The purpose of this study was to determine the late complications in critically ill patients requiring percutaneous tracheostomy (PT) using the balloon dilation technique.
DesignA prospective, observational cohort study was carried out.
ScopeTwo medical-surgical intensive care units (ICU).
PatientsAll mechanically ventilated adult patients consecutively admitted to the ICU with an indication of tracheostomy.
InterventionsAll patients underwent PT according to the Ciaglia Blue Dolphin® method, with endoscopic guidance. Survivors were interviewed and evaluated by fiberoptic laryngotracheoscopy and tracheal computed tomography at least 6 months after decannulation.
VariablesIntraoperative, postoperative and long-term complications and mortality (in-ICU, in-hospital) were recorded.
ResultsA total of 114 patients were included. The most frequent perioperative complication was minor bleeding (n=20) and difficult cannula insertion (n=19). Two patients had severe perioperative complications (1.7%) (major bleeding and inability to complete de procedure in one case and false passage and desaturation in the other). All survivors (n=52) were evaluated 211±28 days after decannulation. None of the patients had symptoms. Fiberoptic laryngotracheoscopy and computed tomography showed severe tracheal stenosis (>50%) in 2 patients (3.7%), both with a cannulation period of over 100 days.
ConclusionsPercutaneous tracheostomy using the Ciaglia Blue Dolphin® technique with an endoscopic guide is a safe procedure. Severe tracheal stenosis is a late complication which although infrequent, must be taken into account due to its lack of clinical expressiveness. Evaluation should be considered in those tracheostomized critical patients who have been cannulated for a long time.
Analizar las complicaciones a largo plazo de los pacientes críticos que requirieron traqueotomía percutánea (TP) con el método de dilatación con balón.
DiseñoEstudio observacional, prospectivo, de cohorte.
ÁmbitoDos unidades de cuidados intensivos (UCI) polivalentes.
PacientesAdultos ventilados mecánicamente ingresados en UCI con indicación de TP.
IntervenciónEn todos los pacientes se realizó TP mediante Ciaglia Blue Dolphin® con guía endoscópica. Los pacientes decanulados vivos fueron evaluados clínicamente, así como mediante laringotraqueoscopia y tomografía axial computarizada cervical al cabo de al menos 6 meses tras la decanulación.
VariablesComplicaciones intraoperatorias, postoperatorias y tardías. Mortalidad intra-UCI y hospitalaria.
ResultadosSe incluyeron 114 pacientes. Las complicaciones intraoperatorias más frecuentes fueron la hemorragia leve (n = 20) y la dificultad para insertar la cánula (n = 19). Dos pacientes tuvieron complicaciones intraoperatorias graves (1,7%) (hemorragia e imposibilidad de finalización de la técnica, en un caso, y falsa vía y desaturación, en otro). Todos los pacientes decanulados vivos (n = 52) fueron revisados a los 221 ± 28 días tras la decanulación. Ningún paciente presentaba síntomas. La tomografía axial computarizada y la laringotraqueoscopia mostraron estenosis traqueal severa (>50%) en 2 pacientes (3,7%), ambos con periodos de canulación superiores a 100 días.
ConclusionesLa TP usando la técnica Ciaglia Blue Dolphin® con guía endoscópica es un procedimiento seguro. La estenosis traqueal grave es una complicación tardía que, aunque infrecuente, debe ser tenida en cuenta por su falta de expresividad clínica. Debería considerarse la evaluación de aquellos pacientes críticos que han sido traqueotomizados y han permanecido canulados durante periodos prolongados de tiempo.
Ever since 1985, the percutaneous tracheotomy (PT) procedure has become more and more popular in Intensive Care Units (ICU) because it is easy to execute, because the intensivist can use it at the patient's bedside, and because it has a low rate of serious complications. Recently, the first evidence-based clinical guidelines for the use of tracheotomy procedures in critically ill patients have been published; they happen to be the only internationally agreed comprehensive guidelines today.1
Yet despite the fact that the PT procedure has been widely used and the medical literature is extensive on this regard, neither the prevalence nor the impact of its long-term complications have been studied. The difficulty inherent to the follow-up of critically ill patients who have been tracheostomized has led to very few studies and scarce samples.2–4 The goal of this study has been to analyze the late complications of patients operated through PT procedures using the balloon dilation technique (Ciaglia Blue Dolphin® [CBD]) through one follow-up protocol consisting of clinical examination; laryngotracheoscopy (LT) and computerized axial tomography (CAT) scan of the cervical spine.
Patients and methodProspective, observational cohort study conducted in two (2) medical-surgical ICUs.
