To explore the training, ability and attitudes toward cardiopulmonary resuscitation and the use of automatic defibrillators among the population of the Basque Country (Spain).
DesignA face-to-face survey.
ScopeCapital cities of the Basque Country.
ParticipantsA total of 605 people between 15–64 years of age were randomly selected.
Main variables of interestInformation about the knowledge, perceptions and self-perceived ability to identify and assist cardiopulmonary arrest was requested.
ResultsA total of 56.4% of the responders were women, 61.8% were occupationally active, and 48.3% had higher education. Thirty-seven percent of the responders claimed to be trained in resuscitation techniques, but only 20.2% considered themselves able to apply such techniques. Public servants were almost 4 times more likely of being trained in defibrillation compared to the rest of workers (OR 3.7; p<0.001), while people with elementary studies or no studies were almost 3 times more likely of not being trained in cardiopulmonary resuscitation, in comparison with the rest (OR 2.7; p=0.001). A total of 94.7% of the responders considered it “quite or very important” for the general population to be able to apply resuscitation, though 55% considered themselves unable to identify an eye witnessed cardiac arrest, and 40.3% would not recognize a public-access defibrillator.
ConclusionsCitizens of the Basque Country consider the early identification and treatment of cardiorespiratory arrest victims to be important, though their knowledge in cardiopulmonary resuscitation and defibrillation is limited.
Explorar la formación, la capacitación autopercibida y las actitudes de la población del País Vasco sobre la resucitación cardiopulmonar y el uso de desfibriladores automatizados.
DiseñoEncuesta heteroadministrada a pie de calle.
ÁmbitoCapitales de provincia del País Vasco.
ParticipantesSeiscientas cinco personas de entre 15 y 64 años, seleccionadas mediante muestreo aleatorio estratificado por edad.
Variables de interés principalesNivel de formación recibida, capacitación autopercibida y percepciones y actitudes para identificar y asistir a una persona en parada cardiorrespiratoria.
ResultadosEl 56,4% de los encuestados eran mujeres, el 61,8% en situación laboral activa y el 48,3% poseía estudios superiores. El 37% refirió haberse formado en técnicas de resucitación, pero solo un 20,2% consideraba encontrarse capacitado para aplicarlas. Las personas que trabajan en la administración pública mostraron una probabilidad casi 4 veces mayor de estar formadas en desfibrilación que quienes trabajan en otros sectores (OR 3,7; p<0,001), mientras que aquellos con estudios elementales/sin estudios presentaron una probabilidad casi 3 veces mayor que el resto de no haberse formado en resucitación cardiopulmonar (OR 2,7; p=0,001). El 94,7% consideraba «bastante/muy importante» que la población fuese capaz de realizar una resucitación, pero el 55% declaró que no sabría identificar una parada cardiaca si la presenciase y el 40,3% no sabría reconocer un desfibrilador de acceso público.
ConclusionesLa ciudadanía del País Vasco considera importante saber identificar y tratar precozmente a una persona en parada cardiorrespiratoria, pero los conocimientos generales sobre resucitación cardiopulmonar y desfibrilación son pobres.
An average of 850 out-of-hospital cardiac arrest (OH-CA) episodes are recorded in the Basque Country (Spain) each year, and one-third of them occur outside the home of the patient. Despite the important efforts made by the emergency medical systems in the last decades, over 80% of all individuals suffering OH-CA die before reaching hospital.1
The best management strategy for OH-CA is the early application of a series of successive and coordinated actions known as the chain of survival, and which include early recognition of the emergency situation and activation of the medical emergency system; the application of basic cardiopulmonary resuscitation (CPR) maneuvers; early defibrillation; and the provision of specialized medical care. It is important to note that in addition to improving the response of the emergency medical services, this strategy implicates citizens in the protection of their own health, by leading them to participate in the first three links of the chain.2
The chances of surviving OH-CA depend on a range of factors, though the start of resuscitation by witnesses of the event before the arrival of the emergency medical service, and early defibrillation, are considered to be the measures that most influence the prognosis of cardiac arrest (CA) secondary to ventricular tachyarrhythmias, independently of the influence of other factors. Indeed, the adoption of such measures can double the patient survival rate after 30 days.3–5 Over a decade ago, the introduction of the first automated external defibrillators (AEDs) represented an important step toward optimizing the management of OH-CA in our community.
