The management of critical trauma disease (CTD) has always trends the trends in military war experiences. These conflicts have historically revolutionized clinical concepts, clinical practice guidelines and medical devices, and have marked future lines of research and aspects of training and learning in severe trauma care. Moreover, in the civil setting, the development of intensive care, technological advances and the testing of our healthcare systems in the management of multiple victims, have also led to a need for innovation in our trauma care systems.
La atención a la patología traumática crítica (PTC) siempre ha recogido las ten-dencias del manejo de los traumas generados por conflictos bélicos. Estos conflictos han revolucionado históricamente los conceptos clínicos, las guías de práctica clínica, los equi-pos, han marcado las líneas de investigación venideras e incluso han servido para definir nuevosaspectos curriculares y de formación para la atención al trauma grave. Por otra parte en elámbito civil la evolución de los cuidados intensivos, el avance tecnológico, así como la puestaa prueba de nuestros sistemas sanitarios a la atención de múltiples víctimas, también hanprovocado la necesidad de innovación en nuestros sistemas de atención al trauma.
The management of critical trauma disease (CTD) has always contemplated the trends in military war experiences.1 These conflicts historically have revolutionized clinical concepts, clinical practice guidelines and medical devices (in terms of both invention and applications), and have marked future lines of research and aspects of training and learning in severe trauma care.2 Clearly, extrapolating these experiences is not without problems and bias (the ultimate objectives of military medicine, the characteristics of research, the hostile environment in which it takes place, the types of trauma, the underlying mechanisms involved, etc.). However, even in this setting there have been advances through the establishment of registries, international collaboration, and relations between the civil and military contexts. After over a decade of military conflicts in different settings, a review is required of the most innovating aspects of the management of CTD.3
On the other hand, in the civil setting, the development of intensive care, technological advances (largely referred to imaging techniques) and the testing of our healthcare systems in the management of multiple victims, have also led to a need for innovation in our trauma care systems. Furthermore, from the start, the management of CTD has been tied to the field of Intensive Care Medicine, and has always had an enormous influence upon its progression (management of bleeding, nutrition, training, etc.).4
For all the above reasons, these developments in CTD require a review of those aspects referred to innovation–the latter being understood according to Rye as: “any material, artifact or practice representing an important deviation from the currently assumed body of knowledge, as determined by the collective judgment of people with expertise in the field in the moment in which it appears for the first time in the context of practice”.5
