Intensive care to facilitate organ donation (ICOD) is defined as the initiation or continuation of life-sustaining measures, such as mechanical ventilation, in patients with a devastating brain injury with high probability of evolving to brain death and in whom curative treatment has been completely dismissed and considered futile.
ICOD incorporates the option to organ donation allowing a holistic approach to end-of-life care, consistent with the patients wills and values. Should the patient not evolve to brain death, life-supportive treatment must be withdrawal and controlled asystolia donation could be evaluated.
ICOD is a legitimate practice, within the ethical and legal regulations that contributes increasing the accessibility of patients to transplantation, promoting health by increasing deceased donation by 24%, and with a mean of 2.3 organs transplanted per donor, and collaborating with the sustainability of health-care system.
This ONT-SEMICYUC recommendations provide a guide to facilitate an ICOD harmonized practice in Spanish ICUs.
Los cuidados intensivos orientados a la donación (CIOD) se definen como el inicio o la continuación de medidas de soporte vital, incluyendo la ventilación mecánica, en pacientes con lesión cerebral catastrófica y alta probabilidad de evolucionar a muerte encefálica, en los que se ha descartado cualquier tipo de tratamiento.
Los CIOD incorporan la opción de la donación de órganos permitiendo un enfoque holístico en los cuidados al final de la vida coherente con los deseos y valores del paciente. Si el paciente no evoluciona a muerte encefálica, se deben retirar las medidas de soporte vital valorando la donación en asistolia controlada.
Los CIOD respetan el marco ético y legal y contribuyen a aumentar las probabilidades de los pacientes de acceder a la terapia de trasplante, generando salud, incrementando la donación en un 24% con una media de 2,3 órganos trasplantados por donante y contribuyendo a la sostenibilidad del sistema sanitario.
Estas recomendaciones ONT-SEMICYUC proporcionan una guía para facilitar una práctica armonizada de los CIOD en las UCI españolas.
Intensive care to facilitate organ donation (ICOD) involves the adoption of life support measures, including invasive mechanical ventilation, with no therapeutic purpose, in patients with catastrophic brain damage, with the aim of avoiding imminent cardiorespiratory arrest and thus allowing progression toward brain death (BD) with a view to facilitating the possibility of organ donation in end-of-life care.
Intensive care to facilitate organ donation is only considered when any treatment by the team in charge of caring for the patient is considered to be futile, and requires prior evaluation of the probability of evolution toward BD, the exclusion of medical contraindications, and an interview with the family or representatives of the patient, in order to assess the patient will regarding organ donation and obtain consent to the procedure1,2.
Intensive care to facilitate organ donation refers not only to the start of supportive measures to facilitate organ donation but also to the prolongation of such measures in patients admitted to the Intensive Care Unit (ICU) with curative intent, and in which a poor subsequent clinical course confirms the futility of maintaining such measures.
The present study describes the recommendations on ICOD developed by an ad hoc working group of specialists in Intensive Care Medicine under the auspices of the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias [SEMICYUC]) and the Spanish National Transplantation Organization (Organización Nacional de Trasplantes [ONT])1, and complements these recommendations with a number of clinical cases.
BackgroundIn 1988, the Royal Devon and Exeter Hospital adopted a protocol for the identification of patients in deep coma secondary to a cerebrovascular accident and without options for cure, admitted to the emergency service or hospital ward. After due evaluation and consultation with the family, the patient was intubated at the time when cardiorespiratory arrest proved imminent, and was moved to the ICU for organ donation purposes. This protocol made it possible to double the number of donations of the hospital and was held to be promising in view of the potential increase in donations in the event the protocol were implemented on a nationwide basis3.
The mentioned procedure was referred to as “elective ventilation” (EV) or “non-therapeutic elective ventilation”, and generated an intense ethical debate that reached institutional levels. Despite support from the British Medical Association4, the practice was rejected by the Society of Intensive Care Medicine5, and its legality was even questioned on the grounds of a restrictive interpretation of represented consent. Finally, in October 1994, the British Ministry of Health issued a guideline considering EV to be illegal – thereby putting an end to its practice6. Although the debate continued7, two decades went by before EV was again applied in the United Kingdom8,9.