Between September 2011 and May 2014, the data from all patients tracheostomized using the CBD technique was recorded. Back in 2013 one intermediate analysis was conducted in order to assess the early complications of the first 70 PT procedures whose results were published in this medical journal.5 In this work, the surgical technique, the inclusion and exclusion criteria, and all the in- and postoperative complications are described. In the actual work, the intraoperative complications of the overall sample studied are shown, together with one long-term assessment (that did not happen during the preliminary analysis) of patients tracheostomized using the CBD method.
The patients were evaluated six (6) months after the decannulation. The assessment consisted of: (1) Clinical examination to assess the presence of pain in the area of the prior PT procedure, dyspnea, cough, voice changes, and difficulties releasing secretions. The patient scored the esthetic result of his surgical scar in a scale ranging from bad, to regular, good, and very good. (2) Assessment by one ENT (ear, nose, throat) specialist who conducted the flexible LT in order to check the vocal cords motility, the resulting stromal crust, and any other possible complications associated with the former PT procedure. (3) Radiologic examination through a CAT scan of the cervical spinal (0.6mm slices). 3D sagittal, coronal reconstructions, and virtual endoscopies were conducted. When in the presence of tracheal stenosis, both during the ENT and the radiological assessment, the location, cause, and gradation were registered using the following ranges: (a) mild stenosis – obstructions <10%; (b) moderate stenosis – obstructions between 10% and 50%, and (c) severe stenosis – obstructions >50% of the tracheal lumen.
The study was approved by the ethics committee from each hospital. Prior written informed consent from the patients or their legal representatives was needed to participate in the study.
