The favorable evolution of critically ill patients is often dependent on time-sensitive care intervention. The timing of transfer to the intensive care unit (ICU) therefore may be an important determinant of outcomes in critically ill patients. The aim of this study was to analyze the impact upon patient outcome of the length of stay in the Emergency Care Department.
DesignA single-center ambispective cohort study was carried out.
SettingA general ICU and Emergency Care Department (ED) of a single University Hospital.
PatientsWe included 269 patients consecutively transferred to the ICU from the ED over an 18-month period.
InterventionsPatients were first grouped into different cohorts based on ED length of stay (LOS), and were then divided into two groups: (a) ED LOS ≤5h and (b) ED LOS >5h.
VariablesDemographic, diagnostic, length of stay and mortality data were compared among the groups.
ResultsMedian ED LOS was 277min (IQR 129–622). Patients who developed ICU complications had a longer ED LOS compared to those who did not (349min vs. 209min, p<0.01). A total of 129 patients (48%) had ED LOS >5h. The odds ratio of dying for patients with ED LOS >5h was 2.5 (95% CI 1.3–4.7). Age and sepsis diagnosis were the risk factors associated to prolongation of ED length of stay.
ConclusionsA prolonged ED stay prior to ICU admission is related to the development of time-dependent complications and increased mortality. These findings suggest possible benefit from earlier ICU transfer and the prompt initiation of organ support.
La evolución de los pacientes críticos se relaciona con intervenciones que dependen del tiempo. Por tanto, el momento de traslado de los pacientes graves a la UCI puede relacionarse con el pronóstico. El objetivo de este estudio fue analizar el impacto de la duración del ingreso en Urgencias sobre el pronóstico de los pacientes.
DiseñoEstudio de cohortes ambispectivo de centro único.
ÁmbitoUCI polivalente y Servicio de Urgencias de un Hospital Universitario.
PacientesUn total de 269 pacientes ingresados en la UCI consecutivamente desde urgencias durante 18meses.
IntervencionesSe agrupó a los pacientes en cohortes según la duración del ingreso en urgencias. Después se dividieron en 2 grupos: a)estancia en urgencias ≤5h, y b)estancia en urgencias >5h.
VariablesDemográficas, diagnóstico, estancia, mortalidad.
ResultadosMediana de estancia en urgencias de 277min (RIC129-622). Los pacientes que desarrollaron complicaciones en la UCI tuvieron mayor estancia en Urgencias que aquellos sin complicaciones (349 vs. 209min, p<0,01). Un total de 129 pacientes (48%) tuvieron un ingreso en urgencias >5h. La odds ratio para el fallecimiento hospitalario de los pacientes con un ingreso en urgencias >5h fue de 2,5 (IC del 95%, 1,3 a 4,7). La edad y la sepsis fueron los factores de riesgo asociados a la prolongación del ingreso en urgencias.
ConclusionesUna estancia prolongada urgencias antes del ingreso en la UCI se relaciona con el desarrollo de complicaciones que dependen del tiempo y con la mortalidad. Estos hallazgos sugieren un beneficio del ingreso precoz en la UCI y del inicio de soporte orgánico sin retraso.
The time lapse between the onset of organ dysfunction and the initiation of appropriate treatment may play a decisive role in outcome for critically-ill patients. In fact, patients who have already developed multiple organ dysfunction syndrome (MODS) predict a very poor outcome,1 and a subsequent intensive care unit (ICU) admission may well prove futile. Successful evolution of these patients often depends on time-sensitive care interventions capable of repairing the damaged organs. Among such interventions are aggressive resuscitation after major trauma, thrombolytic agent therapy in stroke patients, early rapid fluid resuscitation and appropriate antibiotics in septic shock, or artery revascularization in myocardial infarction.2–6 Thus the timing of transfer to the ICU to receive life-sustaining therapies may be an important determinant of outcome for critically-ill patients admitted to the emergency department (ED). Delayed ICU admissions have been associated with higher mortality.7–9 Delays of four or more hours in ICU transfers following physiological deterioration have been associated with a 3.5 times higher mortality rate.10
Few studies have investigated the impact on critically-ill patients of ED length of stay prior to ICU admission.11 However, solid data exist concerning already severely-ill patients having to wait in the emergency department for ICU bed availability.7,12,13 These studies confirm that waiting time is associated with poorer outcome, although there is still little data to support the use of any particular time frame as an indicator of quality of care. Outside of the ICU and postoperative care areas, critical care is more frequently delivered in the emergency department than in any other area in the hospital. Hence the increasing focus on “critical care without walls”,14,15 whereby critically-ill patients are increasingly being cared for in the emergency department.16
For emergency department patients, the timing of transfer to the ICU may be an important determinant of outcomes. Therefore, the purposes of this study were to identify factors likely to increase emergency department length of stay, and analyze the relationship between ED length of stay and the clinical course of disease in patients subsequently admitted to the ICU.
