Pressure support ventilation (PSV) is used during gradual weaning from mechanical ventilation (MV) or to favor spontaneous ventilation, and its potential benefits (improved oxygenation and the avoidance of diaphragmatic atrophy) must be weighed against its potential harmful effects such as overdistension in dependent pulmonary zones and diaphragmatic damage due to overload in the presence of excessive respiratory effort or severe lung injury. Distending pressure (DP) (as a signal of protective or harmful ventilation) is often used during assisted/controlled MV, though its evaluation in spontaneous modes has received little attention in the literature. Furthermore, in PSV it is difficult to clearly see the contribution of the effort generated by the respiratory muscles, unless an esophageal balloon is available.
The present study describes the use of inspiratory and expiratory protocols during PSV as an estimation of DP and inspiratory effort, discussing its limitations and potential clinical implications.
Inspiratory pause: respiratory effort and static distending pressureThe feasibility of an inspiratory pause during MV in spontaneous modes was demonstrated in the 1990s. Pesenti et al.1 Described the “airway occlusion maneuver” and showed estimated resistance and elastance in PSV to be well correlated to the measurements made in controlled MV or using an esophageal balloon.
Fundamentally, the inspiratory pause in PSV allows us to estimate two main variables: the respiratory effort of the patient and distending pressure. However, its adequate interpretation requires us to take a number of limitations into account.
During PSV, the inspiratory pause reflects patient effort, with a positive pressure greater than the programmed maximum pressure (pressure support [PS] + positive end-expiratory pressure [PEEP]), due to relaxation of the respiratory muscles (Fig. 1). This effort can be quantified by the pressure muscle index (PMI),2 which corresponds to the difference between the plateau pressure (Pplat) and the programmed maximum pressure. The PMI is correlated to the inspiratory muscle pressure (Pmus) and to the pressure x time product – both being indicators of respiratory effort.
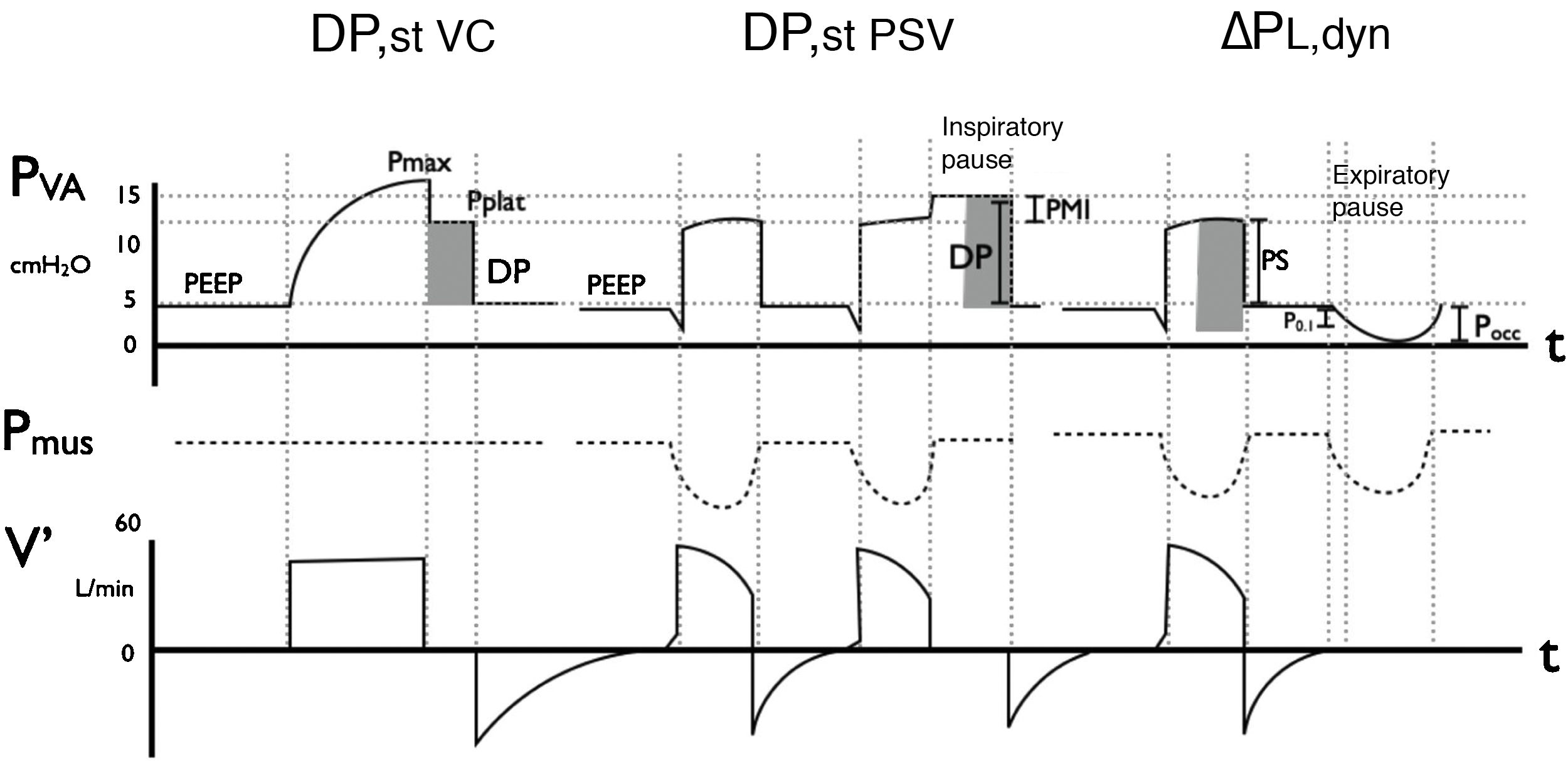
Methods for measuring distending pressure (DP) in volume control mode (DPst VC) and in pressure support mode: static (DPst PSV) and dynamic (△PL,dyn).