StatisticsThe data was analyzed using the statistical software Statistical Product and Service Solution (SPSS) version 19. The results of the quantitative variables were expressed as averages and standard deviations when they followed a normal distribution curve assessed using the Kolmogorov–Smirnoff test. The ones that did not follow a normal distribution were expressed as means and ranges. The quantitative data was expressed as absolute values (n) and percentages. The comparison among the different quantitative variables was conducted using Student t test or the Mann–Whitney test and based on the behavior of the variables analyzed. The Chi-square test was used to show the differences among all the qualitative variables. P values <0.05 were considered statistically significant.
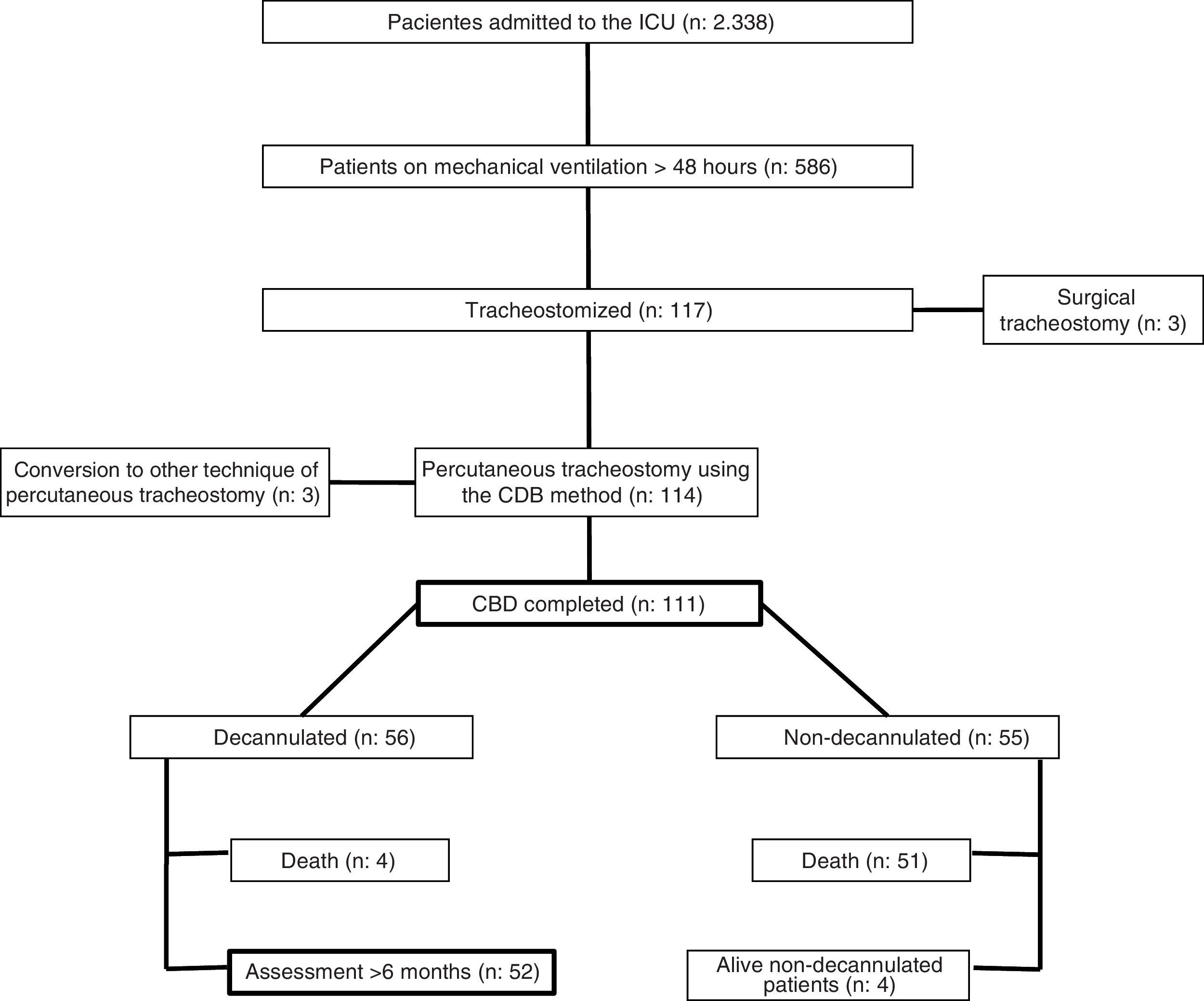
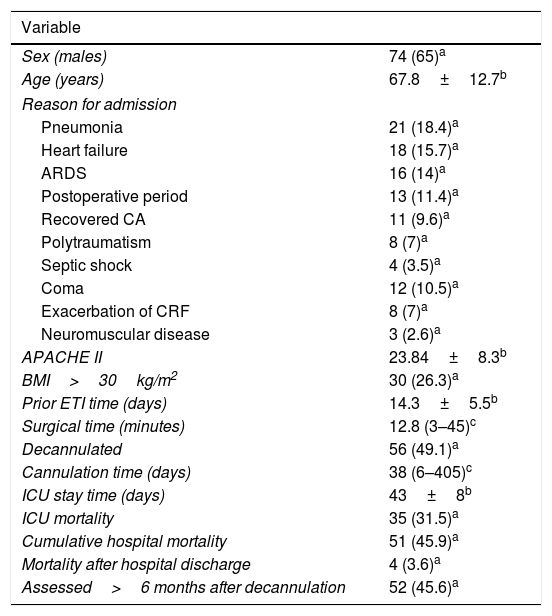
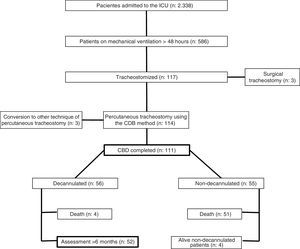
ResultsA total of 117 patients were tracheostomized, that is, 20% of the patients ventilated>48h (n=586). Three (3) patients were excluded due to contraindication to undergo PT procedures (two patients due to anatomical distorsion with impossibility of locating the structures, and one patient due to prior PT procedure), so, eventually, 114 patients underwent PTs using the CBD method. The epidemiological data is shown in Table 1.
Epidemiological data.
| Variable | |
|---|---|
| Sex (males) | 74 (65)a |
| Age (years) | 67.8±12.7b |
| Reason for admission | |
| Pneumonia | 21 (18.4)a |
| Heart failure | 18 (15.7)a |
| ARDS | 16 (14)a |
| Postoperative period | 13 (11.4)a |
| Recovered CA | 11 (9.6)a |
| Polytraumatism | 8 (7)a |
| Septic shock | 4 (3.5)a |
| Coma | 12 (10.5)a |
| Exacerbation of CRF | 8 (7)a |
| Neuromuscular disease | 3 (2.6)a |
| APACHE II | 23.84±8.3b |
| BMI>30kg/m2 | 30 (26.3)a |
| Prior ETI time (days) | 14.3±5.5b |
| Surgical time (minutes) | 12.8 (3–45)c |
| Decannulated | 56 (49.1)a |
| Cannulation time (days) | 38 (6–405)c |
| ICU stay time (days) | 43±8b |
| ICU mortality | 35 (31.5)a |
| Cumulative hospital mortality | 51 (45.9)a |
| Mortality after hospital discharge | 4 (3.6)a |
| Assessed>6 months after decannulation | 52 (45.6)a |
No.=114 patients included for percutaneous tracheostomy procedure using the balloon dilation technique.
BMI: body mass index; CRF: chronic respiratory failure; CA: cardiac arrest; ARDS: acute respiratory distress syndrome; Prior ETI time: endotracheal intubation time prior to the tracheostomy.
