 169.52 | 23 | 6.5437 | −3.3155 | P<.01 | ||
| ISS | ISS<16 | 133 (11.05) | 129 | 124.77 | 4 | 3.1805 | −1.7559 | .0791 | |
| ISS 16–24 | 310 (25.75) | 301 | 295.38 | 9 | 1.8129 | −1.7031 | .0885 | ||
| ISS 25–34 | 183 (15.2) | 152 | 144.14 | 31 | 4.2951 | −1.8518 | .0641 | ||
| ISS>34 | 241 (20.0) | 147 | 137.11 | 94 | 4.1037 | −1.6291 | .1033 |
Regarding their origin, 969 of them (78%) were brought by the pre-hospital services, 149 (12%) were transferred from the ER, and 121 patients (10%) were secondary transfers from other centers.
A clear prevalence of closed traumas can be seen (92%) as opposed to penetrating traumas (8%). The most common injury mechanism in this cohort is traffic accidents (42%) followed by autolysis, and aggression (12% and 10%, respectively).
Before being admitted to the hospital, low blood pressure (SBP<90mmHg) is confirmed in 357 patients (29%), Glasgow scale scores≤8 in 414 patients (34%), and an RTS score<12 points in 834 patients (67%). The mean ISS during admission of the overall sample was 26.02. During pre-hospital care, 585 patients (47%) required secure airway management. During their ICU stay a total of 190 patients died (15.32%). Of the remaining 1050 patients who were discharged, 976 (79%) were transferred to the hospital floor, and 19 of them eventually died (1.95%).
The W-statistic values for the TRISS, updated TRISS, and PS14 models applied to our global population with their 95% confidence interval were 6.72 (5.03–8.41), 1.47 (−0.19 to 3.15), and 2.74 (1.1–4.39), respectively (Fig. 2).
To study the ability to discriminate of each prediction model, the ROC curves were obtained (Fig. 3). The values of the area under the ROC curve (AUC) for the TRISS, updated TRISS, and PS14 models with their corresponding 95% confidence intervals were 0.91 (0.89–0.93), 0.91 (0.89–0.93), and 0.92 (0.90–0.94), respectively. After using the DeLong test to compare the AUC values of the different models, no significant differences were found between the TRISS model and the classic and updated coefficients (P=.44), between the classic TRISS model and the PS 14 (P=.75) or between the TRISS model with updated coefficients and the PS 14 (P=.67).
The Hosmer–Lemeshow statistical values for the TRISS, updated TRISS, and PS14 models were 29.9, 56.2, and 49.9, respectively; all of them with P values <.05.
The GiViTI calibration belt for each model (with representation of the 80% and 95% confidence interval) is shown in Fig. 4.
Data of the subgroup analysis are shown in Table 1.
DiscussionThe 3 models share high discriminating capacity and low calibration. This pattern had already been reported. The AUROC values are consistent with those from other studies conducted in our field.6 The low calibration capacity of the TRISS model had already been reported, and it is common to other models applied in the intensive medicine setting.7,8
Regarding the TRISS 2010 model, other authors have seen that mortality rate is underestimated when it is <60% and overestimated when it is >60%.6 The calibration belt obtained in our study for this model is consistent with this tendency seen. Underestimating the severity of the patients’ severe TBI patients and that of old patients is another limitation reported by the authors. This limitation can be responsible for the unfavorable difference seem between the survival observed and predicted in patients >70 years, which was not seen when model PS14 was used. Probably the latter model is a better predictor of severity in these patients. On one hand, it is not based on a dichotomic division of age (it rather assigns different coefficients to 8 ranges of age). On the other hand, it includes comorbidity as one of the variables, which is more common in these patients. In this sense, treating age as a continuous variable would be associated with better calibration values. However, the NORMIT model built from the Norwegian registry where age is included as a cubic (continuous) function also shows poor calibration values.7
Another aspect that can be associated with low the calibration values of both models is the use of the ISS scale to quantify the severity of the injuries (that overlooks the presence of several serious injuries in the same anatomical region). A possible alternative to this scale would be the use of the NISS scale in the prediction model (as it is the case of the NORMIT scale developed from the Norwegian model).7 Other simpler survival prediction models such as the BIG (that don’t use the ISS calculation) show lower discriminating capabilities.9
The Glasgow scale score stands out among the multiple elements involved in PS calculation in both models. However, it has been criticized due to its complexity, subjectivity, and low reproducibility.10 In the case of trauma patients, this scale is often affected by artifacts resulting from alcohol or drug abuse.7
We should mention here that none of the models studied included analytical values as it occurs with the German model (RISC) that incorporates base excess and prothrombin activity and shows discriminating capabilities that can be compared to the TRISS system.11
The disparity in the differences seen when applying the classic TRISS methodology and TRISS 2010 methodology can be explained by the 30-year difference that separates both scales, during which trauma care has improved substantially.