In Spain, although current state legislation establishes the conditions and minimum safety and quality requirements referred to the use of AEDs outside the healthcare setting,6 the different Autonomous Communities in the country are in charge of the mechanisms referred to the control and coordination of their use. In this respect, although regulations have been developed in most Communities,7 there is a lack of heterogeneity among the different regions in terms of the scope, requirements and elements of the programs or interventions related to AEDs–complicating access to these devices on the part of non-healthcare personnel in many regions.8 This situation therefore complicates the development of consensus-based strategies for the promotion of public access to AEDs as a measure for shortening the time to defibrillation in cases of CA.9
In the Basque Country, and since introduction of the first regulations referred to AEDs for non-medical personnel in 2005,10 there have been a number of legislative changes destined to spread and facilitate the access to such devices. Thus, in 2007, the use of AEDs was authorized for nursing personnel, and the training validity period for non-healthcare personnel was extended.11 Subsequently, in 2011, all citizens were acknowledged to be directly accredited to use AEDs, under the assumption that such interventions are contemplated within the basic CPR scheme.12 More recently, in a further step to spread and enhance public access to AEDs, a new legal measure has established the obligation to install such devices in certain public spaces outside the healthcare setting, such as large shopping surfaces; public facilities with a capacity of over 700 people; bus or railway stations in cities of over 50,000 inhabitants; subway, train or bus stations used by a daily average of 2000 people or more; and educational centers with 2000 people or more.13
Through the obligation to install AEDs in greatly visited public spaces, the Basque Government has established the possibility of improving the prognosis of patients with OH-CA. However, it must be taken into account that the survival of such patients is not intrinsically conditioned by the fact of increasing the number of public access AEDs, but rather by the rapid intervention and the knowledge of CPR maneuvering among the circumstantial witnesses of the acute event. Consequently, the aim of this study was to explore the training received, self-perceived capacitation, general knowledge and the perceptions and attitudes of the population of the Basque Country referred to CPR and the use of AEDs in dealing with people who suffer OH-CA.
Material and methodsA population-based, cross-sectional analytical components descriptive study was carried out.
The study included all people living in the Basque Country and aged between 15–64 years (reflecting the potentially active population age range). Individuals with a medical, nursing or healthcare emergency care education (whether completed or otherwise) were not included, in the same way as workers in the emergency medical transport sector. People with physical, language or cognitive impairments were also excluded.
The minimum sample size was estimated for a 95% confidence level and a margin of error of±4%, under the most unfavorable hypothesis of maximum indetermination (p=q=0.5). In order to guarantee representativeness of the sample and maintain the reference population proportions, stratification was carried out by age, contemplating three intervals (15–29, 30–49 and 50–64 years), and by province (Vizcaya, Guipuzcoa and Alava). Sample screening was performed on a randomized basis in the metropolitan settings of the three provincial capitals (Bilbao, San Sebastian and Vitoria), selecting as recruitment points those places requiring the installation of a public access AED as specified by Decree 9/2015, or which on the date of the survey already had such a device installed.
Data collection was carried out between May and June 2015, based on an anonymous structured questionnaire taking 5min to answer, and which was administered in person by the investigators and developers of the questionnaire.
The questionnaire was specifically developed for this study. A literature search was carried out to identify the topics to be evaluated, and the specific items were defined. The questionnaire comprised a number of sociodemographic variables (gender, age, educational level and profession) and a series of questions organized in relation to the categories “self-perceived capacitation to apply CPR maneuvers”, “basic training received in CPR techniques”, “general knowledge of CA and AED”, and “perceptions and attitudes toward CPR maneuvers”. Measurement of the operative variables referred to perceptions was based on closed-ended questions and a descriptive estimation scale (none, a little, quite a lot, a lot).
The validation of contents was carried out sequentially, with a review of the initial questionnaire by the group of investigators, and critical analysis by a group of experts. Lastly, a pilot trial involving 28 people was carried out to check the validity of the instrument in terms of adequate understanding on the part of the study subjects. The participants in the pilot trial were selected with no sampling criterion, though all of them were required to meet the abovementioned inclusion and exclusion criteria. At the end of this phase, we recorded the opinions and suggestions of the group of experts, of those in charge of data collection, and of the participants–introducing the opportune changes in the definitive questionnaire.
The reliability and stability over time of the final questionnaire was assessed by applying a test–retest protocol to the group of subjects that participated in the pilot trial, with an interval of two weeks between the two phases. The level of concordance (agreement) corresponding to each item was determined based on the Kappa coefficient–a value of >0.50 being regarded as acceptable. The anonymity of the questionnaire was maintained by using paired codes based on the last two digits and letter of the national identity card of each subject.
Qualitative variables were reported as absolute frequencies and proportions, while quantitative variables were presented as the median and interquartile range (IQR). Comparative testing was based on the chi-squared test and Mann–Whitney U-test (in view of the non-normal distribution of data as evidenced by the Shapiro–Wilk test). Statistical significance was considered for p<0.05. The magnitude of the association between variables with statistically significant associations was also examined by calculating the raw odds ratios (ORs) and corresponding 95% confidence intervals (95%CI).
The proportions were graphically displayed as bar charts with the respective 95%CI.
The SPSS® version 21 statistical package and OpenEpi® program were used throughout.
ResultsA total of 605 valid questionnaires were collected (52.9% from Vizcaya, 32.1% from Guipuzcoa and 15% from Alava). Of the surveyed individuals, 56.4% were women, 61.8% were actively employed, and 18.8% had elementary studies or no studies.