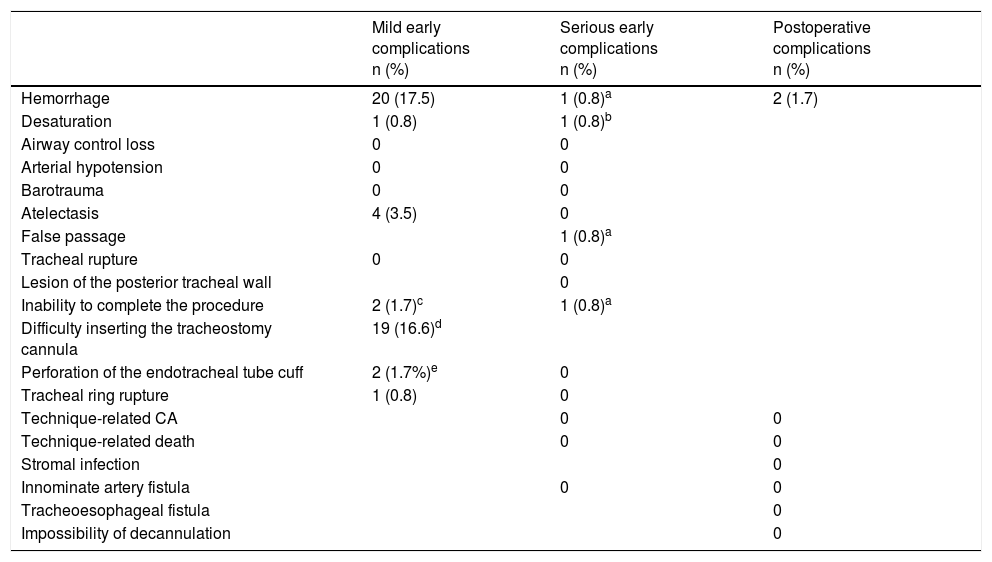
Intraoperative and postoperative complications are shown in Table 2. In three (3) patients (2.6%) it was impossible to complete the procedure using the CBD method, and another PT modality had to be used. These three (3) patients were excluded from the subsequent follow-up. Out of the 111 PTs completed using the CBD method, 51 patients (44.7%) died in the hospital while cannulated (35 in the ICU) due to underlying conditions. The main reasons for admission for the deceased patients (n=51) were: urgent postoperative period (19.6%), cardiac arrest reversal (17.6%), and pneumonia (15.6%). Thirty-six (36) patients were men. The average age was 72±18 years and the APACHE II score was 24.7±8.6. The cannulation time was 17.9 days [r: 3–75].
Perioperative and postoperative complications (n=114).
| Mild early complications n (%) | Serious early complications n (%) | Postoperative complications n (%) | |
|---|---|---|---|
| Hemorrhage | 20 (17.5) | 1 (0.8)a | 2 (1.7) |
| Desaturation | 1 (0.8) | 1 (0.8)b | |
| Airway control loss | 0 | 0 | |
| Arterial hypotension | 0 | 0 | |
| Barotrauma | 0 | 0 | |
| Atelectasis | 4 (3.5) | 0 | |
| False passage | 1 (0.8)a | ||
| Tracheal rupture | 0 | 0 | |
| Lesion of the posterior tracheal wall | 0 | ||
| Inability to complete the procedure | 2 (1.7)c | 1 (0.8)a | |
| Difficulty inserting the tracheostomy cannula | 19 (16.6)d | ||
| Perforation of the endotracheal tube cuff | 2 (1.7%)e | 0 | |
| Tracheal ring rupture | 1 (0.8) | 0 | |
| Technique-related CA | 0 | 0 | |
| Technique-related death | 0 | 0 | |
| Stromal infection | 0 | ||
| Innominate artery fistula | 0 | 0 | |
| Tracheoesophageal fistula | 0 | ||
| Impossibility of decannulation | 0 |
The shadowed cells in the columns of the perioperative complications correspond to complications that are not considered mild or severe. In the case of postoperative complications, they are not considered as such.
CA: cardiac arrest.
Four (4) patients (3.5%) were transferred with the cannula in situ to long-stay hospitals due to the impossibility of decannulating them and, in all of them, the possibility of complications following the PT procedure was ruled out (two patients developed polyneuropathy of the critically ill patient and could not be disconnected from the mechanical ventilation machine, one patient had ventilator-dependent amyotrophic lateral sclerosis, and one patient had sequelae following a severe brain traumatic brain injury that required the aspiration of bronchial secretions). A total of 56 patients (49.1%) were successfully decannulated, but four (4) of them died after being discharged from the hospital (during the study period) for medical causes unrelated to the technique used. A total of 52 patients were included in the analysis of late complications (Fig. 1).