The present study offers a review of the main research lines, novel aspects related to patient resuscitation, new devices, modifications in the care of cardiorespiratory arrest (CRA) in trauma, and the training and structure of trauma care teams–attempting to establish a difficult inference regarding the future of these topics in such a changing type of disease. The interpretation of these innovating subjects always must be made within context (stock of knowledge on the subject, the institutional and social environment, and the efforts of our organization).6
Research lines in critical trauma diseaseResearch in trauma disease, particularly referred to initial patient care, has a series of special characteristics and challenges that are different from those found in research in other areas, including Intensive Care Medicine referred to other types of diseases. The intense and necessary collaboration with the pre-hospital setting, the difficult differentiation between research and innovation in this field, the need for informed consent or substitutes thereof (consent from an independent physician), the scant time available for patient inclusion, and the influence of trauma care system maturity upon the outcomes, all complicate the conduction of clinical trials in this type of disease. Despite such difficulties, however, in recent years we have witnessed advances in methodological aspects and in the conduction of pragmatic trials, with high external validity, which have produced a genuine revolution in this field–resulting in levels of evidence which previously had only been possible in other types of diseases.7–9
The main lines of research in CTD focus on the new strategies referred to resuscitation with damage control. This concept is defined in the glossary of terms of the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias, SEMICYUC), and encompasses the use of permissive hypotension in patients, adequate settings and types of trauma, the restrictive use of crystalloids, measures against hypothermia and acidosis, the use of prohemostatic drugs adjusted to the published evidence, and hemostatic resuscitation practices involving the balanced use of blood products in patients with traumatic hemorrhagic shock.10
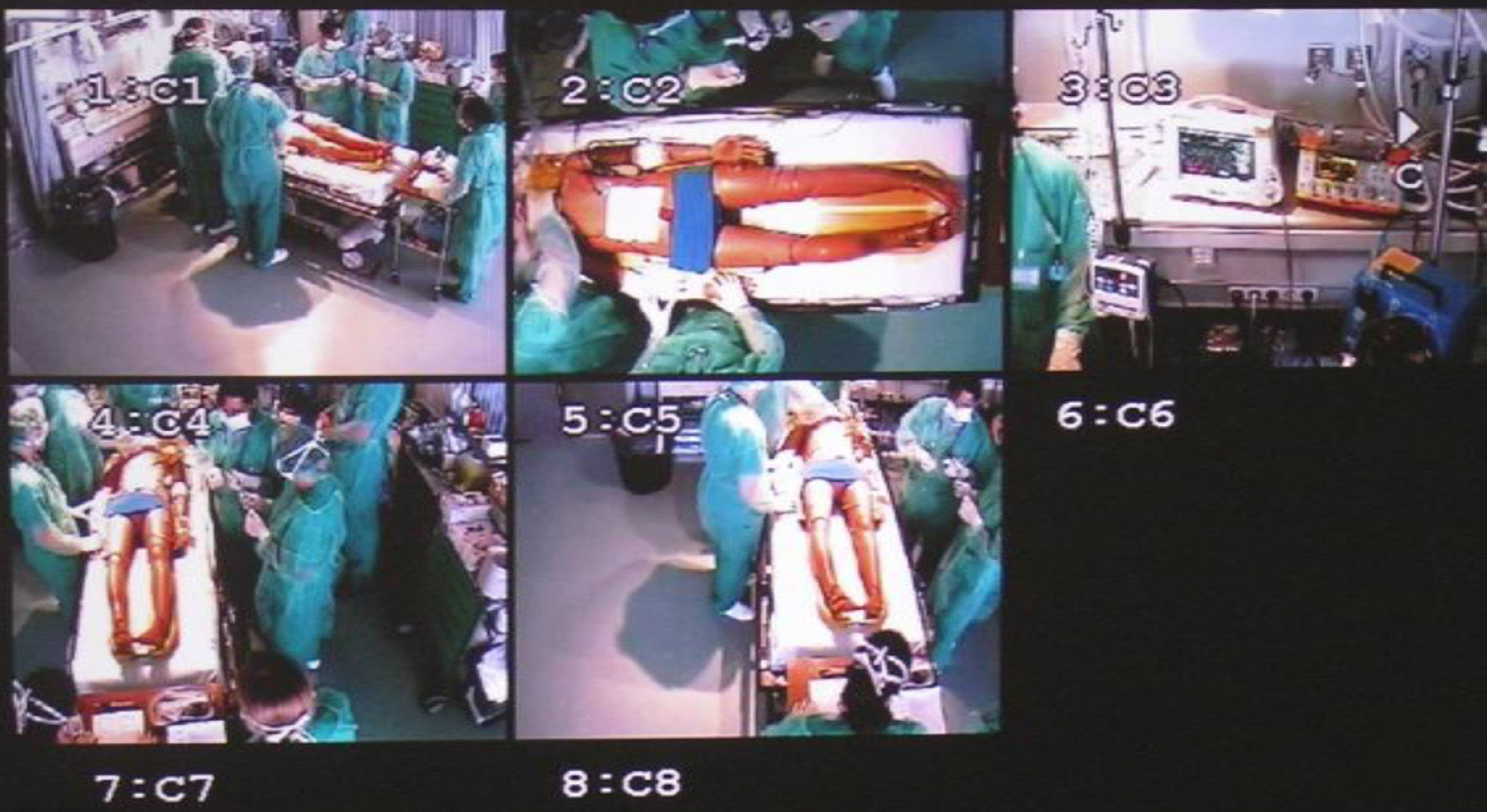
The main research lines that have given rise to clinical trials are summarized in the following tables. The data have been obtained through a search in: clinical trials.gov (US National Institutes of Health), Current Controlled Trials, COCHRANE central register of controlled trials, using the following terms: trauma patients, severe trauma/coagulopathy, trauma/fibrinogen, trauma/tranexamic acid, trauma/antifibrinolytics, trauma/activated recombinant human factor VII, trauma/rFVIIa, trauma/hypotensive resuscitation, trauma/transfusion, trauma/thromboelastography, trauma/hemostatic resuscitation.