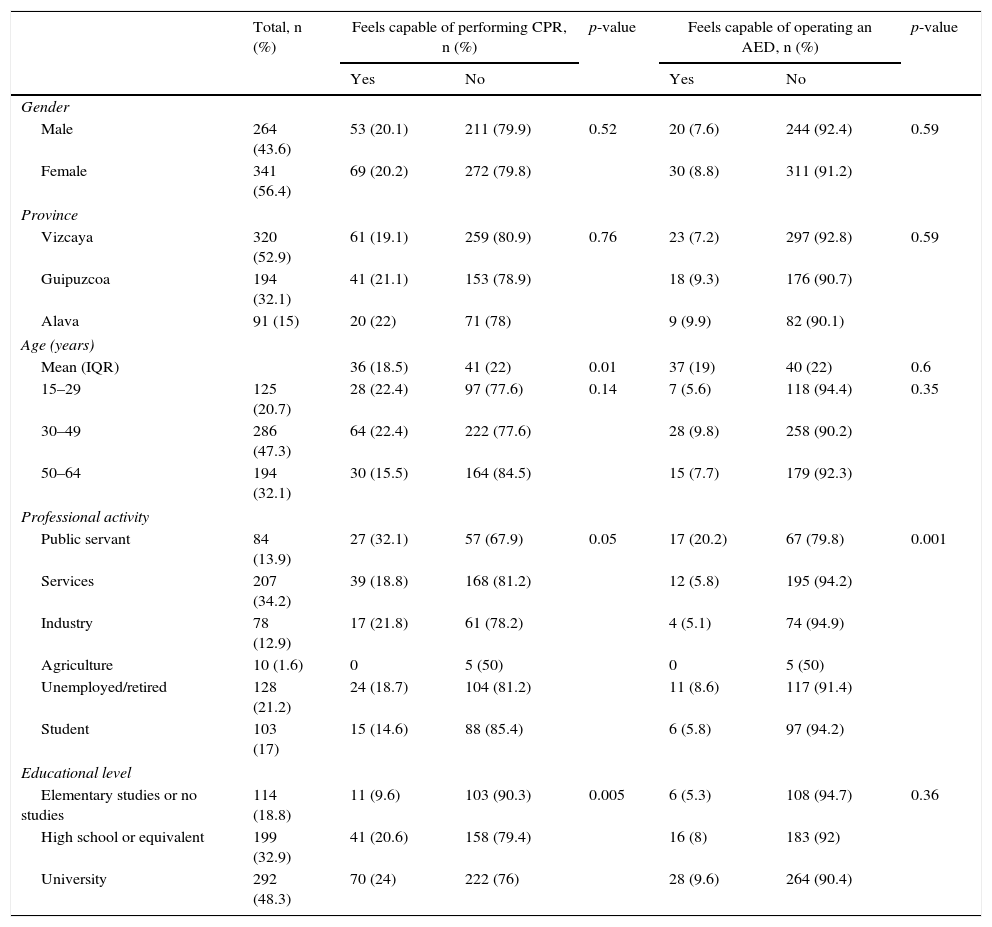
Self-perceived capacitation to apply resuscitation maneuvers in an adult patientA total of 20.2% of the surveyed individuals considered themselves capable of performing CPR–a figure that dropped to 8.3% when asked about capacitation to use an AED. Statistically significant differences were recorded on contrasting the median age of those who considered themselves to be trained and capable of applying CPR techniques versus those who did not–though no such differences were observed in the case of specific training in the use of AED or upon stratifying the sample into age intervals. Individuals working in the public administration (public servants) were almost four times more likely to feel capable of using an AED than those working in other sectors (OR 3.7; 95%CI 1.9–7), and people with elementary studies or no studies were almost three time more likely to feel unable to perform CPR techniques than the rest (OR 2.7; 95%CI 1.4–5.5). The remaining general characteristics of the sample and subject self-perception of the capacity to apply resuscitation maneuvers according to such characteristics are described in Table 1.
General characteristics of the study population and comparative analysis according to self-perceived capacitation to perform cardiopulmonary resuscitation or operate an automated external defibrillator in an adult patient (n=605).
