Limitation of life-sustaining treatment (LLST) is a recommended practice in certain circumstances. Limitation practices are varied, and their application differs from one center to another. The present study evaluates the current situation of LLST practices in patients with prolonged admission to the ICU who suffer worsening of their condition.
DesignA prospective, observational cohort study was carried out.
SettingSeventy-five Spanish ICUs.
PatientsA total of 589 patients suffering 777 complications or adverse events with organ function impairment after day 7 of admission, during a three-month recruitment period.
Main variables of interestThe timing of limitation, the subject proposing LLST, the degree of agreement within the team, the influence of LLST upon the doctor-patient-family relationship, and the way in which LLST is implemented.
ResultsLLST was proposed in 34.3% of the patients presenting prolonged admission to the ICU with severe complications. The incidence was higher in patients with moderate to severe lung disease, cancer, immunosuppressive treatment or dependence for basic activities of daily living. LLST was finally implemented in 97% of the cases in which it was proposed. The decision within the medical team was unanimous in 87.9% of the cases. The doctor–patient–family relationship usually does not change or even improves in this situation.
ConclusionLLST in ICUs is usually carried out under unanimous decision of the medical team, is performed more frequently in patients with severe comorbidity, and usually does not have a negative impact upon the relationship with the patients and their families.
La limitación de tratamientos de soporte vital (LTSV) es una práctica recomendada en determinadas circunstancias. Las formas de limitación son variadas y su aplicación es diferente entre unos centros y otros. Conocer la situación actual de la LTSV en pacientes que presentan un ingreso prolongado en UCI y que sufren un empeoramiento es el objetivo de este trabajo.
DiseñoCohorte, observacional, prospectivo.
ÁmbitoUn total de 75 UCI españolas.
PacientesSe estudia a 589 pacientes que presentan 777 complicaciones o eventos adversos con repercusión orgánica a partir del séptimo día de ingreso, reclutados durante 3 meses.
Variables de interés principalesEstudiamos el momento en que se propone la limitación, el actor que la propone, el grado de acuerdo dentro del equipo, la influencia de este hecho en la relación médico-paciente-familia y sus formas de aplicación.
ResultadosSe plantea alguna limitación al tratamiento en el 34,3% de los pacientes con estancia prolongada en UCI que sufren complicaciones graves. La incidencia es mayor en pacientes con neumopatía moderada o grave, enfermedad oncológica, tratamientos inmunosupresores y en pacientes dependientes. En el 97% de los casos en los que se propone realizar la LTSV, finalmente se acuerda la misma. La decisión dentro del equipo médico fue unánime en el 87,9% de casos. Habitualmente la relación médico-paciente-familia no cambia o incluso mejora ante esta situación.
ConclusiónLa LTSV en las UCI es una práctica que se suele llevar a cabo con la decisión unánime del equipo médico, se realiza con más frecuencia en pacientes con comorbilidad grave y no suele deteriorar la relación con pacientes y familiares.
Intensive care units (ICUs) and life support measures with organ function replacement have contributed to prolong survival among patients with a broad range of diseases, but have also led to futile prolongation of the dying process, with an emotional and financial burden that is difficult to calculate.1,2 In 1983, Bedell et al.3 reported that although 44% of the hospitalized patients initially respond to cardiopulmonary resuscitation (CPR), only 14% are still alive at the time of discharge from hospital–this percentage in turn being far lower in individuals with certain disease conditions such as pneumonia or renal failure. The same authors found no patients with metastatic cancer, acute stroke, sepsis or pneumonia to survive following hospital admission due to cardiorespiratory arrest.4 This led Symmers5 to wonder whether the new technologies are truly able to maintain life or simply interfere with the dying process. Blackhall6 in turn suggested that physicians should apply such technologies selectively, as is still recommended today.7 Thirty-five years ago, most patients who died in the ICU were subjected to CPR.8 However, now that the limited usefulness of the indiscriminate application of CPR is known, its massive indication has given way to the limitation of therapeutic effort or the limitation of life-sustaining treatment (LLST).9
A joint document drafted by intensivists and specialists in palliative care10 has underscored that the starting point of these discussions is the recognition that life should not be needlessly prolonged in patients with incurable or end-stage disease. Severity scales or mortality predictors can be used in this respect.11 However, is it possible to predict the future with sufficient certainty to not risk depriving a patient of potential cure?
The Medical Deontological Code of the Spanish General Council of Official Medical Colleges,12 in its article 12, recognizes the right of the patient to reject a treatment and frees the physician from having to apply a treatment which he or she considers inadequate or inacceptable. On the other hand, in article 36, the mentioned Code obliges physicians to adopt the measures required to ensure patient wellbeing when healing or improvement is no longer possible. In 2002, the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias, SEMICYUC) published a series of recommendations on LLST13 with the aim of offering orientations for promoting bioethical discussion. Limitation of life-sustaining treatment is applied in very diverse ways and has evolved in recent years. In order to know the current situation in this field, an analysis is made of the results of the multicenter “Evolution and prognosis of patients with prolonged ICU admission who suffer worsening” (Evolución y pronóstico de los pacientes con ingreso prolongado en UCI que sufren un empeoramiento, EPIPUSE) study. Specifically, the aim is to “know the frequency with which LLST is considered in patients with prolonged admission to the ICU; who proposes LLST; the consensus reached before LLST is applied; and the proportion of such decisions that are finally put into practice”.