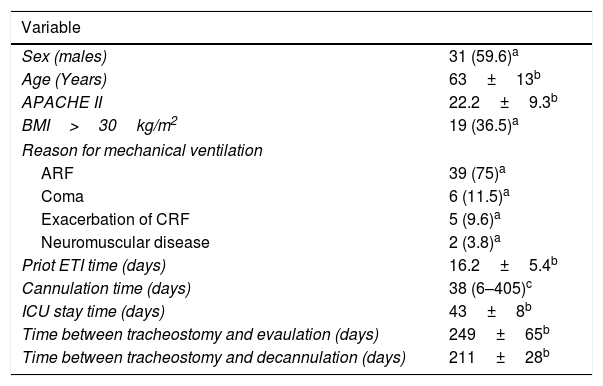
They all agreed to the evaluation included in the protocol (questionnaire, LT and CAT); evaluation that was completed in each and every patient. The demographic data of these 52 patients is shown on Table 3. The average cannulation time was 38 days (r: 6–405). Ten (10) patients (17.8%) were cannulated for more than 30 days. During the cannulation period, two (2) patients (2.6%) showed mild hemorrhages through the edges of the stroma without any other postoperative complications. The average time elapsed from the decannulation up until the evaluation was 211±28 days.
Epidemiological data of patients under long-term assessment (n=52).
| Variable | |
|---|---|
| Sex (males) | 31 (59.6)a |
| Age (Years) | 63±13b |
| APACHE II | 22.2±9.3b |
| BMI>30kg/m2 | 19 (36.5)a |
| Reason for mechanical ventilation | |
| ARF | 39 (75)a |
| Coma | 6 (11.5)a |
| Exacerbation of CRF | 5 (9.6)a |
| Neuromuscular disease | 2 (3.8)a |
| Priot ETI time (days) | 16.2±5.4b |
| Cannulation time (days) | 38 (6–405)c |
| ICU stay time (days) | 43±8b |
| Time between tracheostomy and evaulation (days) | 249±65b |
| Time between tracheostomy and decannulation (days) | 211±28b |
Prior ETI time: endotracheal intubation time prior to the tracheostomy; BMI: body mass index; ARF: acute respiratory failure; CRF: chronic respiratory failure.
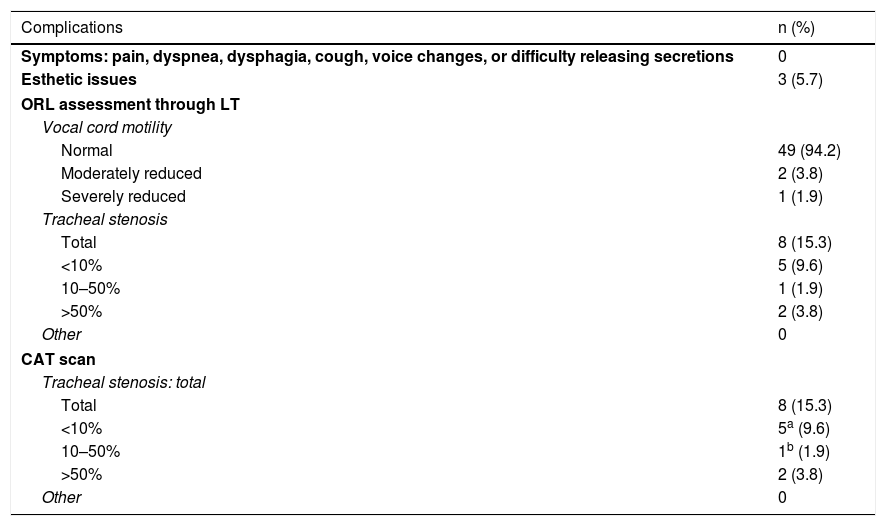
Late complications are shown in Table 4. No patient was symptomatic. The physical examination confirmed no stridor in any of the cases. Three (3) patients (2.6%) ranked the esthetic outcome as poor, but no repairing surgery was necessary in any of them.