| Total, n (%) | Feels capable of performing CPR, n (%) | p-value | Feels capable of operating an AED, n (%) | p-value | |||
|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | ||||
| Gender | |||||||
| Male | 264 (43.6) | 53 (20.1) | 211 (79.9) | 0.52 | 20 (7.6) | 244 (92.4) | 0.59 |
| Female | 341 (56.4) | 69 (20.2) | 272 (79.8) | 30 (8.8) | 311 (91.2) | ||
| Province | |||||||
| Vizcaya | 320 (52.9) | 61 (19.1) | 259 (80.9) | 0.76 | 23 (7.2) | 297 (92.8) | 0.59 |
| Guipuzcoa | 194 (32.1) | 41 (21.1) | 153 (78.9) | 18 (9.3) | 176 (90.7) | ||
| Alava | 91 (15) | 20 (22) | 71 (78) | 9 (9.9) | 82 (90.1) | ||
| Age (years) | |||||||
| Mean (IQR) | 36 (18.5) | 41 (22) | 0.01 | 37 (19) | 40 (22) | 0.6 | |
| 15–29 | 125 (20.7) | 28 (22.4) | 97 (77.6) | 0.14 | 7 (5.6) | 118 (94.4) | 0.35 |
| 30–49 | 286 (47.3) | 64 (22.4) | 222 (77.6) | 28 (9.8) | 258 (90.2) | ||
| 50–64 | 194 (32.1) | 30 (15.5) | 164 (84.5) | 15 (7.7) | 179 (92.3) | ||
| Professional activity | |||||||
| Public servant | 84 (13.9) | 27 (32.1) | 57 (67.9) | 0.05 | 17 (20.2) | 67 (79.8) | 0.001 |
| Services | 207 (34.2) | 39 (18.8) | 168 (81.2) | 12 (5.8) | 195 (94.2) | ||
| Industry | 78 (12.9) | 17 (21.8) | 61 (78.2) | 4 (5.1) | 74 (94.9) | ||
| Agriculture | 10 (1.6) | 0 | 5 (50) | 0 | 5 (50) | ||