These studies fundamentally deal with the pharmacology of hemostasis, permissive deferred hypotension and the type of fluids used in trauma care, hemostatic resuscitation, point of care guided resuscitation versus predetermined resuscitation, with the use mainly of viscoelastic techniques (thromboelastogram or rotational thromboelastometry) or evolutions of these techniques, and attempting to consider all the systemic factors implicated in coagulation (platelets, endothelium, whole blood, etc.). Almost all of the publications are related to the change in paradigm in resuscitation (Table 1).
Studies (PubMed-clinicaltrials) related to the pharmacology of hemostasis, permissive hypotension, fluid therapy used in trauma, hemostatic resuscitation, and the point of care management of coagulopathy due to trauma.
| Pharmacology of hemostasis |
| RETIC Trial: Reversal of trauma induced coagulopathy using coagulation factor concentrates or fresh frozen plasma |
| An observational study of early coagulopathy, or clotting disorder, in injured patients |
| Clinical randomization of an antifibrinolytic in significant hemorrhage |
| Fibrinogen concentrate (FGTW) in trauma patients, presumed to bleed |
| Study of fibrinogen metabolism during severe trauma and burns |
| Effect of an early prehospital administration of tranexamic acid on hyperfibrinolysis in multiple trauma |
| Platelet function analysis in head trauma: ASA/Plavix |
| Efficacy and safety of activated recombinant human factor vii in severely injured trauma patients |
| The use of rFVIIa in trauma patients: a multi-center case registry |
| National Registry of rFVIIa (Novoseven) in Hemorrhagic Traumatology |
| Permissive hypotension |
| A comparison of two target mean arterial pressures in the resuscitation of hypotensive trauma patients |
| Field trial of hypotensive versus standard resuscitation for hemorrhagic shock after trauma |
| Colloids in severe trauma |
| Optimal fluid resuscitation for trauma patients |
| Normal saline versus plasmalyte in initial resuscitation of trauma patients |
| Hypertonic resuscitation following traumatic injury |
| AVERT shock: arginine vasopressin during the early resuscitation of traumatic shock |
| Efficacy and safety of colloids versus crystalloids for fluid resuscitation in critically ill patients |
| Fluid therapy in trauma |
| Pragmatic, randomized optimal platelets and plasma ratios |
| The trauma formula driven versus lab guided study (TRFL Study) |
| The effect of red blood cells transfusion in trauma patients |
| Frozen red blood cell transfusions in trauma patients |
| Effectiveness of plasma transfusions in critical care patients |
| Point of care in coagulopathy. Current experimental sturis (PubMed-clinicaltrials) |
| A prospective evaluation of thromboelastography for identifying coagulopathy in severely injured patients |
| Comparison of rapid thromboelastography and conventional coagulation testing for haemostatic resuscitation in trauma |
| Evaluating the use of thromboelastography to diagnose coagulopathy after traumatic brain injury |
| The clinical utility of thromboelastography in guiding prophylaxis of venous thromboembolism following trauma |
| Rapid TEG MA validation |
In recent years there has been an increase in the development of new devices applied to initial patient care and to the posterior management of trauma. In this regard, the advances have fundamentally consisted of improvements of different already existing techniques, with a view to expanding their use.