Late complications (n=52).
| Complications | n (%) |
|---|---|
| Symptoms: pain, dyspnea, dysphagia, cough, voice changes, or difficulty releasing secretions | 0 |
| Esthetic issues | 3 (5.7) |
| ORL assessment through LT | |
| Vocal cord motility | |
| Normal | 49 (94.2) |
| Moderately reduced | 2 (3.8) |
| Severely reduced | 1 (1.9) |
| Tracheal stenosis | |
| Total | 8 (15.3) |
| <10% | 5 (9.6) |
| 10–50% | 1 (1.9) |
| >50% | 2 (3.8) |
| Other | 0 |
| CAT scan | |
| Tracheal stenosis: total | |
| Total | 8 (15.3) |
| <10% | 5a (9.6) |
| 10–50% | 1b (1.9) |
| >50% | 2 (3.8) |
| Other | 0 |
LT: laryngotracheoscopy; ORL: otorhinolaryngology.
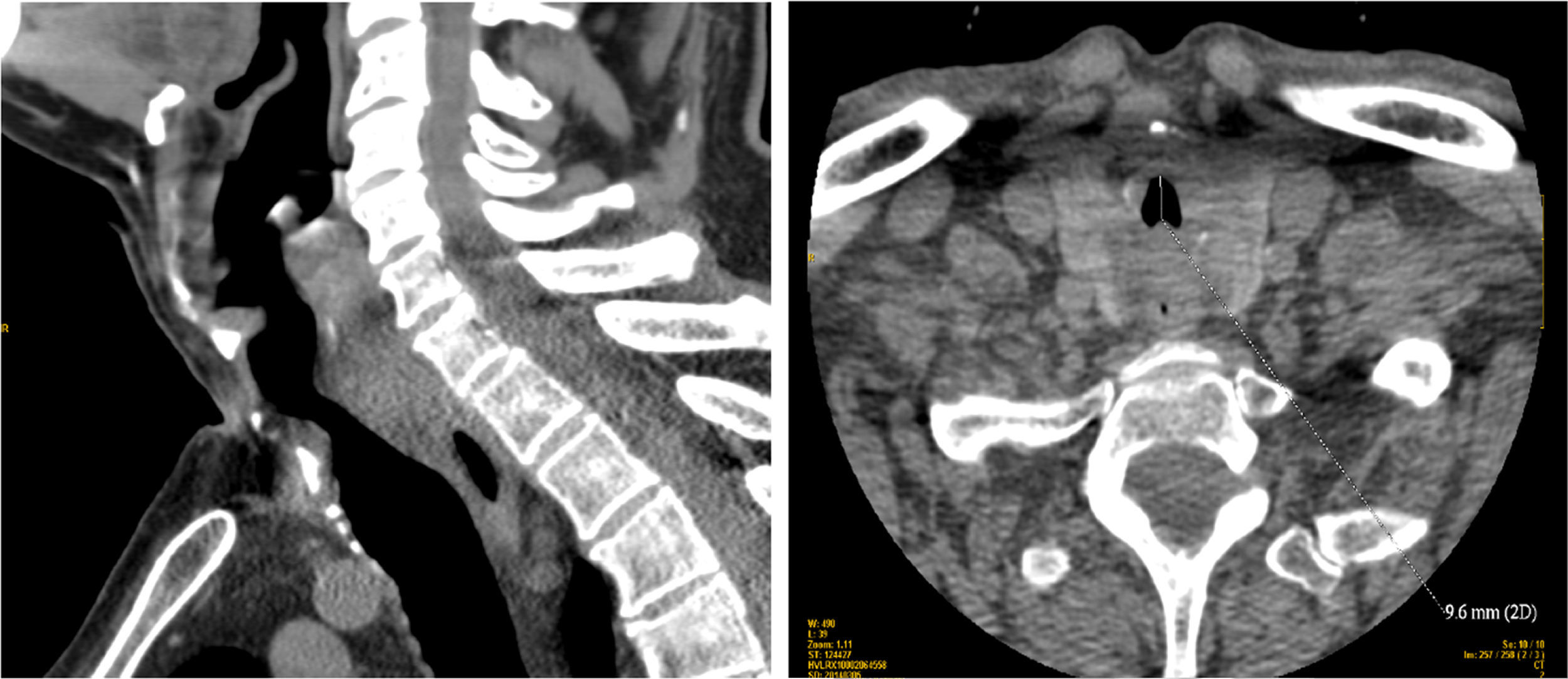
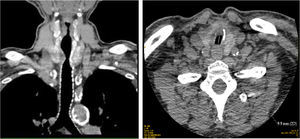
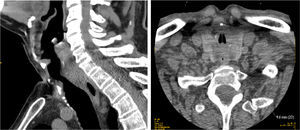
The CAT scan confirmed tracheal stenoses in eight (8) patients. In six (6) of them, it was located in the stroma (5 cases with stenoses <10%, and one case with a 25% stenosis due to tracheal ring rupture with anteroposterior displacement). In the remaining two (2) cases (3.4%) there were stenoses >50% underneath the stroma at the endotracheal tube cuff of the cannula and, in both cases, it was due to the formation of granulomas. One of these cases of severe stenosis had a 19mm-long 70% narrowing between the second and third tracheal rings, and a free tracheal diameter of 9.9mm (Fig. 2). This patient was cannulated for 138 days. The other case of severe stenosis had an 18mm-long 75% narrowing between the second and third tracheal rings, and a free tracheal diameter of 9.6mm (Fig. 3). This patient was cannulated for 128 days. Both patients had no symptoms.
