Kounis syndrome (KS) or allergic infarction was first described back in 1991 as the simultaneous appearance of an acute coronary syndrome (ACS) and an anaphylactic allergic reaction. Its incidence is still unknown, since most data come from small series of cases.1–10 When it comes to its etiology, multiple trigger factors have been described such as drugs or food.3
We conducted one retrospective study including all patients admitted to our hospital Intensive Care Unit (including both the Polyvalent Intensive Care Unit and the Coronary Unit) due to anaphylactic reactions from 2007 through 2015 (a total of 11,780 admissions). This study was approved by our center research ethics committee. The goal was to know the incidence, characteristics, management and progression of the KS.
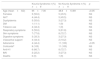
Twenty (20) patients were included, of which nine (9) (45%) suffered allergic infarctions (Table 1), which amounts to an incidence rate of six (6) cases for every 1000 admissions-year. The average age was 63 years old (range 59–77); 66.7% of the cases showed some cardiovascular risk factor, although only one (1) patient had a prior history of ACS. All cases showed ST-segment elevation: the inferior territory was the most commonly damaged territory followed by the anterior territory or by simultaneous damage to both territories. None of the patients of our series was treated with thrombolysis; 77% of the patients showed elevated markers of myocardial damage (high-sensitive cardiac troponin T [normal hs-cTnT 0–14pg/mL] and creatine phosphokinase [normal CK 26–140UI/L]), yet the hs-cTnT was significantly higher (mean 133, range 10–567) than the CK (mean 96, range 35–859). Only two (2) patients (cases 7 and 9) showed ventricular dysfunction, one of them in the context of the Tako-Tsubo syndrome, but somehow unrelated to the acute coronary occlusion that was also present in two (2) cases. In the cases with ventricular dysfunction, such dysfunction resolved during follow-up. During the average follow-up of 39.7±28.6 months no deaths were reported or major cardiovascular events.
Characteristics of patients with Kounis syndrome.
| Case#1 | Case#2 | Case#3 | Case#4 | Case#5 | Case#6 | Case#7 | Case#8 | Case#9 | |
|---|---|---|---|---|---|---|---|---|---|
| Age | 63 | 59 | 58 | 77 | 64 | 73 | 73 | 59 | 59 |
| Sex | Female | Male | Female | Male | Male | Female | Female | Female | Male |
| AHT | Yes | No | No | Yes | No | No | Yes | No | Yes |
| DM | No | No | No | No | No | No | Yes | No | No |
| Dyslipidemia | No | No | No | Yes | Yes | Yes | Yes | No | Yes |
| Tobacco use | No | Yes | No | Yes | Yes | Yes | No | No | No |
| Noxa | Unknown | Paracetamol | Anesthesiaa | Amoxicillin -clavulanic acid | Anesthesiaa | Sonovue | Metamizol | Anesthesiaa | Amoxicillin |
| ST-elevation | Inferior | Anterior | Inferior+anterior | Inferior | Inferior | Inferior | Anterior | Inferior | Inferior+anterior |
| hs-cTnT peak (pg/mL) | 12 | 489 | 10 | 39 | 133 | 528 | 567 | 79 | 327 |
| CK peak (IU/L) | 35 | 298 | 42 | 96 | 155 | 90 | 205 | 60 | 859 |
| LVEFb in % | 65 | 62 | 58 | 75 | 68 | 60 | 45 | 70 | 30 |
| Segmental alterations | No | Distal lateral and apical | No | Inferior and distal inferior-lateral | No | Inferior and basal inferior-lateral | Apex | No | Generalized |
| Coronariography | Normal | Distal ADA occlusion | Normal | Normal | Normal | Stent thrombosis in RCA | Normal | Not performed | Normal |
| Antiplatelet therapy | ASA and clopidogrel | ASA and clopidogrel | ASA and clopidogrel | ASA and clopidogrel | ASA and clopidogrel | ASA and clopidogrel | A ASA and clopidogrel | ASA | ASA and clopidogrel |
| Nitroglycerine | No | No | No | Yes | No | Yes | No | No | No |
| Vasoactive support | No | No | Yes | No | Yes | No | No | Yes | Yes |
| Adrenaline | No | Yes | Yes | No | No | No | No | Yes | Yes |
| Corticoids | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Anti-H1 | Yes | Yes | Yes | No | Yes | No | Yes | No | Yes |
| IMV | No | Yes | No | No | No | No | No | No | Yes |
| Death or MACE | No | No | No | No | No | No | No | No | No |
ASA: acetylsalicylic acid; RCA: right coronary artery; CK: creatine phosphokinase (normalcy range 26–140IU/L); ADA: anterior descending artery; DM: diabetes mellitus; MACE: major adverse cardiac events (acute myocardial infarction, heart failure, or stroke); LVEF: left ventricle ejection fraction; AHT: arterial hypertension; hs-cTnT: high-sensitive cardiac troponin T (normalcy range 0–14pg/mL); IMV: invasive mechanical ventilation.