In Spain, in the year 2003, and following approval from its clinical Ethics Committee, Gregorio Marañón Hospital in Madrid started a protocol for consideration as possible donors, and with admission to the ICU, of those patients with irreversible massive brain hemorrhage who otherwise would have died of cardiorespiratory arrest in the Emergency Service10. The initial experience proved encouraging: during the first two years, the procedure resulted in 15 donations, representing 30% of all donations in the hospital. Seventy-six percent of the interviewed families authorized intubation and admission to the ICU to facilitate donation, and the mean time from admission to the Unit to the diagnosis of BD was 15h (De la Calle B, Pascual M, Tomey MJ. Admission to the ICU as possible donors of patients with irreversible massive brain hemorrhage, a two-year experience [Ingreso en UCI como potencial donante, de pacientes en situación irrecuperable por hemorragia cerebral extensa, experiencia de dos años]. XX National Meeting of Transplantation Coordinators. Valladolid, 4–6 May 2005, personal communication).
In 2006, San Pedro de La Rioja Hospital developed a procedure for the detection and management of possible donors in the Emergency Service, with subsequent admission to the ICU for donation, and which doubled the number of donors in the hospital11,12. This experience marked the start of institutional collaboration between the ONT and the Spanish Society of Emergency Care and Emergencies (Sociedad Española de Medicina de Urgencias y Emergencias), with the drafting of a document containing recommendations to facilitate the identification of possible organ donors from the hospital emergency care setting and optimize their management13.
Over time, admission to the ICU of patients with catastrophic brain damage for donation purposes spread to many centers throughout the country. The ethical particulars and technical difficulties inherent to the procedure advised the development of a series of recommendations in order to homogenize and improve this practice. These recommendations were published in 2017 in a document produced by a working group composed of experts designated by the SEMICYUC and ONT1. This document coined the term “ICOD”, which refers to both the start of supportive measures with donation intent (the EV strategy of the Anglo-Saxon literature) and to the prolongation of such measures once they have become futile – since both situations must be guided by the same ethical principles and technical considerations.
At present, ICOD is a reality in many countries in our setting14,15. In Spain, the practice has been formally recommended by the SEMICYUC16, is performed on a generalized basis in Spanish ICUs17, and generates 24% of all organ donations – with 2.3 transplanted organs per donor18.
Legal, ethical and deontological contextIntensive care to facilitate organ donation abides with Spanish legislation – the reference legal documents being those referred to end-of-life decision making and the harvesting and clinical use of organs and tissues of human origin19–22.
Respect for the principle of autonomy is a crucial principle for the clinical team in charge of a patient with catastrophic brain damage when considering the possibility of donation, once curative treatment has been discarded and the aim of management is reoriented toward end-of-life care. This principal requires the professionals to explore patient will referred to donation, checking whether such a will was made known to other persons or through the means contemplated by law, such as the advance directive or living will registry23. If there is an advance directive specification against organ donation, the option of ICOD will not be considered. The healthcare professional in charge must ensure an adequate informative process for the family before obtaining represented consent to ICOD. The responsibility of the professional to facilitate patient access to transplantation therapy is the second principle that must be considered in relation to donation in the end-of-life care setting.
From the ethical perspective, an ICOD program is respectful of the principle of autonomy, since it allows inclusion of the patient will in the care process, including those instructions referred to the destination of body and organs, and taking into account the moral values and living principles of the individual. With regard to the family of the possible donor, organ donation can provide consolation in the face of loss, and an opportunity to express values such as solidarity and social commitment. In turn, as regards the patients on the transplant waiting list, ICOD, by offering the possibility of organ donation, can improve their survival and quality of life16,24–28.
The use of ICU resources necessary for ICOD is justified not only by the clinical benefits derived from transplantation but also by its contribution to the sustainability of the healthcare system, since kidney transplantation for example is a cost-effective procedure29.
Intensive care to facilitate organ donation must be performed respecting the dignity of the patients and recognizing their option for donation, but always ensuring the absence of maleficence. At all times we must ensure the absence of suffering and guarantee patient wellbeing30–32. If the potential donor does not progress to BD in the period of time commented with the family, or if the family does not wish to prolong the wait, patient care must be exclusively redirected toward measures of wellbeing, with withdrawal of the rest of measures and devices, in order to allow the disease process to follow its natural course9,33,34. In this regard, emphasis is placed on the need to adequately select possible donors on the basis of their high probability of progressing toward BD in a short period of time.