The LT confirmed tracheal stenoses in the aforementioned eight (8) patients in the CAT scan (Table 4). Also, three (3) patients showed alterations in their vocal cords motility: 2 cases with unilateral palsy (one of them due to tumor infiltration in the cervical spine, and the other due to one iatrogenic lesion of the recurrent laryngeal nerve after carotid surgery), and one (1) case with bilateral palsy attributed to central origin due to meningococcal meningitis.
The tracheal stenosis was not associated with age, severity (measured using the APACHE IIscore), days of intubation prior to the PT, tracheostomies conducted during the learning period, location of the tracheal puncture site, or days of cannulation.
DiscussionThis work is the largest series published so far with an assessment of the CBD early complications, and the only one where CBD late complications have been studied. When it comes to the early complications, no more serious complications other than the ones reported in the intermediate analysis were added.5 The most common mild complications were hemorrhages and difficulties trying to insert the cannula. The latter one is a technical complication per se, and the frequency of the former one is based on how rigorous we want to be with its definition.
The protocol for the evaluation of late complications (clinical examination, LT and CAT scan) allowed us to make an analysis of the morphological and functional alterations. Thus, the late lesions of the airways found can be summarized into tracheal stenosis and vocal cord palsy. The former one is attributed to the surgical technique used, or cannula used for the tracheotomy procedure, and the latter one is attributed to underlying conditions rather than complications in the access site per se.
The actual incidence rate of late complications following PT procedures is hard to quantify. Few studies have analyzed the long-term complications and, in many cases, with short series.2–4,6–16 The characteristics of these patients make follow-up studies hard to conduct. Many critically ill patients die before being decannulated, or even before entering the study. In those who survive the disease, it may be difficult to proceed with any assessments due to the persistence of chronic medical problems, or the fact that patients do not want to be part of any studies, particularly if they are still having symptoms. Also, in the actual studies, there is a lack of consensus both on the definition of late complications and the way evaluations should be conducted. When it comes to the size of the samples, the studies with the largest samples include interviews and clinical assessments.6 In those studies where additional tests are conducted, the works where unexpensive examinations are conducted are larger,8,10,11 whereas those studies where more expensive,2,4,7,12,15 or invasive3,9,14,16 examinations are conducted have smaller samples. Only in two (2) studies, CAT scans and LTs are conducted,4,12 but in one of the studies12 none of these imaging modalities are conducted to the entire sample studied, while in the other one4 only 20 patients are studied.
Some authors say17 that if all tracheostomized patients were studied in the long term, regardless of their clinical manifestations, the incidence rate of late complications would be over 65%. Our results do not support this statement.
During the clinical assessment, all patients remained asymptomatic. The long-term symptomatology of patients operated through PT procedures are voice changes, hoarseness, and dyspnea. Most esthetic assessments were good or very good. We should remember here that a poor esthetic outcome is considered a late complication that requires surgical repair and that can happen in up to 14.1%12 of the cases. It also happens that our three (3) patients who gave negative assessments were the youngest of the series, which could have had an impact on the assessment.
The long-term complication more frequently published is tracheal stenosis. An important piece of information is that only 3–12% of them remain symptomatic.17,18 The tracheal stenosis is subclinical until the lumen does not go below 50% of its original diameter, which is when cough and difficulties clearing secretions appear; dyspnea occurs when the tracheal lumen is <10mm, and stridor when the lumen is <5mm.8
The incidence rate of tracheal stenosis found in our series (15.3%) is higher than the one published in a recent systematic review19 aimed at assessing the late complications following surgical or percutaneous tracheostomies. In that series, the prevalence of tracheal stenosis in surgical tracheostomies was 2.8%, whereas the prevalence of tracheal stenosis in percutanoues tracheostomies was between 0.6% and 1.5%. There are several reasons that may explain the difference between these results and those obtained in our sample. In the first place, the methodology of the studies included in the aforementioned systematic review may have led to a certain bias when diagnosing all late complications, since in some of the studies, only additional examinations were conducted in symptomatic patients, which is why the asymptomatic tracheal stenoses went unidentified. Secondly, the heterogeneity in the diagnosis of tracheal stenosis. In some studies, tracheal stenosis was only considered when lumen reduction was >10%,7,10,15 and in other studies when it was >50%.6 In our series, we considered tracheal stenosis even lumen reductions <10% in an attempt to better define their prevalence. Yet if we exclude stenoses <10%, the incidence rate of tracheal stenosis would drop to 5.7% and, if we only take into account stenoses >50%, the incidence rate would be 3.8%. We should also take into account here the potential issues posed by misdiagnosed tracheal stenoses, because they can be clinically relevant in patients who do vigorous work-out or even be a factor in patients who require tracheal intubation due to urgent control of their airways or scheduled surgery. On the other hand, the results from the study conducted by Karvandian et al.4 are significant since they found an 86% incidence rate of subglottic stenoses in 20 patients who underwent PT procedures using the CBD method, and were assessed using CAT scans and LTs. Although the series is scarce, these results show the highest prevalence of stenosis ever reported following PT procedures.