Using the Student's t-test for mean-comparison or the χ2-test for proportion-comparison and yet despite the limitation due to the number of patients and after checking the adjustment of a normal distribution using the Kolmogorov–Smirnov's test, one comparative analysis was conducted with the anaphylactic reaction without allergic infarction. There were no statistically significant differences except for age: the youngest patients were those without KS and on treatment with adrenaline, that was most commonly used in the latter (Table 2).
Comparison of the characteristics of patients with anaphylactic reactions associated, or not, to Kounis Syndrome.
| Kounis Syndrome n (%) n=9 | No Kounis Syndrome n (%) n=11 | p | |
|---|---|---|---|
| Age (mean±SD) | 65±7.36 | 48.8±13.89 | <0.05 |
| Females | 5 (55.6) | 5 (45.5) | NS |
| AHT | 4 (44.4) | 5 (45.5) | NS |
| Dyslipidemia | 5 (55.6) | 3 (27.3) | NS |
| DM | 1 (11.1) | 1 (9) | NS |
| Tobacco use | 4 (44.4) | 1 (9) | NS |
| Respiratory symptoms | 5 (55.6) | 9 (81.8) | NS |
| Skin symptoms | 7 (77.8) | 8 (72.7) | NS |
| Digestive symptoms | 3 (33.3) | 3 (27.3) | NS |
| Vasoactive support | 4 (44.4) | 2 (18.2) | NS |
| Adrenaline | 4 (44.4) | 11 (100) | <0.05 |
| Corticoidsa | 9 (100) | 11 (100) | NS |
| Anti-H1 | 6 (66.7) | 8 (72.7) | NS |
| IMV | 2 (22.2) | 3 (27.3) | NS |
| Deaths | 0 (0) | 1 (9) | NS |
Anti-H1: antihistamines H1; SD: standard deviation; DM: diabetes mellitus; AHT: arterial hypertension; NS: non-significant (p≥0.05); IMV: invasive mechanical ventilation.
The sudden onset of thoracic pain followed by allergic symptoms should be suspicious of KS and, in our series, a considerable number of patients with anaphylactic shock who were admitted to the ICU showed clinical manifestations compatible with an allergic infarction.
There are three (3) types of KS that appear in our series. Type I occurs in patients without coronary disease and the most likely mechanism is vasospastic disorder or microvascular damage.2 In type II there is preexisting atheromatous disease and erosion, or acute tear of the plaque induced by the release of mediators of anaphylaxis.1–6 The last one, type III, is described as somehow related to the thrombosis of a stent previously implanted.5
As it occurs in our series, the ECG usually shows the ST-segment elevation in inferior and anterior leads2,8 and it is essential not only for its diagnosis, but also to establish a cause-effect correlation with the possible trigger factor. Added to the usual lab conclusions of ACS, an immune-allergic study should be conducted here3 including tryptase, histamine, complement, eosinophils and IgE.2,7,8
When it comes to management, we should say that the specific therapies accepted for the management of ACS and anaphylaxis can have contraindications too.8
When it comes to the management of ACS, acetylsalicylic acid and beta-blockers could aggravate anaphylaxis. The calcium channel blockers are the first line anti-ischemic therapy, although nitroglycerine may be considered in patients who are not hypotense.4,6,7 In our series, no patient was ever treated with beta-blockers or calcium antagonists and two (2) cases were treated with nitroglycerine. For pain relief purposes, the use of fentanyl is preferred over morphine, that is capable of promoting mastocyte degranulation.2
Although adrenaline is the therapy of choice for the management of anaphylaxis, in the ACS it can aggravate ischemia and induce vasospasms and arrhythmias.7 Thus, in the management of KS (particularly types II and III) the risks may overcome the benefits, which is why it is necessary to conduct targeted studies to be able to make recommendations on this regard.1 Although corticoids can slow down the myocardial wall scar formation process, no data dissuade us from using them,1,6 being the simultaneous use of H1 (dexchlorpheniramine or diphenhydramine) and H2 (ranitidine) antagonists recommended.4,8
Up to 40% of intravascular volume moves into the interstitium, meaning that volume expansion may be necessary, which should be performed through hemodynamic monitoring and evaluation of the ventricular function in order to avoid developing congestion.6,7
Today there are no established clinical guidelines for the management of KS and the number of cases is too small to be able to draw definitive conclusions on this regard. In sum, an initial approach should first evaluate whether, in the clinical manifestations, the anaphylactic reaction with associated skin or respiratory damage (so that the use of adrenaline is not delayed) or the ACS with persistent thoracic pain is predominant (for which we will prioritize the use of calcium antagonists). Secondly, and preferably with known coronary anatomy and based on the type of KS, the presence of coronary occlusion and revascularization should be assessed here, as well as the existence and extension of myocardial necrosis and, finally, in a risk/benefit ratio, we will associate corticoids, volume, or antiplatelet therapy.
There are still many doubts on this rare and underdiagnosed entity2: we need to study more cases before we can solve these doubts and understand the links with other entities such as the Tako-Tsubo syndrome.2,10
Please cite this article as: Barrionuevo Sánchez MI, Corbí Pascual MJ, Córdoba Soriano JG, Ramírez Guijarro C, Calero Nuñez S, Gallego Sánchez G. Síndrome de Kounis o infarto alérgico: una entidad desconocida. Med Intensiva. 2018;42:506–509.