Intensive care to facilitate organ donation abides with the medical deontological code of the Spanish Medical Collegiate Organization, which is considered mandatory. According to the mentioned code, physicians have the duty to encourage and promote organ donation. Other duties are referred to information and communication for decision making; care of the health of the individual and of the community; respect for human life and personal dignity; and the provision of end-of-life care. These fundamental duties of the physician imply that ICOD is based on medical deontological principles and can be regarded as part of medical practice as such35.
The SEMICYUC possesses an ethical code referred to the practice of Intensive Care Medicine. In relation to patient autonomy, the code underscores the importance of informed consent, the living will, and the right to die with dignity. The right to information for represented decision making is also emphasized. The code calls for guaranteeing the quality of healthcare in accordance with the state of knowledge at the time, ensuring efficient management of the available resources as an ethical principle of distributive fairness. Lastly, it explicitly establishes the responsibility of the intensive care professionals to facilitate organ donation, thereby also encompassing ICOD within the ethical code of the SEMICYUC36.
Summary of the ONT-SEMICYUC recommendations on ICOD and clinical–radiological predictors of progression toward brain deathThe evaluation of a patient as a candidate for ICOD is based on the probability of progression toward BD in a short period of time, with the exclusion of possible medical contraindications to organ donation. If progression toward BD is considered unlikely, or in the presence of absolute medical contraindications, the possibility of ICOD should not be contemplated.
Once the decision has been made to not continue medical or surgical treatment with healing intent, the option of donation should be considered on a systematic basis. In practice, this means reporting the case to the transplantation coordinator (TC) of the center – this in turn being facilitated by the existence of clear consensus-based referral criteria and of a fluid mechanism of communication with the TC.
According to the United States Neurocritical Care Society, the definition of “devastating brain damage” or “catastrophic brain damage” includes patients with neurological brain injuries (of neurological origin) that pose an immediate threat to life, and those with severe brain damage in which the initial decision is made to limit treatment of the disease itself and place priority on other types of care, such as the ensuring of wellbeing32.
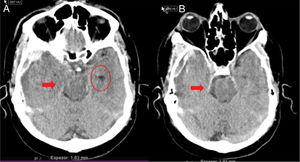
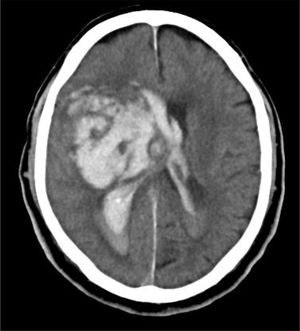
In clinical practice, before establishing a definitive prognosis, it is advisable to have the opinion of an expert multidisciplinary team, with the aim of minimizing personal bias. The specialist in Intensive Care Medicine, thanks to his/her knowledge of neurocritical disease, play a key role in this regard. Catastrophic brain damage results in an elevation of intracranial pressure (ICP), with a decrease in brain perfusion pressure, and the gradual development of brain circulatory arrest. The probability of progression toward BD must be based on clinical data, neuromonitoring information and the brain computed tomography (CT) findings. Firstly, the clinical neurological condition must be considered, based on the usual severity scales according to the different types of disease (Glasgow Coma Score [GCS], Hunt and Hess classification, NIHSS), along with the absence of certain brainstem reflexes. The severity scales used in the first hours of injury have limitations, and their prognostic usefulness increases when they are applied after patient resuscitation. The probability of prognostic error is always less when these scales yield an extreme score: the greater the clinical severity, the greater the probability of progression toward BD37. In this respect, some studies have found that the abolition of three brainstem reflexes upon admission is the parameter that most predicts progression toward BD38. Another prognostic factor that may be of help in predicting a strong probability of progression toward BD is brain CT evaluation, since this imaging technique allows us to document the type, volume, location and severity of the structural damage, as well as the presence of signs of intracranial hypertension and cerebral herniation. In the case of brain hemorrhage, hematoma volume is one of the strongest predictors of progression toward BD, and some authors point to a volume of over 65ml as a determinant factor in this respect39. Likewise, the presence of the “whirl sign” on the CT scan without contrast injection, and of the “spot sign” in the