Patients and methodsStudy design and study populationWe present a prospective cohort study of all patients consecutively transferred to the ICU from the emergency department from October 2011 to March 2013.
During the study period, there were 782 ICU admissions. We excluded the following patients: (a) patients transferred directly by the pre-hospital emergency medical services to the ICU (n=93); (b) inter-hospital transfers (n=84); (c) transfers from wards (n=202); and (d) transfers from operating rooms (n=114). A total of 289 patients from the emergency department were considered as potential candidates for inclusion in the final analysis. However, the following exclusions criteria were applied: (a) patients transferred to a ward within 24h of ICU admission (n=14) and (b) and incomplete follow-up patients (n=4). Thus 269 patients made up the final study population.
Our ICU is a closed 17-bed unit staffed by seven highly-trained intensivists. The emergency department area consists of a 37-bed main unit, a 40-bed observation unit and a two-bed urgent care unit. ED patients are treated by trained physicians and consultants from different medical or surgical specialties. Intensivists are consulted when patients need intensive therapies of the ICU, and the final decision regarding ICU admission is then made by the senior intensivist. Patients are treated by intensivists, according to ICU protocols, when they arrived in the intensive care unit.
The study protocol was approved by the Ethics Committee of our institution, and the informed consent requirement was waived. Patient anonymity was protected at all times throughout the study period.
Data collectionAll interventions subsequent to ICU admission were prospectively recorded. ED admission data were obtained from the emergency department records. Follow-up continued until hospital discharge.
The following data were collected: day of ICU admission; age; sex; comorbidities (arterial hypertension, diabetic, cardiovascular, respiratory, renal or hepatic chronic disease, acquired immunosuppression and solid or hematological cancer); procedures or treatment in the ICU (mechanical ventilation, central venous catheterisation, dialysis, vasoactive drugs, sedation longer than 24h, and urgent surgical intervention); and diagnostic category classified as: (a) sepsis; (b) neurocritic (intracranial hemorrhage, stroke, status epilepticus, other); (c) respiratory (acute exacerbation of asthma or chronic obstructive pulmonary disease, pulmonary embolism, other); (d) gastrointestinal (pancreatitis, gastrointestinal bleeding, acute hepatitis or liver complications); (e) renal/metabolic (acute renal failure, diabetic ketoacidosis, other metabolic decompensation); and (d) miscellaneous. All physiological and laboratory data needed to calculate the Acute Physiology and Chronic Health Evaluation (APACHE) II score within the first 24h of ICU admission were recorded.17
Outcome measurements were as follows: (a) ICU complications [shock (when vasoactive drugs are needed to avoid tissue hypoperfusion), acute heart failure (according to chest radiography image and/or monitoring of ventricular filling pressures or cardiac index), acute respiratory distress syndrome (ARDS) or acute renal failure based on definitions previously used,18,19 coagulopathy based on local laboratory tests, and multiple organ failure]; (b) ICU and hospital length of stay (LOS); and (c) ICU and hospital mortality.
Emergency department length of stay, defined as the period from the patient's ED arrival to their ICU arrival, was measured in minutes by the ICU team and recorded for all patients. The relationship between ED LOS and outcome was examined in two ways. Firstly, patients were grouped into six cohorts according to the number of hours spent in the emergency department: 0–2, 2–4, 4–6, 6–12, 12–24, and more than 24h. Secondly, patients were divided into two groups according to the median ED LOS: (a) those with an ED LOS ≤5h and (b) those with an ED LOS >5h.