TourniquetsTourniquets are devices that had been regarded as a last resort in limb injuries causing hemorrhagic shock, or had even been discarded at the start of recent military conflicts and had to be reintroduced as specific protocols (combat application tourniquet) because of the large number of casualties due to exsanguination in vascular trauma. Different designs have attempted to minimize the side effects of tourniquet use, though rather than using one device or other, the important factor is probably recognition that the control of limb exsanguination is one of the most important aspects of pre-hospital care, both for saving the life of the patient and for limiting unnecessary resuscitation measures.11
New tourniquet versions, such as pneumatic devices, may prove to be essential for the management of injuries in the pre-hospital setting or until definitive bleeding control is achieved. However, the insufflation pressure of these devices has not been established, and there have been a certain number of cases of temporary or even permanent tissue damage associated to their use. As a result, in recent years systems have been described that make use of insufflation pressure synchronized to patient arterial pressure. These systems require a monitor with information on the vital signs, since they immediately adjust the insufflation pressure according to the existing systolic blood pressure, measured at concrete intervals.12 Good safety and efficacy have been reported during their use in limb surgeries without complications, fundamentally those of a neurological nature.13
Although these devices are probably less widely used in the civil setting due to the lesser incidence of vascular injuries and the shorter times to definitive bleeding control, their use probably will be maintained in the future. Fig. 1 shows the reusable tourniquet design employed in our setting.
Hemostatic dressings and forcepsThose injuries not amenable to tourniquet use are difficult to control and are a cause of mortality in the military setting. In this regard, recent estimates indicate that 4.6% of the victims of military conflicts could have been saved with the use of a device capable of controlling the bleeding.14
A temporary wound closing device, the iTClamp®, has been developed to control severe bleeding of open wounds in compressible body zones (Fig. 2). The device seals the margins of the skin within a pressure barrier, allowing the formation of a hematoma in which the blood accumulates under pressure to form a stable clot until definitive surgical repair is performed. The clamp is applied by aligning it with the edges of the wound and then pressing the arms together to seal the device. A locking mechanism prevents it from opening accidentally. There are needles near the edges of the skin to allow complete sealing and reduce slippage.15 Most publications attempting to demonstrate its efficacy in application to vascular damage are based on studies in animals or cadavers.16 Nevertheless, despite the few clinical studies available, the results obtained show greater survival rates than with the standard devices, as well as less blood loss, without causing the occlusion of distal flow or skin tearing or lesions.
As regards hemostatic dressings, it must be pointed out that until only a few years ago, gauzes were the only kind of dressing available. In recent years, dressings in trauma have improved with the addition of different hemostatic agents–the most common being chitosan and the kaolin, although there are also other so-called second generation agents. None of the different options have been shown to be superior to the rest, though they are more effective than common dressings in controlling bleeding.17
Sternal intraosseous systemsNew sternal intraosseous devices have been developed for the administration of fluids (Fig. 3), allowing rapid vascular access with a high infusion capacity. These devices are compatible with the use of a neck collar, and have been especially designed for the pre-hospital setting. They are equipped with stabilization points and an infusion tube allowing rapid insertion (in under 60s) even by non-expert personnel, with a high success rate.18
The system must be placed perpendicular to the manubrium in order to allow adequate administration, since otherwise the device is unable to correctly penetrate the bone. It should not be used in patients with important osteoporosis, in children under 12 years of age, or in individuals with severe thoracic trauma.