| Unemployed/retired | 128 (21.2) | 24 (18.7) | 104 (81.2) | 11 (8.6) | 117 (91.4) | ||
| Student | 103 (17) | 15 (14.6) | 88 (85.4) | 6 (5.8) | 97 (94.2) | ||
| Educational level | |||||||
| Elementary studies or no studies | 114 (18.8) | 11 (9.6) | 103 (90.3) | 0.005 | 6 (5.3) | 108 (94.7) | 0.36 |
| High school or equivalent | 199 (32.9) | 41 (20.6) | 158 (79.4) | 16 (8) | 183 (92) | ||
| University | 292 (48.3) | 70 (24) | 222 (76) | 28 (9.6) | 264 (90.4) | ||
AED: automated external defibrillator; CPR: cardiopulmonary resuscitation; IQR: interquartile range.
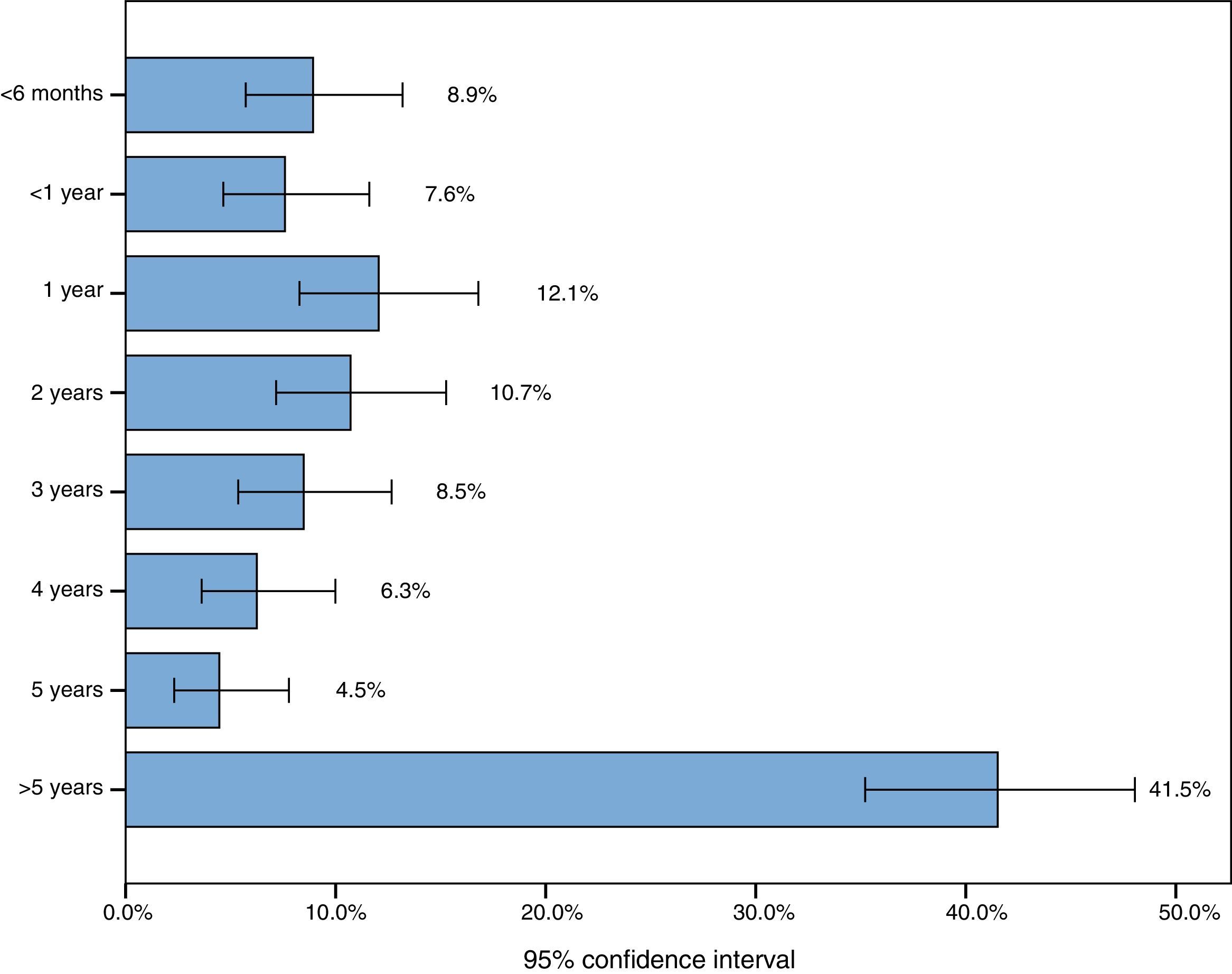
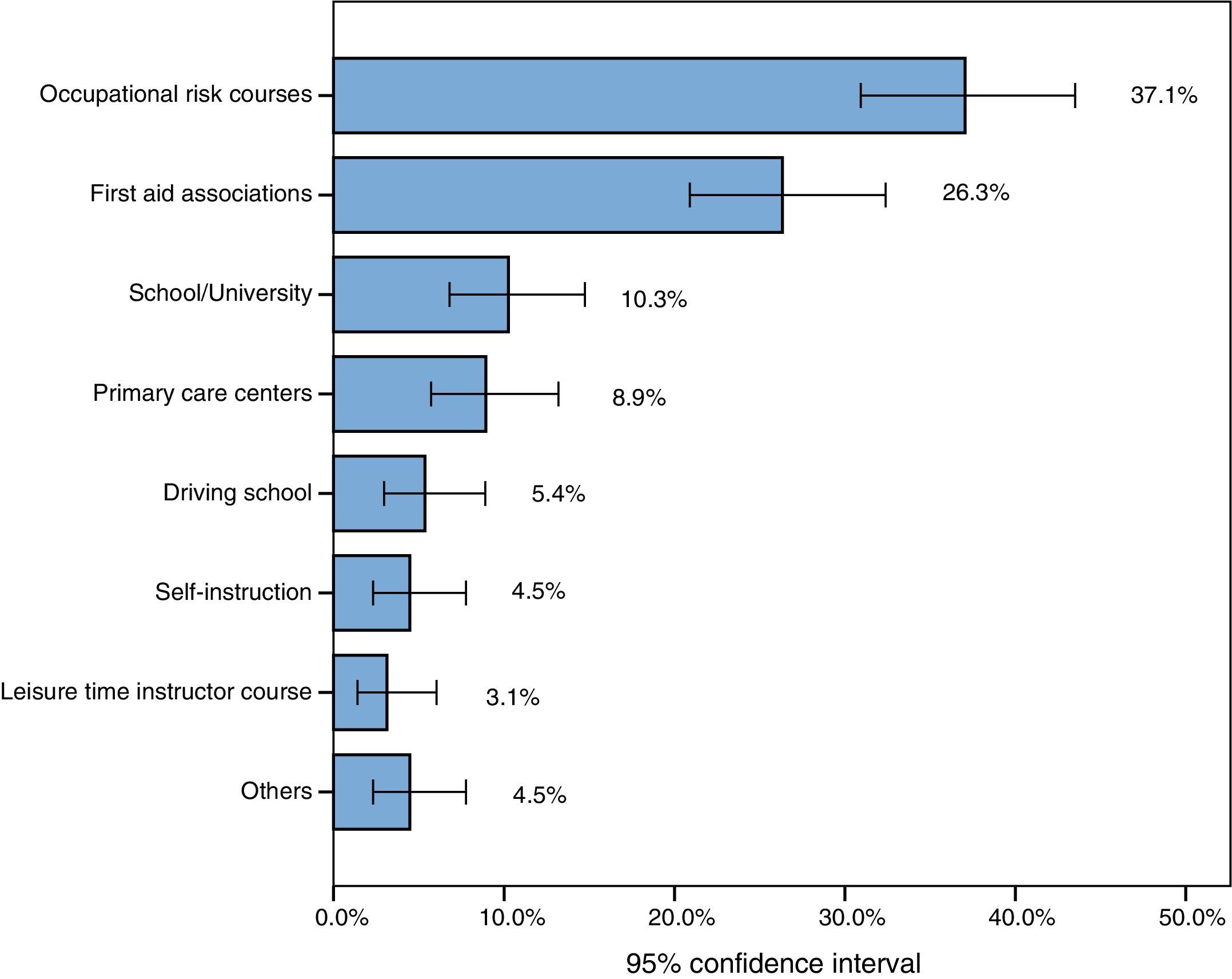
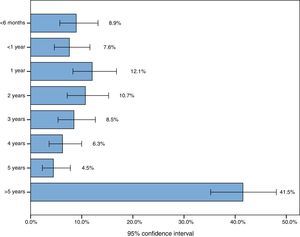
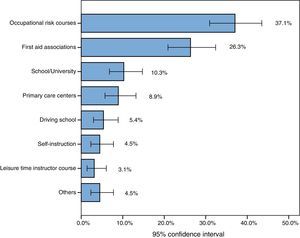
Independently of self-perceived capacitation, 224 subjects (37%) had received training in CPR and/or the management of AED in the past. Of the total people with training, 28.6% had last received instruction one year or less ago, while in 46% of the cases training had taken place 5 or more years ago (Fig. 1). The training programs fundamentally took place in the context of occupational risk prevention courses in the work (company) setting (37.1%), or in courses organized by emergency care associations (26.3%) such as the Red Cross. Only 10 people (4.5%) were self-instructed (Fig. 2).