Statistical analysisStatistical analysis of data was performed using STATA/SE statistical package, version 10.0. Continuous variables were presented as mean and standard deviation (SD) if normally distributed, otherwise as median with interquartile range (IQR). Categorical variables were presented as a percentage. Normality of distribution was tested with the Kolmogorov–Smirnov test. Continuous variables were compared using the Student's t or Mann–Whitney U tests, as appropriate. Categorical variables were compared using a chi-squared test or Fisher's exact test for non-normally distributed data. Multivariate stepwise logistic regression (backward elimination) approach was used to identify potential risk factors associated with prolonged emergency department length of stay. The median value of ED LOS (5h approximately) was used as a cut-off to transform the data into categorical variables. Only variables with p<0.20 in the univariate analysis were included in the multivariate analysis, and results are presented as odds ratio with 95% confidence interval. A Kaplan–Meier curve was performed to analyze patient survival. All two-sided p-values less than 0.05 were considered statistically significant.
ResultsA total of 269 patients was the final study population. Patients were mainly male (59%), with a mean age of 53±17 years and a mean APACHE II score of 16±7 points. Median time spent in the emergency department before ICU transfer was 277min (IQR 129–622). Patients were grouped into six cohorts based on ED LOS as follows: 61 patients (23%) under 2h, 60 patients (22%) from 2 to 4h, 30 patients (11%) from 4 to 6h, 62 patients (23%) from 6 to 12h, 45 patients (17%) from 12 to 24h, and 11 patients (4%) more than 24h. The majority of ICU admissions occurred in the daytime (72%, 195/269) and on a week day (66%, 178/269).
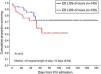
Fig. 1 shows the relation between ED length of stay and different diagnoses. As can be seen, patients with sepsis or gastrointestinal diagnoses were more likely to have longer ED LOS (p<0.001). Neither the day of ICU admission (weekday vs. weekend) nor the shift (day vs. night) were associated with ED length of stay: weekday 276min (IQR 120–622) vs. weekend 288min (IQR 145–664), p=0.59; and day 266min (IQR 123–617) vs. night 395min (IQR 170–674), p=0.14, respectively.
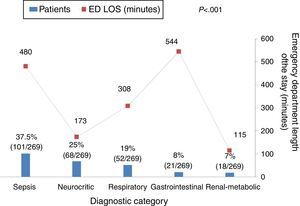
Patient outcome was related to ED length of stay. Table 1 shows the differences in ED length of stay for that did or did not require organ support after admission to the ICU. The subgroup of patients that required vasoactive or dialysis support had a longer ED LOS than patients that did not. In addition, Table 2 shows that the subgroup of patients who developed ICU complications had a longer ED LOS compared to those without complications (349min vs. 209min, p<0.01). Shock, renal failure, coagulopathy and multiple organ failure in particular were time-dependent complications (Fig. 2).
ICU organ support.
| Type of support | Patient with ICU support | Patient without support | p-Value | ||
|---|---|---|---|---|---|
| n | Median ED LOS | n | Median ED LOS | ||
| Mechanical ventilation | 141 | 261 (120–576) | 128 | 270 (128–600) | 0.14 |
| Vasoactive drugs | 126 | 364 (175–693) | 143 | 232 (111–357) | 0.004 |
| Dialysis | 43 | 420 (201–678) | 226 | 267 (125–621) | 0.03 |
| Sedation longer than 24h | 102 | 275 (132–632) | 167 | 280 (128–623) | 0.87 |
| Central venous catheter | 162 | 307 (140–670) | 107 | 243 (122–586) | 0.22 |
| Urgent surgery | 29 | 228 (133–522) | 240 | 290 (128–667) | 0.23 |
Data shown as n (number of patients) and median of minutes (IQR).
ED LOS: emergency department length of stay.
ICU time-dependent complications.
| Complication category | Patient with complication | Patient without complication | p-Value | ||
|---|---|---|---|---|---|
| n | Median ED LOS | n | Median ED LOS | ||
| Any complication | 173 | 349 (147–719) | 96 | 209 (115–499) | 0.002 |
| Shock | 77 | 413 (178–768) | 192 | 239 (117–589) | 0.003 |
| Acute heart failure | 50 | 420 (177–779) | 219 | 275 (126–590) | 0.10 |
| ARDS | 41 | 379 (147–583) | 228 | 276 (126–661) | 0.48 |
| Renal failure | 83 | 480 (203–888) | 186 | 225 (114–539) | <0.001 |
| Coagulopathy | 69 | 480 (262–892) | 200 | 230 (114–539) | <0.001 |
| Multiple organ failure | 55 | 470 (203–910) | 214 | 239 (120–587) | 0.003 |
Data shown as n (number of patients) and median of minutes (IQR).