Representation of the curve corresponding to airway pressure (Pva), muscle pressure (Pmus) and flow over time. In VC mode with constant flow, an inspiratory pause evidences the plateau pressure (Pplat), which represents the elastic rebound pressure of the respiratory system. As there is no inspiratory effort (Pmus = 0), the difference between Pplat and PEEP is the DP. Transpulmonary pressure in PSV depends on both pressure support (PS) and on the component of Pmus; an inspiratory pause allows us to evidence this effort, by raising the pressure curve to a value greater than the configured value: this is the Pplat, and its difference with PEEP is DP., In dynamic mode, △PL,dyn is estimated by summing PS to −2/3 occlusion pressure (6) (Pocc). Both methods are inter-correlated, with △PL,dyn always being (since it includes the resistive component of the respiratory system). On the other hand, PMI is also represented, being Pplat – (PS + PEEP), and constituting an indicator of inspiratory effort, together with P0.1, which is the pressure measured in the first 100 ms of inspiration and reflects the intensity of respiratory center demand.
Note: Pocc is always ≤0 cmH2O (negative with respect to basal).
The DP corresponds to the difference between Pplat and total PEEP, and its estimation is possible in the presence of a reliable inspiratory pause.3 A high DP has been associated to increased mortality (OR 1.34; 1.12–1.61) in patients with acute respiratory distress syndrome (ARDS) in PSV.4
With regard to the limitations of Pplat during PSV, the most common corresponds to the presence of expiratory effort (the muscles do not relax passively), which can increase Pplat. However, this situation can only overestimate DP; consequently, a low DP under these conditions implies the absence of global pulmonary overdistension.5 Three possible patterns following an inspiratory pause have been described: analogous to passive (Pplat < Pmax), defined plateau (Pplat stable ≥ Pmax) and irregular elevation (Pplat > Pmax without established plateau).5 Only the first two allow us to measure Pplat, since Pplat without an established plateau can under- or overestimate DP. Other technical aspects for adequate measurement are described in Table 1.
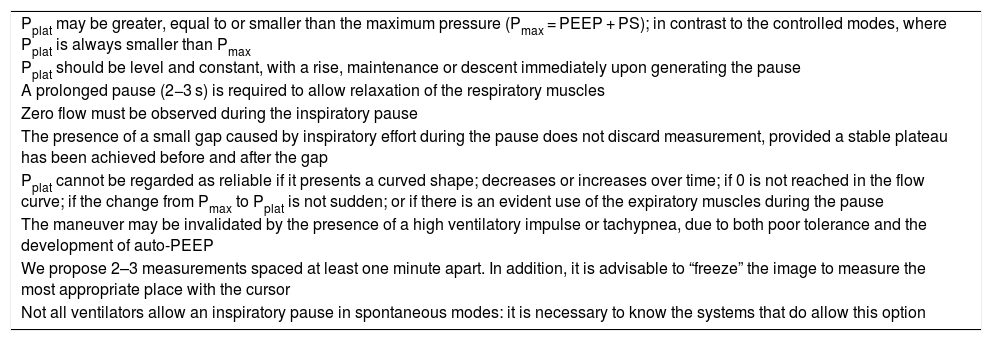
Considerations for adequate execution of an inspiratory pause and interpretation of distending pressure in pressure support ventilation.