Resuscitative endovascular balloon occlusion of the aorta (REBOA)Although this device is not new (it has been known since the Korean war), it has been revisited in more recent publications as a result of endovascular technological improvements, and has been revised for use in initial trauma care.19 The utilization of resuscitative endovascular balloon occlusion of the aorta (REBOA) requires knowledge of the key steps, which can be summarized as follows: vascular access, selection and positioning of the balloon, insufflation and deflation of the balloon, and finally removal of the sheath.20 The access can be established via the percutaneous route with or without ultrasound guidance, though prior decision must be made of where occlusion is to be performed, depending on the suspected origin of the bleeding (zone I: descending thoracic aorta between the root of the left subclavian artery and the celiac artery; zone II: between the celiac artery and the renal artery; and zone III: from the infrarenal aorta to the iliac bifurcation). In cases of refractory shock, placement should be in zone I, though in patients with pelvic bleeding the selected location is zone III. This procedure is equivalent to manual aortic control in damage control surgery in hemorrhagic shock patients, though in this case adopting an endovascular approach.21
The balloons and sheathes come in different sizes depending on the occlusion zone involved (large and long in zone I, and short and of large diameter in zone III). Insufflation is carried out through the administration of contrast with saline solution, and visualization is performed under radiological control–evidencing compression during systole. In contrast, deflation of the balloon must be done slowly in order to avoid a sudden drop in afterload and the induction of arterial hypotension.
Few patient series have been published. Brenner et al. described the cases attended in a trauma center, with goods results in the form of low mortality and few complications–though the authors recognized that definition is needed of those patients who stand to benefit most from the technique.21
Other devicesOther devices where the existing experience is more limited are the abdominal aortic tourniquet (combat ready clamp), other “joining” tourniquets for the groin, axillas and neck, designed to control bleeding outside the region of the extremities,22,23 and the so-called hypothermia prevention and management kit.24
Surgical management of thoracic traumaConcern about modifying the clinical course of chest injuries through surgery is not new. However, there have been new devices and developments regarding the selection of patients who might benefit from such surgery.25 The surgical management of thoracic trauma allows stabilization in cases of multiple rib fractures with important chest deformation. Different implant systems have been developed for this purpose: 3D costal clips with between 6 and 9 segments for stabilizing fractures at several locations, or implant bridges composed of two or more clips aligned with a connecting bar. These devices are currently made of titanium, which allows better adaptation, lesser loss of resistance, and the recovery of shape without loss of pressure.26
There is little scientific evidence on these devices, the existing data being centered on series with few patients, though the results are favorable in terms of days on mechanical ventilation and stay in the Intensive Care Unit (ICU), with less pain and better rehabilitation outcomes. These results are more patent when management is performed early and with adequate patient selection.27,28
Other innovations in the field of trauma surgery are the reorganization of the specialty toward emergency care surgery, the use of temporary vascular shunts, vacuum systems in open fractures, preperitoneal packing in pelvic injuries, and the endovascular management of vascular damage at different levels.
Cardiac arrest in traumaCardiac arrest in trauma has been associated to high mortality, with an overall survival rate of only 5.6%. In this regard, cardiac arrest in the context of trauma was classically regarded as normally resulting in death upon admission. For reasons that have not been well clarified, the survival figures in the last 5 years have improved with respect to the previously reported data. Nevertheless, the neurological outcome among the survivors is favorable in only 1.6% of the cases.29
In terms of the mechanism underlying trauma, both closed and penetrating injuries present similar survival rates, though the neurological outcomes are more favorable in penetrating trauma. However, this may be due to confounding factors related to when death is certified.30