ED LOS: emergency department length of stay; ARDS, acute respiratory distress syndrome.
Time-dependent complication rate among critically-ill patients grouped by emergency department length of stay prior to ICU admission. These figures show increase in complication rates according to ED waiting time. (A) There is a tendency of increase in shock rate with longer ED LOS (but no significant, p=0.10). (B) There is a significant tendency of increase in renal failure rate with longer ED LOS (p=0.001). (C) There is a significant tendency of increase in coagulopathy rate with longer ED LOS (p<0.001). (D) There is a significant tendency of increase in multiple organ failure rate with longer ED LOS (p=0.009).
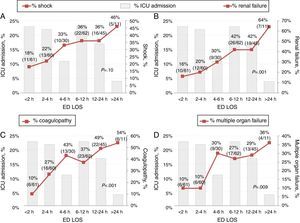
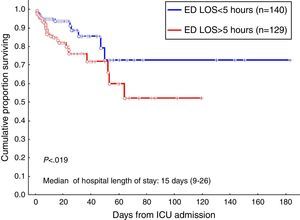
Because a worse patient outcome was associated with the time in the emergency department, patients were divided using a 5h cut-off. Table 3 shows the characteristic and outcome data of patients. A total of 129 patients (48%) had an ED LOS >5h. The results of multiple logistic regression analysis to determine which characteristics are independently associated with the prolongation of ED LOS are shown in Table 3. As can be seen, age and a sepsis diagnosis are the risk factors to have a prolonged emergency department stay prior to transfer to the ICU. In addition, sepsis was the most frequent diagnosis in patients older than 65 years (n=67) than in patients under 65 years (n=202), 51% (34/67) versus 33% (67/202), p=0.008; without different in others diagnosis. Finally, the odds ratio for in-hospital death for patients with an ED LOS higher than 5h was higher compared to patients with an ED LOS shorter than 5h [2.5 (95% CI, 1.3–4.7) versus 0.8 (95% CI, 0.7–0.9)]. Hospital survival probability from ICU admission according to the time in ED was estimated using the Kaplan–Meier method. With a median time of stay in hospital of 15 days, the probability of being alive at hospital discharge was 93.5% and 84.8% in ED LOS ≤5h group and ED LOS >5h group, respectively (Fig. 3, log-rank p<0.019).
Characteristics and outcome patients using a 5h cut-off. Multivariable analysis to identify factors associated with ED LOS ≥5h.
| ED LOS <5h | ED LOS ≥5h | p-Value | |
|---|---|---|---|
| (n=140) | (n=129) | ||
| Clinical characteristics | |||
| Age (years) | 50±17 | 57±16 | <0.001* |
| Sex: male | 81 (58%) | 77 (60%) | 0.74 |
| APACHE II (points) | 15±7 | 16±8 | 0.20* |
| Comorbidities | |||
| Arterial hypertension | 48 (34%) | 46 (36%) | 0.8 |
| Cardiovascular | 15 (11%) | 22 (17%) | 0.09* |
| Diabetic | 23 (16%) | 19 (15%) | 0.82 |
| Respiratory | 28 (20%) | 30 (23%) | 0.55 |
| Renal | 6 (4%) | 10 (8%) | 0.17* |
| Hepatic disease | 17 (12%) | 22 (17%) | 0.16* |
| Cancer | 15 (11%) | 21 (16%) | 0.12* |
| Acquired immunosuppression | 18 (13%) | 19 (15%) | 0.39 |
| Diagnostic category | |||
| Sepsis | 36 (26%) | 65 (50%) | <0.001* |
| Neurocritic | 49 (35%) | 19 (15%) | <0.001* |
| Respiratory | 25 (18%) | 27 (21%) | 0.53 |
| Gastrointestinal | 9 (6%) | 12 (9%) | 0.35 |
| Renal-metabolic | 15 (11%) | 3 (2%) | 0.003 |
| Miscellaneous | 6 (4%) | 3 (2%) | 0.34 |
| Weekend day admission | 46 (33%) | 45 (35%) | 0.73 |
| Night-time admission | 34 (24%) | 40 (31%) | 0.20* |
| Clinical outcome | |||
