Hemorrhage is the leading cause of preventable death within the first few hours of standard care to patients with severe traumatic disease. Up to 50% of all deaths reported within the first 24 hours after sustaining trauma are due to bleeding. A recent analysis of the main multicenter clinical trials on severe trauma and hemorrhagic shock demonstrated that 73% to 91% of all deaths occurred within the first 6 hours after sustaining trauma.1 On the other hand, a study of 4596 autopsies due to combat trauma demonstrated that 24% of all deaths could have been avoided.2 Among them, 91% of the deaths were due to hemorrhages, most of them located at the chest and barely 9% due to problems with the airway or the ventilation.2
Resuscitation in patients with traumatic critical hemorrhage (TCH) is one of the biggest challenges associated with the management of trauma patients due to the complex and multifactorial etiopathogenesis of its complication and coagulopathy associated with trauma.3 Therefore, although the overall mortality rate of this population has dropped over the last decade, especially at the expense of a lower prehospital mortality rate, and also within the first 3-24 hours after sustaining trauma,4 certain challenges still remain in the management and treatment of TCH including its definition, pathophyisiological aspects, monitorization, bleeding control, and type of early transfusion.
DefinitionIn all detail, critical hemorrhage is defined as a bleeding that threatens the life of patients. However, in the current setting, authors suggest a pragmatic definition of TCH whose associated characteristics are shown on Table 1.
Diagnostic criteria proposed for the management of traumatic critical hemorrhage.
| Mechanism of traumatic action (often associated with a high-energy mechanism) |
| Physiological repercussion (hemodynamic instability, corresponds to shock index ≥ 1, classes III and IV) |
| Association of prehospital or hospital activation to a massive bleeding control protocol |
| Need for «life-saving» maneuvers like emergency surgery, angioembolization or use of other devices of external or vascular compression |
Applying this definition to the ICU Trauma Registry database‒RETRAUCI‒, nearly 6% of the patients admitted to our ICUs due to trauma have TCH, which is followed by an in-hospital mortality rate of 35%. However, that mortality is only associated with patients admitted to the ICU meaning that the actual mortality rate of this population is probably much higher.
Pathophysiology-endotheliumCoagulopathy associated with trauma affects nearly a third of all patients with hemorrhagic shock. There are several analytical criteria based on different conventional analytical tests (INR > 1.2, thrombocytopenia < 100 000/μL, plasma fibrinogen < 1.5-2.0 g/L), and viscoelastic tests (EXTEM CA5 ≤ 40 mm, and/or FIBTEM CA5 ≤ 9 mm) indicative of trauma related coagulopathy.5 Also, the elevated levels of syndecan-1, an indicator of endothelial glycocalyx degradation, were also associated with inflammatory parameters, coagulopathy, and mortality.6 Experimentally, some therapies commonly used have proven effective restoring the integrity of endothelial glycocalyx like the administration of fresh plasma, and the ultra-fast administration (< 60 min) of tranexamic acid7 which justifies, in part, its potential beneficial clinical effects. The next few years different strategies will probably be implemented on this regard.
MonitorizationThe clinical practice guidelines published by the Eastern Association for the Surgery of Trauma recommend using viscoelastic tests during resuscitation of trauma patients with active bleeding to minimize the transfusion of hemoderivatives. Reducing the number of «life-saving» maneuvers like surgical procedures or angioembolization has proven beneficial too. However, there is not a clear translation of this regarding the reduction of mortality rate.8 Also, the European guidelines for the management of bleeding and traumatic coagulopathy recommend that the routine clinical practice should use a combination of conventional lab tests, point-of-care TP/INR, and viscoelastic tests (Grade 1C recommendation).9 However, the ambitious multicenter ITACTIC clinical trial has been published recently. It included 392 patients with severe trauma and hemorrhagic shock but did not find any differences regarding survival 24 h and 90 days after trauma in patients resuscitated with conventional tests compared to viscoelastic tests.10 For all these reasons, the exact role played by the different viscoelastic tests in the group of patients with severe trauma is still to be determined beyond its clear effects on the use of resources. In the authors’ opinion, resuscitation with damage control and the implementation of massive bleeding protocols in our ICUs is far beyond the debate over the transfusion ratios. In this context, monitoring resuscitation using viscoelastic tests probably facilitates the identification of the specific deficit of coagulation factors for eventual replenishment purposes. However, to accomplish this, organization, training, and experience are needed to identify the group of patients that would benefit the most.
Bleeding controlThe use of the resuscitative endovascular balloon occlusion of the aorta (REBOA) is one of the latest tools in the management of patients with exsanguinating torso due to trauma. The fast deployment of the REBOA catheter allows us to increase central aortic pressure, perfuse brain and heart, and increase postload. At the same time, it stops the bleeding below compression, and eventually gives us 30 to 60 minutes before definitive hemostasis with other measures can be performed. Therefore, a systematic review demonstrated its benefits over the hemodynamic situation of patients with hemorrhagic shock,11 without any clear benefits regarding survival.12 Also, we should mention the high rate of complications seen,12 something we should really pay attention to in our setting where experience on this regard is scarce‒a few cases only.13 Despite of this, the clinical practice guidelines recently published by the European Resuscitation Council include the use of the REBOA catheter for the management of cardiopulmonary periarrest due to trauma.14 However, in our opinion, the definitive role it will play in hemorrhage control in our setting will be determined in the years to come. Still, extensive training, the right selection of patients, and more scientific evidence supporting its benefits regarding survival will be needed before being included in the routine clinical practice.
On the other hand, the use of tourniquets or hemostatic dressings is something common in a combat setting. However, the heterogeneity of the results available and the high risk of bias complicate their use in the civilian context.15 However, tourniquets have already made it to the prehospital setting and their use to stop bleeding from the limbs has gained a Grade 1B recommendation9 while the use of new hemostatic dressings to reduce the time elapsed until bleeding control15 will probably be the next step in this context.
Type of early transfusionProtocols for the management of massive bleeding always try to balance the transfusion of different blood derivatives with the right supplementation of coagulation factors. In this context, combat medicine teaches us that we should bring the moment of trauma and the moment of whole blood transfusion closer together since it has all the necessary elements for homeostasis at almost physiological concentrations.16 Although appealing, doing this is challenging from so many different levels: organizational, healthcare related, and even legal. Also, evidence is still scarce to justify its use in the civilian setting.
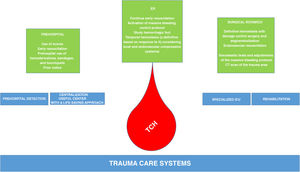
In conclusion, TCH is the leading cause of preventable death in patients with severe traumatic disease. Over the next few years, the role played by therapies to restore the integrity of endothelial glycocalyx, viscoelastic tests, endovascular compression techniques, external compression, and early use of whole blood will need to be determined. Everything will be part of the comprehensive management of patients with TCH from the prehospital, ER, surgical room, ICU, and hospitalization settings (Fig. 1).
Conflicts of interestJuan Antonio Llompart-Pou declared no conflicts of interest associated with this manuscript.
Mario Chico-Fernández received honoraria from Innovasc for providing training.
The authors wish to thank all lecturers and attendees to the Traumatic Critical Hemorrhage Day for their enthusiastic and unselfish participation.
Please cite this article as: Llompart-Pou JA, Chico-Fernández M. Hemorragia crítica traumática. Retos futuros. Med Intensiva. 2022;46:217–220.