Since the year 2005 a number of articles have reported improvements in the survival rates, though the precise reasons for such improvement are not clear. Survival after cardiac arrest in trauma has even been reported to be comparable to that observed in other types of cardiac arrest involving guided protocols.31 Initial liberal application of cardiopulmonary resuscitation (CPR) measures is recommended, provided the number of patients is manageable, and restrictive CPR protocols in cardiac arrest in trauma are not advised.32
Survival after cardiac arrest in trauma is correlated to the time of CPR and of pre-hospital arrest. In this regard, the literature considers CPR to be successful when recovery is achieved in under 16min.33
Pre-hospital intervention should contemplate the on-scene exclusion of reversible causes. In this respect, vital maneuvering is required at the site of the accident, with quick transfer of survivors to the nearest appropriate medical center. Retrospective studies have attempted to identify the factors associated to increased recovery of spontaneous circulation and to improved neurological status in cardiac arrest in trauma. The group led by Camacho Leis et al.34 analyzed a total of 167 patients with cardiac arrest in trauma in the pre-hospital setting, and recorded a survival rate of 49.1%, with full neurological recovery in 6.6% of the cases. Greater benefits were noted in children, as well as in patients with initial ventricular fibrillation or electrical activity in the absence of a pulse. Key aspects are taken to be a rapid response, with aggressive resuscitation using fluids, and placing priority on early management of the reversible causes (especially thoracotomy in the case of cardiac tamponade).35
Importance of thoracotomy in traumatic cardiorespiratory arrestThere is much controversy regarding the use of thoracotomy at both pre-hospital and hospital level. The technique has been regarded as being of little use when the resuscitation times are prolonged, conditioned to the type of mechanism involved: 5min in closed trauma and 15min in penetrating trauma. In this regard, recently established protocols recommend emergency thoracotomy in patients with closed thoracic trauma if surgery cannot be carried out in less than 10min–with favorable outcomes not only in terms of survival but also as regards neurological recovery. A number of aspects must be taken into account when interpreting the most recently published information: biochemical tests (with resuscitation parameters obtained from intracardiac blood sampling); the differences in results obtained between studies published in Europe and the United States, and which are probably attributable to the setting and training of the specialist performing the technique; the analysis of long-term functional outcomes among the survivors; the costs according to quality adjusted life years (QALYs)(which would make the procedure profitable in penetrating but not in closed trauma); and exposure to biological risks of the attending team and the possible use of some of these patients as organ donors.36
Controlled deep hypothermia and extracorporeal membrane oxygenation (ECMO) in CRA in trauma. Suspended animation for delayed resuscitationIn situations of CRA, cell death occurs within minutes if tissue perfusion is not restored. The greatest challenge in patients with cardiac arrest secondary to exsanguinating trauma is to achieve adequate hemostasis and restore the lost volume before ischemic damage is caused in particularly sensitive areas such as the brain. We therefore may consider the start of cell protecting maneuvers while gaining time to control bleeding and repair the damage (the suspended animation for delayed resuscitation concept). One such maneuver would be the induction of cardiac arrest with controlled deep hypothermia. The use of this type of resuscitation strategy would represent a genuine change in approach–coming into contradiction with the idea that hypothermia is an indicator of poor prognosis and that hypoperfusion is a key factor in coagulopathy associated to trauma. Nevertheless, there are nonclinical studies that demonstrate the protective role of controlled deep hypothermia and the possibility of applying extracorporeal support to combat ischemia-reperfusion lesions, with improved survival rates. Although this type of strategy has been found to be technically feasible in animal models, it has not been supported by clinical studies.37,38 Recently, a multicenter trial has been authorized in the United States to study the usefulness of this strategy in combination with emergency thoracotomy in trauma and the provision of extracorporeal support using cardiopulmonary bypass techniques. The mentioned trial will investigate the usefulness of preservation and resuscitation in cardiac arrest in trauma, recruiting penetrating trauma patients presenting arrest after 5min or in the medical center. Cannulation for extracorporeal membrane oxygenation (ECMO) will be carried out, with rapid transfer to the operating room for damage control surgery, and adequate resuscitation–the primary endpoint being survival at hospital discharge and the assessment of neurological impairment.39