Of the 378 people who had received no training in CPR (with or without AED support), 61.4% explained that they had not had any opportunity to receive training, 29.9% claimed to have little interest in the subject, and 7.7% claimed to have no time for such training. When asked whether they would be interested in participating in a training workshop in basic resuscitation techniques outside working/academic hours, 64.3% replied affirmatively, while 11.1% replied no. The rest were undecided.
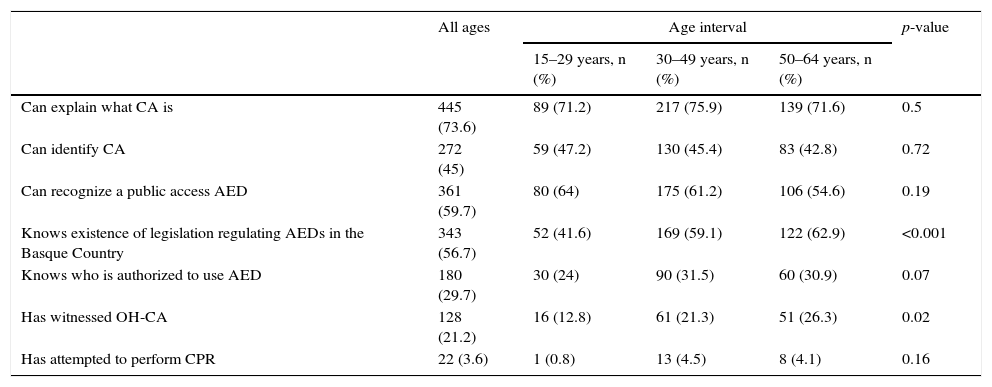
General knowledge of cardiac arrest and semiautomated external defibrillationA total of 73.6% of the responders claimed to know the meaning of cardiac arrest, though only 45% felt that they could identify CA if they were to witness the event. In turn, 59.7% would be able to identify a public access AED, and 43.3% were unaware of the existence of regulations on the use of such devices in the Basque Country (such unawareness being greater among young individuals between 15–29 years of age). Only 29.8% knew that citizens are legally authorized to use such devices in the event of an emergency.
A total of 21.2% of our study sample claimed to have witnessed OH-CA at some point in life, and 3.6% reported having attempted CPR maneuvering before arrival of the medical emergency service.
Table 2 shows the general knowledge of the study population, establishing comparisons by age groups. Notorious homogeneity of knowledge was evidenced in all three age intervals.
General knowledge of cardiac arrest and automated external defibrillators according to age intervals.
| All ages | Age interval | p-value | |||
|---|---|---|---|---|---|
| 15–29 years, n (%) | 30–49 years, n (%) | 50–64 years, n (%) | |||
| Can explain what CA is | 445 (73.6) | 89 (71.2) | 217 (75.9) | 139 (71.6) | 0.5 |
| Can identify CA | 272 (45) | 59 (47.2) | 130 (45.4) | 83 (42.8) | 0.72 |
| Can recognize a public access AED | 361 (59.7) | 80 (64) | 175 (61.2) | 106 (54.6) | 0.19 |
| Knows existence of legislation regulating AEDs in the Basque Country | 343 (56.7) | 52 (41.6) | 169 (59.1) | 122 (62.9) | <0.001 |
| Knows who is authorized to use AED | 180 (29.7) | 30 (24) | 90 (31.5) | 60 (30.9) | 0.07 |
| Has witnessed OH-CA | 128 (21.2) | 16 (12.8) | 61 (21.3) | 51 (26.3) | 0.02 |
| Has attempted to perform CPR | 22 (3.6) | 1 (0.8) | 13 (4.5) | 8 (4.1) | 0.16 |
AED: automated external defibrillator; OH-CA: out-of-hospital cardiac arrest; CPR: cardiopulmonary resuscitation.
A great majority of the responders considered it “very important” or “quite important” for the general population to be able to identify CA and to start resuscitation maneuvering (94.7%), as well as to operate an AED (88.6%).