| Pplat may be greater, equal to or smaller than the maximum pressure (Pmax = PEEP + PS); in contrast to the controlled modes, where Pplat is always smaller than Pmax |
| Pplat should be level and constant, with a rise, maintenance or descent immediately upon generating the pause |
| A prolonged pause (2−3 s) is required to allow relaxation of the respiratory muscles |
| Zero flow must be observed during the inspiratory pause |
| The presence of a small gap caused by inspiratory effort during the pause does not discard measurement, provided a stable plateau has been achieved before and after the gap |
| Pplat cannot be regarded as reliable if it presents a curved shape; decreases or increases over time; if 0 is not reached in the flow curve; if the change from Pmax to Pplat is not sudden; or if there is an evident use of the expiratory muscles during the pause |
| The maneuver may be invalidated by the presence of a high ventilatory impulse or tachypnea, due to both poor tolerance and the development of auto-PEEP |
| We propose 2–3 measurements spaced at least one minute apart. In addition, it is advisable to “freeze” the image to measure the most appropriate place with the cursor |
| Not all ventilators allow an inspiratory pause in spontaneous modes: it is necessary to know the systems that do allow this option |
PEEP: positive end-expiratory pressure; Pmax: maximum airway pressure; Pplat: plateau pressure; PS: pressure support.
An expiratory pause can also be used to detect an excessive inspiratory effort and to predict △PL,dyn. This maneuver measures the pressure change during occlusion of the airway (△Pocc) on initiating spontaneous inspiration (Fig. 1). In contrast to static DP, this method allows us to estimate △PL,dyn without performing an inspiratory pause and without its potential limitations. The prediction of △PL,dyn and Pmus through △Pocc requires the application of a conversion factor, and is estimated based on the following equations6: [△PL,dyn = (peak pressure − PEEP) − 2/3 × △Pocc]; [Pmus = −3/4 × △Pocc]. Both correction factors (2/3 and −3/4) correspond to the ratio between the means of △Pes and Pmus during respirations without occlusion with respect to the mean of △Pocc, respectively. Although the intra- and inter-individual concordance limits of Pmus and △PL,dyn showed a wide range, the capacity to detect excessive respiratory effort and an elevated △PL,dyn proved excellent (area under the receiver operating characteristic curve [AUROC] > 0.9) in all cases. From a practical point of view, values of Pmus ≤ 10 cmH2O and △PL,dyn ≤ 15 cm H2O are considered safe during PSV,6 while the recording of △Pocc = 0 cmH2O corresponds to the absence of effort, with △PL,dyn being equivalent to passive ventilation. The end-expiratory volume is a relevant factor for the capacity of the diaphragm to generate pressure; accordingly, △Pocc could be underestimated in the presence of air trapping.
A retrospective analysis compared both DP measurement methods (static and dynamic) during PSV.7 The correlation proved significantly positive (R2 0.77), reaching R2 0.81 on adding the resistive component to PDest7; the concordance test showed a mean difference of 1.3 cmH2O with a 95% confidence interval (95%CI) of −2.6 to 5.2. These results indicate that both methods are coherent and offer complementary information during PSV. However, the dynamic method for measuring PSV is expected to yield higher DP values than the static method, since it includes the pressure necessary to overcome the airway resistance.
Clinical implicationsDistending pressure represents the cyclic deformation to which the respiratory systems is subjected during each ventilation, and is regarded as a main mortality factor during assisted/controlled MV. In PSV, this deformation does not only depend on the programmed parameters and the mechanical properties of the respiratory system, but also on muscle effort. Thus, the estimation of DP in PSV represents an alternative for the monitoring of ventilation and its potential impact upon the development of patient self-inflicted lung injury (P-SILI). Although there is not enough evidence to recommend a specific cut-off value for DP during PSV, a value of <15 cmH2O is considered safe,8 while >20–25 cmH2O alerts us of the risk of damaging ventilation. Based on our experience, however, in late phases of MV and especially in lungs presenting fibrotic remodeling, it is possible to find high DP values.