angiographic CT study, is indicative of the presence of active arteriolar or venular bleeding, and suggests a poor prognosis, which some authors associate to an increased probability of progression toward BD38,40,41. Displacement of the midline informs us about the degree of compression, and together with the condition of the basal cisterns, helps to assess involvement of the brain structures. Partial or total erasure of the basal cisterns is a strong indicator of probable progression toward BD42. The presence of signs of brain herniation on the CT scan implies intracranial hypertension and thus a high risk of hernial wedging of the brain. The three most common forms of cerebral herniation are: subfalcine herniation, which is characterized by displacement of the midline and compression of the ipsilateral lateral ventricle (Fig. 1); uncal or transtentorial herniation, characterized by dilatation of the cistern of the ipsilateral pontocerebellar angle and temporal horn of the contralateral lateral ventricle (Fig. 2); and amygdaline or tonsillar herniation, characterized by disappearance of the cisterna magna and descent of the cerebellar tonsils or amygdala below the Chamberlain line. The sheath of the optic nerve continues with the meningeal elements of the central nervous system and accumulates cerebrospinal fluid (CSF) within this subarachnoid space, causing an increase in its diameter in the presence of elevated ICP. The diameter can be measured by ultrasound, magnetic resonance imaging (MRI) or brain CT, and although there is no general agreement as to the exact site to obtain the measurement or the diameter cut-off value defining intracranial hypertension, some authors consider an optic nerve sheath diameter of over 5–6mm to be strongly correlated to an ICP of over 20mmHg43,44.
Uncal or transtentorial herniation. (A) Collapse of the temporal horn and cisterna ambiens ipsilateral to the expansive lesion (arrow). Dilatation of the contralateral temporal horn (circle). (B) Dilatation of the ipsilateral cerebellopontine cistern (arrow) (courtesy of Ángela Meilán, Department of Radiology, Hospital Universitario Central de Asturias).
Transcranial doppler ultrasound (TCD) can also be useful for assessing the hemodynamic condition of the brain and estimating the neurological course. The rise in ICP initially induces an increase in peak systolic velocity secondary to the reflex elevation of systolic contractility – incrementing the difference between the peak systolic velocity and the end diastolic velocity, and thus elevating the pulsatility index. If the ICP continues to rise, the end diastolic velocity progressively decreases, giving rise to a “systolized” pattern, followed by complete disappearance of the diastole. Although there is no mathematical model capable of precisely predicting the calculation of ICP from the TCD study, the increase in ICP, and thus the prediction of progression toward BD by TCD, is determined by the decrease in mean brain blood flow velocity, the presence of a highly “systolized” pattern, and the increase in pulsatility index. Lastly, the typical patterns of brain circulatory arrest accompanying BD are inverted diastolic flow or reverberant flow, and the systolic spikes pattern45.
Selection of the possible donor in relation to the absence of contraindications to donation initially should be based on the data available from the case history, interviewing of the family, and the complementary tests.
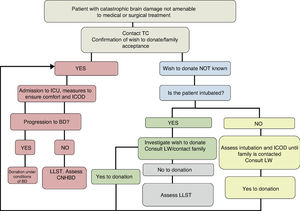
In sum, the decision referred to patient admission to the ICU for ICOD should be made by an expert multidisciplinary team, with individual assessment of each patient based on the available scientific evidence, analyzing the global clinical situation according to the current prognostic models/severity scales, brain CT, TCD, clinical experience, and the patient preferences expressed either in person or by others on a delegated basis (Fig. 3).
Once in the ICU, it is essential to ensure patient comfort and wellbeing. Analgesia and sedation should be provided, if required, using drugs and doses that do not interfere with the diagnosis of BD. Patient management should be oriented toward adequate organ preservation, avoiding any added measures that are considered to be futile46. During admission, evaluation of the possible donor and of the organs that may be harvested for transplantation should be completed. Once BD has been diagnosed, routine consent to organ harvesting is to be obtained. If the patient does not progress toward BD in the agreed period of time, or if the family does not wish to continue the supportive measures for donation purposes, the option of controlled non-heart beating donation may be considered.
Clinical casesThree clinical cases corresponding to patients admitted to the ICU for ICOD are presented below.