The tracheal stenosis following PT procedures can occur at various levels17,18,20: (1) in the stroma (due, above all, to tracheal ring ruptures, displacements of the tracheal rings, and excessive granulation tissue); (2) at the endotracheal tube cuff of the cannula (when the pressure from the tube cuff exceeds the perfusion pressure from the tracheal wall capillaries), and (3) at the distal tip of the cannula (when the tip of the cannula may damage both the anterior and posterior walls of the trachea).
The two (2) severe stenoses identified in our study were underneath stromal level. Both occurred in patients with prolonged cannulation times. Prolonged tracheal intubations prior to the PT procedure may be one confounding variable when it comes to attributing the tracheal stenosis to intubations or the PT procedure.18,20,21 The prior intubation time in the two (2) cases reported of severe stenosis was 13 and 18 days, respectively; however, the subsequent cannulation time was 138 and 128 days (the average cannulation time of the sample was 38 days), meaning that both stenoses were probably associated with prolonged cannulation times rather than endotracheal intubations.
It is not easy to establish what the term prolonged cannulation means, and all definitions are arbitrary on this regard. All patients with some degree of tracheal stenosis had been cannulated for more than 15 days, which is why we have established an assessment protocol for patients with cannulation times over 15 days. Periodic assessments of two (2) patients with severe stenosis are being conducted, and so far, none of them has required surgery.
Three (3) patients showed vocal cord palsy. These lesions are hardly attributed to the tracheostomy technique used, and in all the cases, the palsy was the result of underlying conditions.
Both the LT and the CAT scan used in our study were sensitive enough to detect tracheal stenoses. Our findings were similar with both imaging modalities, yet the follow-up using the LT provides a more dynamic view of the airway (including the vocal cords motility), is more cost-effective than the CAT scan, and, also, avoids radiation exposure. The only setback is that it is inconvenient for the patient.
One thing to remember here is that all patients alive and decannulated wanted to undergo assessments, and none of them rejected undergoing any imaging modalities, which is why the study with the 52 patients could be completed. We think that a time frame of 6 months after the cannulation is enough to see any possible complications of the laryngotracheal axis, particularly tracheal stenosis complications, since the time estimated for the occurrence of this complication is between 3 and 12 weeks.7,18
As it occurs with other studies, the main limitation of our study is that the size of the sample was small. However, we should bear in mind that it still is the largest sample ever where clinical, radiological, and LT assessments have been conducted.
In sum, the PT procedure conducted using the CBD method with ultrasound guidance is one technique with a low incidence rate of early serious complications–very similar to other PT modalities. The severe tracheal stenosis is one rare complications whose presence, although asymptomatic in many cases, should be assessed in tracheostomized patients who have remained with a cannula in situ for long periods of time. We need multicenter studies with large series of patients to give an ultimate response to what the real incidence rate is and determine what the characteristics of late complications following PT procedures in the critically ill patient really are.
Authors’ contributionJBA, JMA and AGDL contributed to the initial study idea and design. JBA, JMA, AMGF, VdP contributed recruiting patients. JBA, ME, JA, DQ, SR and AM contributed to the patients’ follow-up. JBA and JMA had access to all study data and are responsible for the integrity of the study and the accuracy of all the data analyzed. JBA and JMA contributed to the writing of this manuscript. All authors have read and approved the final version of the manuscript.
Conflict of interestThe authors declare no conflict of interests associated with this article whatsoever.
Please cite this article as: Araujo JB, Añón JM, García de Lorenzo A, García-Fernandez AM, Esparcia M, Adán J, et al. Complicaciones tardías de la traqueotomía percutánea con la modalidad de dilatación con balón. Med Intensiva. 2018;42:151–158.