| Mechanical ventilation | 80 (57%) | 61 (74%) | 0.07 |
| Days of MV | 3 (1–9) | 6 (3–12) | 0.009 |
| Dialysis | 16 (11%) | 27 (21%) | 0.02 |
| Vasoactive drugs | 57 (41%) | 69 (54%) | 0.02 |
| Any complication | 78 (56%) | 95 (74%) | <0.001 |
| Shock | 31 (22%) | 46 (36%) | 0.01 |
| Heart failure | 22 (16%) | 28 (22%) | 0.13 |
| ARDS | 19 (14%) | 22 (17%) | 0.27 |
| Renal failure | 27 (19%) | 56 (43%) | <0.001 |
| Coagulopathy | 23 (16%) | 46 (36%) | <0.001 |
| Multiple organ failure | 18 (13%) | 37 (29%) | 0.001 |
| ICU LOS (days) | 4 (2–9) | 5 (3–9) | 0.20 |
| Hospital LOS (days) | 15 (9–27) | 16 (10–25) | 0.51 |
| ICU mortality | 10 (7%) | 23 (18%) | 0.006 |
| Hospital mortality | 12 (9%) | 28 (22%) | 0.003 |
| Odds ratio | 95% CI | p-Value | |
|---|---|---|---|
| Multivariate analysis of factors associated with ED LOS ≥5h | |||
| Age | 1.02 | 1.0–1.1 | 0.004 |
| Sepsis diagnosis | 2.63 | 1.6–4.5 | <0.001 |
Data shown as number of patients (percentage), mean (SD) or median (IQR).
Multivariate analysis: (*) variables included in the analysis; CI: confidence interval; APACHE: Acute Physiology and Chronic Health Evaluation; MV: mechanical ventilation; ARDS: acute respiratory distress syndrome; ED LOS: emergency department length of stay; ICU: intensive care unit.
Survival curve of patients admitted to the ICU from the emergency department according to ED LOS using the Kaplan–Meier method. Vertical axis represents estimated probability of survival. Horizontal axis represents time in days after ICU admission. Blue line indicates patients with ED LOS <5h and red line indicates patients with ED LOS >5h (log-rank p<0.019).
The present study demonstrates that approximately 20% of critically-ill patients spend more than 12h in the emergency department before being admitted to the ICU. Our results suggest that prolonged emergency department boarding times (>5h) are associated with poor clinical patient outcomes such as time-dependent complications and reduced hospital survival. Critically-ill patients constitute a significant and growing proportion of emergency department practice. These patients are likely to remain in the emergency department for significant periods of time.20 Previous articles have associated emergency department length of stay and poor outcomes in critically-ill patients with long waiting times in the emergency department due to ED crowding21–23 or non-availability of ICU beds.7,12,13 In those cases, patients tended to stay in the ED longer and timely therapeutic interventions were delayed with an increased severity of illness as a result.21,22 In our study, hospital survival rates were higher among patients with an ED length of stay of under 5h (p<0.019). Likewise, patients spending over 5h in the emergency department before being admitted to ICU had a nearly three times greater risk of dying than those with a shorter ED stay. In a previous study, Cardoso et al.9 demonstrated that each hour of waiting prior to ICU admission was independently associated with a 1.5% increased risk of ICU death. In their study, nearly 70% of ICU admissions were referrals from the emergency department. Thus, to some extent, emergency department length of stay can be used as a surrogate marker for adverse outcome in critically-ill medical patients subsequently transferred to the ICU.