When comparing our results to those of a contemporary British population using the PS14 model, we saw a favorable statistically significant difference.
The group of old patients is especially important given that they it is a growing group in our center. This group is characterized by having higher mortality rates compared to the overall mortality rate. In our series, the mortality rate of patients >70 years was 45%, similar to that reported by other Spanish groups. An unfavorable survival difference was seen in our center when the TRISS methodology was used that was not confirmed when the PS14 model was used.12 This inconsistency is probably associated with the calibration of the models for this population subgroup as we have already mentioned.
Regarding the female population, it is possible to see higher mortality rates compared to males (RR, 1.47, 95%CI, 1.05–2.07) despite the fact that there are no statistically significant differences in age, ISS, GCS or RTS. These results may be due to differences in the injury mechanisms or patterns or to sex related different responses to trauma. In this sense, mortality and side effects have been postulated in women with TBI compared to males. This may be associated with hormonal, metabolic (that condition the response to treatment), and functional factors of the central nervous system.13
We saw an unfavorable difference in the mortality rate associated with penetrating trauma, which does not reach statistical significance in the PS14 prediction model. This difference can be due to several factors. On the one hand, it may be due to the scarce percentage of patients it represents with respect to the overall number of patients, which speaks of much less experience in the healthcare provider. On the other hand, it can be linked with a calibration error of the predictive model, something that has already been described by other authors.14
In patients with severe TBI (depending on the injuries, defined as MAIS>3) in our center we obtain mortality results that are consistent with the American ones and slightly better than Anglo-Saxon results. The overall mortality of these patients (34%) is acceptable according to the trauma quality markers proposed by SEMICYUC.1
Another subgroup that stands out is that of patients with severe pelvic trauma (defined as MAIS in such region >3), where survival is strikingly higher compared to the one expected for both models. We believe that these results can be associated with our multidisciplinary protocol agreed with prehospital, interventional radiology, trauma and surgery units for a fast, systematic, effective, and comprehensive care of these patients.
This study has some limitations. It was a single-center study whose results probably cannot be generalized to the healthcare provided in other units.
Because this is a retrospective study across time, we are facing problems such as data and patient loss. The variable that is more often incorrectly recorded is respiratory rate, a crucial parameter for the TRISS model. This associated a small but tolerable loss of the patients included initially (3.7%), but it could jeopardize its internal validity. Arterial blood pressure is another variable that was incorrectly recorded partly due to its changing character during initial care.
Lastly, we should not forget that the methodologies used calculate the probability of survival based on the results seen in US (TRISS) and UK hospitals (PS14). The use of such methodologies to assess the ICU of a Madrid tertiary care center has some limitations given the international differences among centers. The resources, experience, type of trauma and patients, and healthcare protocols can vary significantly from one country to the next, which can be a confounding factor if we use it in our setting.
In conclusion, with the objective of assessing the quality of the chain of healthcare provided for the management of patients with severe trauma at our hospital, we tried to compare our own center to the international standards. For the lack of a single international model, and given the limitations found in our study, we believe that the best thing to do would be to create a methodology for evaluation purposes from the data obtained from Spanish hospital ICUs and then compare the results more reliably. A trauma registry would be of special interest in the development of such methodology, and its utility has already been recognized by the WHO.12 Several initiatives have been published in our country being the RETRAUCI project (developed by SEMICYUC1 Trauma and Neurointensive Care Working Group) the most important of all.
Conflicts of interestNone reported.
Please cite this article as: Sainz Cabrejas J, García Fuentes C, García Juarranz C, González López AM, Maure Blesa L, Montejo González JC, et al. Valoración de la calidad asistencial al traumatismo grave mediante comparación con estándares internacionales. Med Intensiva. 2020;44:325–332.