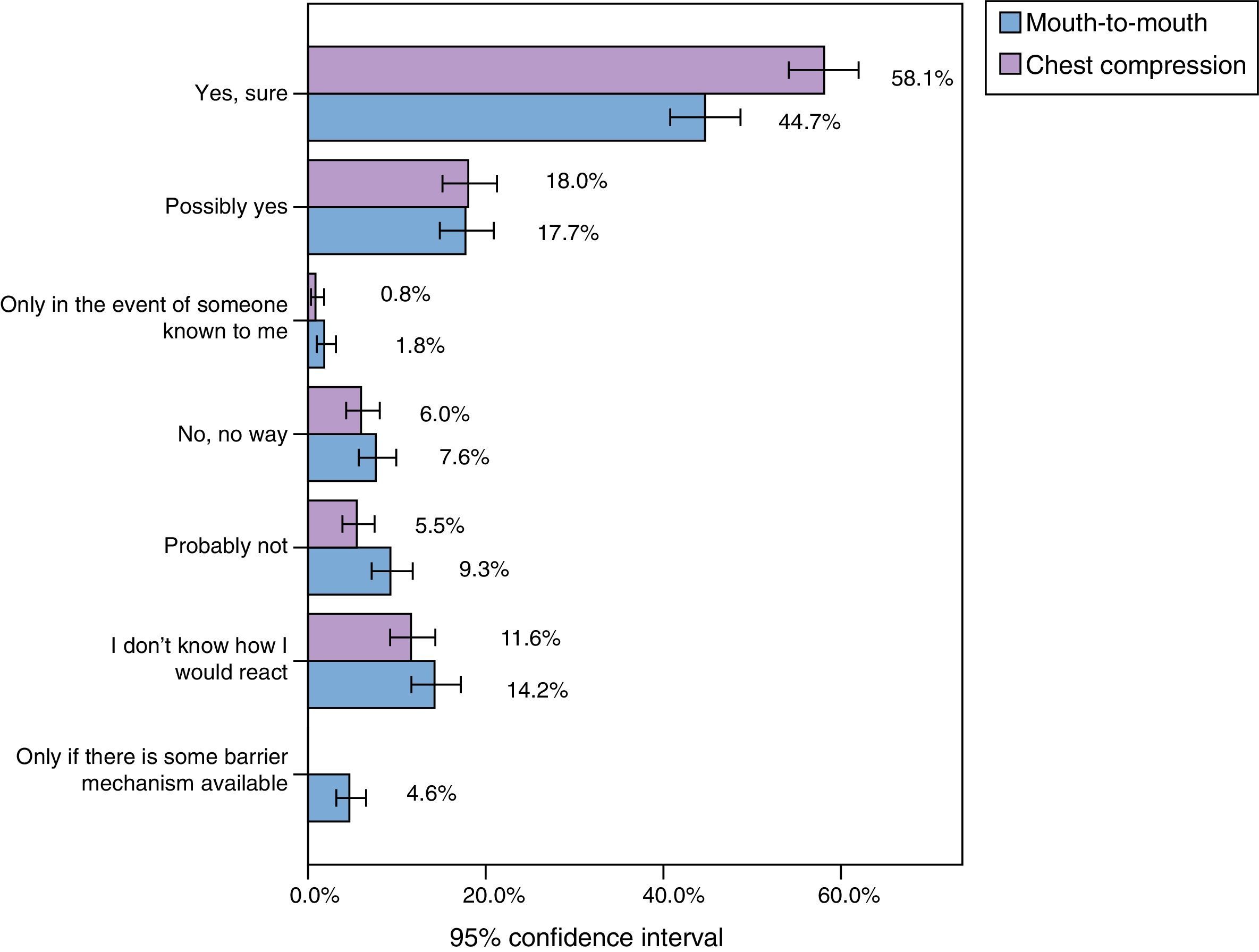
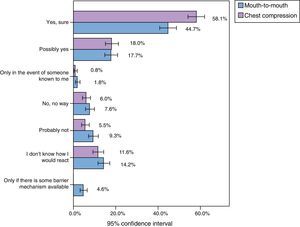
In the hypothetical event of witnessing OH-CA and having to apply basic CPR maneuvers (guided by the instructions that come with the AED or by telephone from the emergency service), 58.1% and the 44.7% of the responders claimed to be willing to perform chest compressions and mouth-to-mouth ventilation, respectively (Fig. 3).
Attitudes referred to willingness to perform chest compression and mouth-to-mouth ventilation in situations of witnessed cardiac arrest upon personal initiative, under telephone guidance from the emergency service, or following the instructions that come with the automated external defibrillator (n=604).
Sudden cardiac death is one of the main causes of death in industrialized countries. Training in CPR is therefore crucial. It has been estimated that optimization and generalization of basic CPR maneuvering in the general population could save about 8000 lives each year in Spain,14 and since ventricular tachyarrhythmia is a frequent cause of CA and defibrillation is currently the only effective way to revert the condition, there is an undeniable need to improve the systems for public access to AEDs, as well as to standardize explicit authorization for non-medical personnel to use such devices–thereby obviating the barriers facing their implementation or use.9
For this reason, and in an attempt to reinforce the third link in the chain of survival, the Basque Government has decided to authorize all citizens to use AEDs–in contrast to the situation found in most Spanish Autonomous Communities, where authorization to use AEDs is limited to medical personnel or people who have completed a specific training program.7 However, in this study it is seen that although the majority of the Basque population appears to understand that acquiring skills for correctly dealing with CA is important, only a small percentage have received specific training in resuscitation maneuvering. Barely 60% of the people in our study considered themselves able to correctly identify a public access AED, and only 30% were aware that all people are legally authorized to use the device in the event of OH-CA. These observations may suggest that efforts have focused more on legislating than on enhancing awareness among the general population of the need to know the first steps to be taken in the case of a person suffering cardiac arrest.
With regard to this latter aspect, it has been postulated that the inclusion of first-aid training in school could represent a great step forward not only in teaching but also in consolidating skills in dealing with health emergencies.15 In fact, countries such as the United States,4 Japan5,16 or Sweden17 have developed public access AED programs, with large-scale educational efforts in resuscitation techniques targeted to the general population, that have resulted in an increase in the survival rates following OH-CA.