Trauma care organization and teamsSince its beginnings, Intensive Care Medicine has witnessed great progress in terms of technology and our knowledge of disease and its physiopathology, with perhaps somewhat lesser progression in relation to more strictly therapeutic aspects. However, the factor that has contributed most to improve patient prognosis has been improvement in the care processes (improved teamwork, training and communication, fewer iatrogenic effects, and contact with the patients and their families).4 Teamwork is particularly important in the management of critical trauma patients. The availability of cohesive trauma teams with an optimum distribution of roles and with strong leadership capable of securing rapid patient resuscitation and stabilization, shortening the diagnostic and treatment times with the purpose of increasing the chances for survival, are crucial considerations that offer benefits versus trauma management by different services that may be implicated in trauma management–particularly in seriously ill patients with an injury severity score of >12 and with severe brain injuries.40
Specifically, teams characterized by a horizontal approach (with the presence of a leader, and role distribution between a multidisciplinary team with fixed personnel and inter-consultants) have been found to shorten the time from trauma to critical intervention (e.g., neurosurgery or bleeding control surgery).41,42
Research in the context of teamwork in the ICU, and specifically in trauma care, is a topic of growing interest in the scientific literature. Improvements in this area focus both on transition activities (referred to the transfer of information) and on actions (specific work activities). The fundamental actions for team improvement are team training and the existence of adequate communication protocols.43,44
SimulationOne of the most important aspects in relation to learning and the monitoring of team performance is the use of simulations. The latter contribute to generate expert competences through the application of practices, techniques and feedback to replicate the environment in which real clinical scenarios take place. The use of simulations in traumatology has been shown to improve a number of dimensions in trauma care such as leadership, monitoring of the situation, mutual support within the team setting, communication and overall performance, using instruments such as the Trauma team performance observation tool.45 Another useful simulation tool is the Theater team non-technical skill scoring system (T-NOTECHS), used to assess non-technical skills in multidiscipline trauma care teams. The use of this instrument has been shown to improve resuscitation times, compliance with the T-NOTECHS scale, and the frequency of almost perfect task performance.46 Although the impact is clear in the literature (pre-post studies with simulation as intervention) regarding the improvement of performance, the long-term effects of simulation strategies are subject to controversy (maintenance of these strategies probably being needed).47 There is also controversy as to which method is best (mannequin or patient), particularly when the aim is to improve training in communication, cooperation and team leadership.48 In the coming years such strategies undoubtedly will have a great impact on both the acquisition and maintenance of skills related to trauma management.
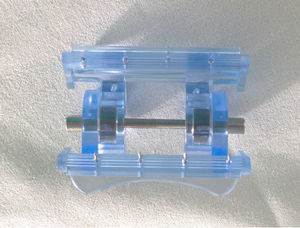
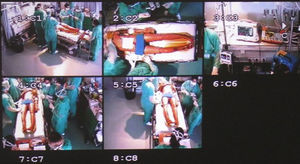
Video recordingA number of studies have evaluated the use of video recordings for both simulation purposes and in application to real clinical cases. In our center such recordings have been used for quite some time to assess severe trauma admissions. In this respect, Figs. 4 and 5 show the initial trauma management box of our ICU with video cameras in the ceiling, along with camera views corresponding to a simulation of initial care in our Unit. Evaluation by means of this method has been integrated within a routine quality assessment practice.