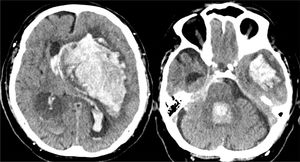
Case 1A 76-year-old male with no disease history of relevance experienced sudden impaired consciousness at home, with GCS 4 (O1, V1, M2). The stroke protocol was activated, and the patient was intubated by the out-hospital emergency service. Upon admission to hospital, the brain CT scan revealed massive hemorrhage of the left basal ganglia, opening to the ventricles, important brain edema and signs of brain herniation (Fig. 4). The situation was assessed by the Department of Neurosurgery and the ICU, and in view of the clinical condition and brain CT findings, treatment was discarded. There was no living will. The family was informed, and a prior interview was held in the emergency service. The family accepted patient admission to the ICU with the sole purpose of organ donation. The patient progressed to BD within 28h and donated the liver. The transplant recipient showed a good clinical course and was discharged from the ICU on day four post-transplantation.
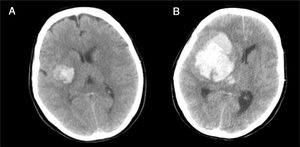
Case 2This was a 65-year-old woman with a history of arterial hypertension and ischemic heart disease, subjected to antihypertensive and antiplatelet drug treatment. She presented left hemiplegia and dysarthria, with GCS 14. The brain CT scan revealed minor hemorrhage affecting the right basal ganglia (Fig. 5A); admission to the stroke unit for control was decided. After 4h the patient suffered a hypertensive crisis, impaired consciousness with GCS 6 (O1, V1, M4) and anisocoria with non-reactive right mydriasis. Repeat CT revealed massive right hemispheric bleeding (Fig. 5B), with signs of subfalcine herniation. The patient was admitted to the ICU, and in view of the seriousness of the condition, treatment measures were ruled out. The family and the TC were notified, and the patient was seen to have a living will specifying her wish to serve as an organ donor. This was reported to the family, which accepted the continuation of ICOD and the desire of the patient. Brain death was confirmed 15h after admission, and the liver and both kidneys were harvested and successfully transplanted.
(A) Initial brain CT scan revealing minor hemorrhage affecting the right basal ganglia, with partial collapse of the ipsilateral ventricular system. (B) Repeat CT scan 4h after the first, showing massive right hemispheric hemorrhage, ventricular invasion and signs of subfalcine herniation.
A 79-year-old male suffered sudden loss of consciousness at home. The emergency service evidenced GCS 4 (O1, V1, M2), non-reactive pupils and a blood pressure of 205/115mmHg. Tracheal intubation was performed and the patient was taken to hospital. In the emergency room he presented GCS 4 with abolished photomotor, corneal and oculocephalic reflexes. The brain CT scan revealed an intraparenchymal hematoma in the right basal ganglia, with midline displacement and invasion of the ventricular system (Fig. 6). The case was assessed by Neurosurgery and Neurology, and treatment was discarded. The TC discussed the possibility of organ donation with the family, which accepted admission of the patient to the ICU for donation under conditions of BD. After 48h the patient remained in non-reactive coma with abolished photomotor, corneal and oculocephalic reflexes, but with persistent cough reflex and spontaneous breathing. The family did not want to prolong the situation, and ventilatory support was therefore suspended. The option of controlled non-heart beating donation was then proposed, and was authorized by the family. The kidneys and corneas were harvested. The kidneys were transplanted, with immediate renal function and a good subsequent course.
ConclusionsIntensive care to facilitate organ donation is a legitimate practice that is observant of our legal, ethical and deontological norms. It allows a holistic approach to end-of-life care, respecting the general interests of the patient (if donation is consistent with his/her wishes and values), while palliative care is provided adjusted to the changing needs of the subject. At the same time, ICOD increases the transplantation options for patients on the waiting list – with the resulting health impact and contribution to sustainability of the system. The recommendations of the ONT-SEMICYUC regarding ICOD seek to offer a guide to ensure practices that are harmonized and coherent with our regulatory framework.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Escudero Augusto D, Martínez Soba F, de la Calle B, Pérez Blanco A, Estébanez B, Velasco J, et al. Cuidados intensivos orientados a la donación de órganos. Recomendaciones ONT-SEMICYUC. Med Intensiva. 2021;45:234–242.