Likewise, adequate respiratory effort is crucial for favoring protective pulmonary and diaphragmatic ventilation. Both extremes – excessive and insufficient – have been associated to structural and functional diaphragmatic damage.9 To date, no prospective studies have evaluated the use of △Pocc as a predictor of Pmus and of PMI for the assessment of respiratory effort. Nevertheless, their use in combination with other noninvasive methods for the evaluation of the respiratory center and effort,10 such as P0.1, could optimize ventilatory therapy (Table 2).
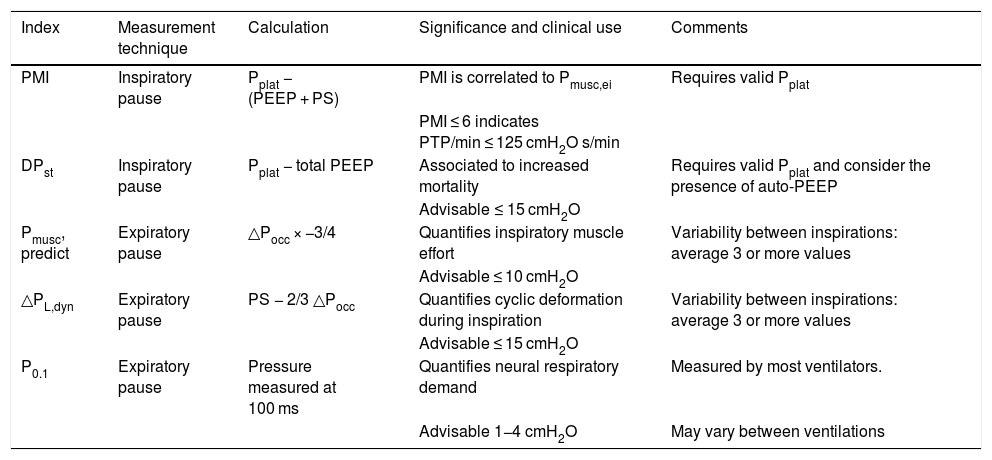
Different distending pressure and muscle effort indices evaluable in clinical practice during pressure support ventilation.
| Index | Measurement technique | Calculation | Significance and clinical use | Comments |
|---|---|---|---|---|
| PMI | Inspiratory pause | Pplat − (PEEP + PS) | PMI is correlated to Pmusc,ei | Requires valid Pplat |
| PMI ≤ 6 indicates PTP/min ≤ 125 cmH2O s/min | ||||
| DPst | Inspiratory pause | Pplat − total PEEP | Associated to increased mortality | Requires valid Pplat and consider the presence of auto-PEEP |
| Advisable ≤ 15 cmH2O | ||||
| Pmusc, predict | Expiratory pause | △Pocc × −3/4 | Quantifies inspiratory muscle effort | Variability between inspirations: average 3 or more values |
| Advisable ≤ 10 cmH2O | ||||
| △PL,dyn | Expiratory pause | PS − 2/3 △Pocc | Quantifies cyclic deformation during inspiration | Variability between inspirations: average 3 or more values |
| Advisable ≤ 15 cmH2O | ||||
| P0.1 | Expiratory pause | Pressure measured at 100 ms | Quantifies neural respiratory demand | Measured by most ventilators. |
| Advisable 1−4 cmH2O | May vary between ventilations |
P0.1: occlusion pressure at the first 100 ms; DPst: static distending pressure; △PL,dyn: dynamic transpulmonary pressure; PMI: pressure muscle index; Pmusc,ei: end-inspiratory respiratory muscle pressure; Pmusc,predict: predicted respiratory muscle pressure; △Pocc: airway pressure during expiratory occlusion; PTP/min: pressure x time per minute product.
Inspiratory and expiratory pause maneuvers during PSV are feasible in clinical practice and could be used as a tool for monitoring DP and respiratory effort. The impact of a ventilation strategy guided by these measurements upon the clinical outcomes is still unclear.
Conflict of interestThere is no conflict of interests with the disclosure.
Thanks are due to Dr. Guillermo Bugedo (Assistant Professor of the Department of Intensive Care Medicine, Pontificia Universidad Católica de Chile) for his valuable feedback on the manuscript.
Please cite this article as: Pavez N, Damiani LF. Pausa inspiratoria y espiratoria durante la ventilación con presión de soporte: Maniobras que debemos incorporar en la práctica clínica. Med Intensiva. 2022;46:213–216.