We found that patients with longer wait times in the emergency department experienced greater delays in the initiation of advanced organ support, such as vasoactive drugs or dialysis, in the ICU. This treatment delay may have contributed to the development of time-dependent complications and a subsequently higher ICU mortality rate. Shock, renal failure, coagulopathy and multiple organ failure are the complications associated with a prolonged stay in the emergency department. The care provided for critically-ill patients during their emergency department stay and subsequently in the ICU impacts on the progression of organ failure and mortality. Though the ED stay is relatively short compared with the overall length of hospitalization, our data emphasize the idea that time to treatment in the ICU has a profound effect on outcome. Our results are consistent with previous studies which demonstrate the importance of providing early specialized intervention to prevent organ dysfunction. An aggressive resuscitation performed during the “golden hour” after a major trauma,3 for example, offers the highest chance of an improved outcome. Similarly, early goal-directed therapy and early administration of appropriate antibiotics in septic patients are strategies which reduce mortality.5,6 Finally, early reperfusion therapies may improve outcome in patients with acute myocardial infarction or ischemic cerebrovascular events.4 Thus outcomes for critically-ill patients are influenced by whether or not optimal intensive care is delivered in a timely manner, which in turn is determined by how long the patient waits in the emergency department for admission to the ICU.
As has been shown, ED length of stay is associated with patient outcome. However, other than ED crowding and non-availability of ICU beds, factors associated with prolonged time in the emergency department are not well known. We selected a subgroup of prolonged ED stays using a 5-h cut-off. This threshold was determined according to the median ED length of stay among our population of approximately 5h. Prolonged emergency department length of stay (>5h) was associated with the age and the type of illness. Fifty percent of the ICU transfers whose ED stay was longer than 5h were septic patients; moreover, the median ED length of stay for these septic patients was 8h. These results are consistent with previous studies which focused on delayed ICU transfers.8,9 It is noteworthy that septic patients were among those that experienced longer stays in the emergency department, despite previous studies having suggested that septic patients benefit from early recognition, timely administration of antibiotics, and resuscitation with intravenous fluids and vasoactive drugs, all of which are care interventions frequently directed by critical care specialists.24–26 This suggests that, in our institution, sepsis may not yet be perceived as a highly time-sensitive process. Respect to the age, it is difficult to explain its relationship with a prolonged emergency department length of stay. However, we think that this factor could also be related with the type of illness, because sepsis was the most frequent diagnosis in older patients (above 65 years), and septic patients are probably associated with a delay in the ICU admission. Nevertheless, additional studies would be needed to support this statement. Finally, although resources and staffing levels are usually reduced at weekends and during the night,27,28 neither the day of the week nor the shift had any correlation with prolongation of ED stay and ICU admission among our study population. This might be explained by having onsite qualified intensivists coverage to ensure continuity of care.
The limitations of our study must be considered. Firstly, data from a single center was analyzed. External validity is low, therefore, and further multicentre studies are needed to corroborate our results and identify risk factors for prolonged ED stays. Secondly, the presence of others confounding factors, such as ICU occupancy rate or ED occupancy rate at the moment of ICU admission, were not taken into account. Future work will need to assess whether these and other related factors are associated with ED length of stay. Finally, there is a degree of diagnostic heterogeneity and this is a factor that could have influenced the observed results. Trauma, obstetrics and coronary artery disease patients were not included, however, due to the existence of specialist ICUs for these pathologies in our institution.
In conclusion, a prolonged emergency department stay prior to ICU admission is related to worse outcomes, including the development of time-dependent complications and increased mortality. Our findings suggest a possible benefit from earlier ICU transfers and the initiation of organ support without delay. The diagnostic category was the principal factor associated with the prolongation of emergency department length of stay. Emergency department physicians can have a significant impact through early recognition of illness severity and facilitation of access to intensive care for the initiation of proper therapeutic interventions.
Authors’ contributionsRenata García Gigorro has been in charge of the review of the literature, data collection and article writing.
Felipe de la Cruz-Vigo has contributed to the study design and final review critical article.
Eva Maria Andrés-Esteban has conducted the study design and analysis and interpretation of data.
Silvia Chacón-Alves has participated in the data collection.
Guillermo Morales-Varas has participated in the data collection.
Jose Ángel Sánchez Izquiedo has contributed to critical revision of the article.
Juan Carlos Montejo has been responsible for the provision of the necessary resources to conduct this study. He has also participated in the final review critical article.
Ethical disclosureProtection of people and animalsThe authors state that the procedures conformed to the ethical standards of human experimentation committee responsible and according to the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed the protocols of the workplace on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the consent of Clinical Research Ethics Committee (CEIC) of the hospital. The committee desertion the need for informed consent due to non-interventionist nature of the study. This document is held by the corresponding author.
Conflicts of interestThe authors declare no conflicts of interests.