Video recording has three basic objectives: evaluation of real cases that may be of educational value; reviewing of real cases with the aim of modifying behaviors and of analyzing general management in a more realistic and structured manner, with feedback from the most experienced professionals; and use of the acquired data for research purposes.49
From the first study published by Hoyt et al. and in posterior articles on the application of this technique, reductions have been reported in initial management time, very particularly in the more seriously ill patients.50,51
Reviewing of the video recordings must be made by a range of professionals implicated in severe trauma cases (radiologists, pre-hospital emergency teams, surgeons, vascular radiologists, etc.), and an objective review protocol should be used. In this regard, we must assess not only objective issues such as adherence to protocols (massive bleeding, airway, prophylaxis, etc.) but also aspects such as leadership or teamwork. In this sense, the T-NOTECHS evaluates 5 non-technical behavioral skills and can be used to assess such aspects from the video recordings.52
Of particular usefulness is the fact that video recording is very objective in evaluating both times and individual performance. Seeing oneself at work is probably the most useful way to evolve toward behavioral and cultural changes by detecting differences between what we think we are doing and what we really are doing.53
The future of trauma teamsIn addition to the topics dealt with above, three other aspects are described as crucial in the coming years for incorporating the new care paradigms to trauma teams. The first aspect refers to the integration of full-body computed tomography (CT) assessment in unstable patients. It is clear that the technological developments of the last decade, the limitations of the patient case history and of exploration in CTD, the proximity of the necessary equipment to the emergency care area, and the possibility of rapid exploration with more detailed information on all the anatomical regions have long ago caused CT to become a key instrument in the evaluation of our patients.54 Although there is some encouraging experience referred to the improvement of patient survival using full-body CT evaluation of trauma patients with hemodynamic instability,55,56 application of the technique in any type of institution requires the necessary logistics to ensure rapid exploration in a fully structured setting specifically referred to trauma disease (not to any acute emergency condition requiring imaging studies), and with a well organized trauma team. Furthermore, there must be well established criteria regarding the type of patients amenable to exploration, with a view to limiting exposure to ionizing radiation and contrast media. In turn, the radiologist must be fully integrated within the trauma team, with real-time definition of the priorities, the implementation of quality assessment instruments (e.g., modal failure and effects analysis), and due peer recognition. In general, and in the opinion of many authors (including ourselves), trauma care will continue to be guided by physiological parameters–though as has been seen in recent years, this imaging technique will be used on an increasingly earlier basis in the resuscitation phase.57
The second aspect to be incorporated in future to trauma teams is more proactive management of hemorrhagic shock, adopting massive bleeding protocols as horizontal procedures in the centers, capable of remedying the many gaps in knowledge that characterize the management of such cases (evidence-based prohemostatic drug use, drug combinations, administration time, early blood product availability, real-time blood product ratio calculations, point of care thromboelastographic or platelet aggregometry coagulation monitoring, with auditing through the transfusion commissions and as a procedure more encompassed within hospital patient blood management, etc.).
Lastly, the possibility of incorporating new spaces for initial trauma care should be considered. An example of this is an immediate CT scan upon admission, as secondary exploration, in the emergency care room. Patients requiring immediate surgery or CPR would be excluded from such practice, according to the criterion of the initial management supervisor. This methodology is currently being examined in the context of a controlled trial.58
In the coming years we will also have to evaluate integral surgical and interventional management initiatives within the same physical space. This concept has given rise to the term RAPTORS (Resuscitation with Angiography, Percutaneous Techniques and Operative Repair), allowing us in one same resuscitation room to apply intensive care, interventional radiology and possible open surgery, with multidiscipline patient management.59 No studies have yet been made to demonstrate the efficacy of such rooms. Nevertheless, over time, clinical management tends to focus upon damage control, accelerating the control of bleeding with designs of this kind–though leadership problems may arise as a result of the mixing of actions of different professional teams.
Discussion and conclusionsThe current world social and political situation unfortunately suggests an important increase in innovations referred to the management of trauma patients in our ICUs. Historically, the only winning party in any war has been the field of critical trauma care.60 Although interesting, in order for the strategies of the military setting to be correctly applied in the civil context, we need reflection, perspective, validation based on controlled studies, and adaptive effort. The greatest source of innovations in this type of disease will come from improved methodology in emergency care medicine, resolution of the gaps in knowledge referred to resuscitation strategies, the study of the influence of changes in the epidemiology of trauma disease upon patient patterns and outcomes, the incorporation of new devices, spaces and concepts, and also the application of methodologies for ensuring correct trauma care team performance. One of the most novel and important aspects in this regard is the study of factors that condition team work, communication issues, and role distribution.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Chico-Fernández M, Terceros-Almanza LL, Mudarra-Reche CC. Innovación y nuevas tendencias en patología traumática crítica. Med Intensiva. 2015;39:179–188.