In the case of the Basque Country, and in concordance with the observations in other regions,18 the lack of knowledge of the population in these issues appears to be a consequence of difficulties in accessing the training offers and the scant interest they raise–though over 40% of the people without training expressed interest in participating in some workshop in this area. On the other hand, it is a matter of concern that most of those who claimed to have received training received it several years ago. In effect, a period of several years is too long, considering that rehabilitation skills quickly deteriorate,19 in the same way as the capacity to react in the event of witnessing CA.20 This circumstance explains the discrepancy observed in our study between the responders who had received training in CPR or AED techniques (37%) and the proportion of people who at the time of the interview really felt capable of applying such techniques (20.2%).
The regular conduction of population-based surveys could be useful for assessing the development of community training programs and for monitoring changes in trends referred to skills in CPR and the use of AED. To our knowledge, ours is the third study to date in addressing knowledge and attitudes toward CPR in the Spanish population. In 2010, upon the initiative of the Spanish Council of Cardiopulmonary Resuscitation, a telephone survey was made of 1001 citizens over 18 years of age from all over the country, with the purpose of exploring their knowledge of CA and resuscitation maneuvers.21 Posteriorly, in 2014, during the International Congress of the European Resuscitation Council in Bilbao (Spain), del Pozo-Vegas et al. presented the results of a survey involving a convenience sample of 340 individuals visiting the emergency care service, in which their knowledge and training in applying resuscitation measures was analyzed.22 In our study we observed similarities as well as differences with respect to the previous surveys. For example, in all three studies, approximately two-thirds of those interviewed recognized an AED, but the proportion of people who claimed to know how to perform CPR ranged from 20.2% in our study to 33% in the survey of the Spanish Council of Cardiopulmonary Resuscitation. Likewise, the number of citizens who claimed to have performed CPR at some time in the past varied from 3.6% in the Basque Country to 11.5% in the study published by del Pozo-Vegas et al. These discrepancies are possibly attributable to methodological differences in the sampling systems used in each study, and do not necessarily reflect trends inherent to each region.
At international level we again find relatively few studies referred to knowledge of CPR among the general population, and most publications focus on the training received–not on self-perception or the evaluation of skills. Of note is the fact that the results of the different surveys show great discrepancies depending on the geographical setting involved. Thus, in New Zealand it has been estimated that 26% of the population has received training in resuscitation techniques,23 versus 31% in Singapore24 and 79% in King County, Washington (USA).25 The data referred to the Basque Country fall short of those published in other European countries such as Slovenia,26 where almost 70% of the population has received training in CPR, or Sweden,27 where the figure is 45%. Since the population of the Basque Country largely views universal training in CPR as important, and considering that the attitudes toward CPR maneuvering guided by telephone or by the instructions that come with the AED are favorable, it would be reasonable to assume that basic training programs for citizens on how to act in the event of CA would be well accepted and followed.
LimitationsThe main limitation of our study is the measurement instrument used. Due to the lack of a standardized and validated questionnaire, an instrument had to be developed ad hoc for the study–a fact that complicated comparisons with other surveys evaluating the same objectives as in our study. Furthermore, feasibility reasons caused us to only consider self-perception of some of the explored knowledge and skills, without being able to assess the suitability or the quality of the steps and techniques used in dealing with CA.
Another limitation of the study is the sampling system used. In view of the important methodological bias affecting telephone surveys as a data collection tool,28 we chose to collect information directly by means of trained interviewers. However, despite the efforts made to obtain a representative sample of each age interval and maintain the proportions of the original population, the sampling points were restricted to provincial capitals. As a result, extrapolation of the results obtained to suburban or rural areas must be made with caution.
On the other hand, the study did not assess individuals under 16 or over 64 years of age, since we felt that the peculiarities of these population groups (maturity, physical capacity, greater functional differences between close-lying ages, etc.) could require a more specific analysis. Furthermore, assuming that resuscitation skills are a competence extendable across all healthcare professions, we likewise excluded people with medical studies or professionally linked to the emergency care setting–though in this regard some investigations have alerted to the existence of training shortcomings in this population group.29,30
Lastly, and in relation to the data collection system used, the possibility of acquiescence bias must be mentioned, reflecting the desire of some responders to offer answers that are pleasant or agreeable to the person conducting the interview or to society. However, an interesting result in our study is the fact that the proportion of responders who claimed to feel capable of applying life support measures (20.2%) was very close to the proportion of OH-CA episodes in which the witnesses of the event performed some resuscitation attempt before the arrival of the first medical team (22.9%).1
Our data show that although there is a generalized perception that citizens should have enough knowledge to identify CA and immediately start basic resuscitation maneuvers, the levels of training, self-perceived capacitation and knowledge among the population of the Basque Country in relation to CPR and AED are very limited. Although important steps have been taken in the Basque Country to improve accessibility to AEDs, educational strategies are needed to optimize the first links in the chain of survival.
Financial supportThis study has received no external financial support.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ballesteros-Peña S, Fernández-Aedo I, Pérez-Urdiales I, García-Azpiazu Z, Unanue-Arza S. Conocimientos y actitudes de los ciudadanos del País Vasco sobre la resucitación cardiopulmonar y los desfibriladores externos automatizados. Med Intensiva. 2016;40:75–83.