Patients and methodsThe EPIPUSE study is a prospective, observational, multicenter cohort study of patients with prolonged admission to the ICU. In a first stage the Heads of Department of 152 Spanish ICUs were contacted. Of these Units, 75 were effectively incorporated to the recruitment phase. The list of participating investigators and centers is found in Appendix A. The project was approved by the Clinical Research Ethics Committee of Hospital Universitario Fundación Alcorcón (Alcorcón, Madrid, Spain), and was subsequently presented to the participating centers. The study moreover received the scientific endorsement of the SEMICYUC.
The patient recruitment period lasted three months, with a subsequent follow-up period of four additional months. The following inclusion criteria were applied: patients over 18 years of age with a stay in the ICU of 7 days or more and who experience a complication or adverse event with organic repercussions (increase in the SOFA scale of one point or more).
A complication or adverse event with organic repercussions was defined as a clinical event that worsens some organ function and has an impact upon the SOFA score, with a known or unknown cause, and attributable or not to a safety problem. Progressive worsening of a previously diagnosed clinical condition was excluded from this definition.
Limitation of life-sustaining treatment was carried out according to the protocols of the participating Units, and this process was not influenced by the present study. Three timepoints were considered in relation to LLST: (1) the moment in which LLST was considered; (2) the moment in which some type of LLST was formally decided after discussion among the medical team and was registered in the case history; and (3) the moment in which LLST was effectively applied.
We developed a database to record the patient demographic data and those personal antecedents capable of influencing the clinical course or conditioning patient recovery and complications. The clinical course and outcome were evaluated from the data referred to survival and duration of stay both in the ICU and in hospital. The causes of the complications were documented in descriptive and tabular form. The existence of possible previous instruction was recorded, together with the validity of such instructions in concrete cases. Regarding LLST, we documented the abovementioned timepoints, the subject proposing limitation (patient, relatives, professionals), the degree of agreement within the medical team (expressed as the percentage of physicians agreeing to LLST with respect to the total physicians present in the session), the impact of the decision upon the physician–patient–family relationship (using a tabular form), and the treatments applied or withdrawn. At the end of the patient follow-up period, the investigators in the different centers forwarded their anonymous and encrypted databases to the study sponsor for centralized integration of the information. Quantitative data were reported using central tendency and dispersion measures (mean and standard deviation, median and interquartile range Q1–Q3), while qualitative data were reported as absolute (n) and relative frequencies (%).
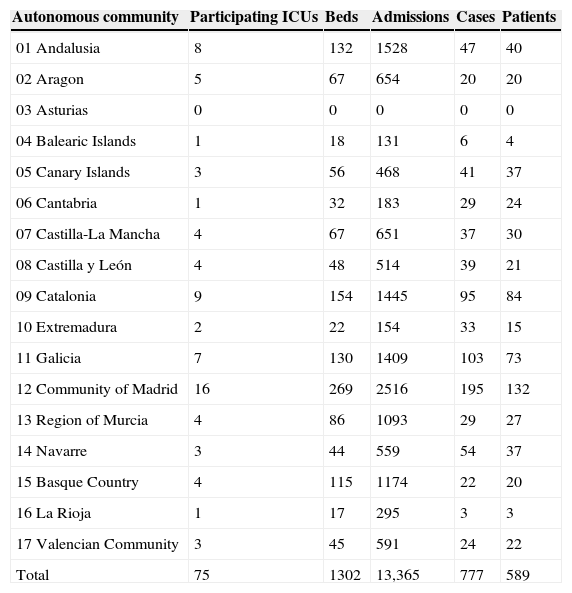
During the three months of the recruitment period, a total of 13,456 patients were admitted to the 75 participating ICUs, representing a total of 1302 beds. Of these subjects, 2594 registered a stay of 7 days or more. In this period of time there were 777 complications or adverse events with organic repercussions from day 7 of admission, affecting 589 patients. The distribution by Spanish Autonomous Communities is shown in Table 1.
Distribution of ICUs, cases and patients by Spanish Autonomous Communities.
| Autonomous community | Participating ICUs | Beds | Admissions | Cases | Patients |
|---|---|---|---|---|---|
| 01 Andalusia | 8 | 132 | 1528 | 47 | 40 |
| 02 Aragon | 5 | 67 | 654 | 20 | 20 |
| 03 Asturias | 0 | 0 | 0 | 0 | 0 |
| 04 Balearic Islands | 1 | 18 | 131 | 6 | 4 |
| 05 Canary Islands | 3 | 56 | 468 | 41 | 37 |
| 06 Cantabria | 1 | 32 | 183 | 29 | 24 |
| 07 Castilla-La Mancha | 4 | 67 | 651 | 37 | 30 |
| 08 Castilla y León | 4 | 48 | 514 | 39 | 21 |
| 09 Catalonia | 9 | 154 | 1445 | 95 | 84 |
| 10 Extremadura | 2 | 22 | 154 | 33 | 15 |
| 11 Galicia | 7 | 130 | 1409 | 103 | 73 |
| 12 Community of Madrid | 16 | 269 | 2516 | 195 | 132 |
| 13 Region of Murcia | 4 | 86 | 1093 | 29 | 27 |
| 14 Navarre | 3 | 44 | 559 | 54 | 37 |
| 15 Basque Country | 4 | 115 | 1174 | 22 | 20 |
| 16 La Rioja | 1 | 17 | 295 | 3 | 3 |
| 17 Valencian Community | 3 | 45 | 591 | 24 | 22 |
| Total | 75 | 1302 | 13,365 | 777 | 589 |
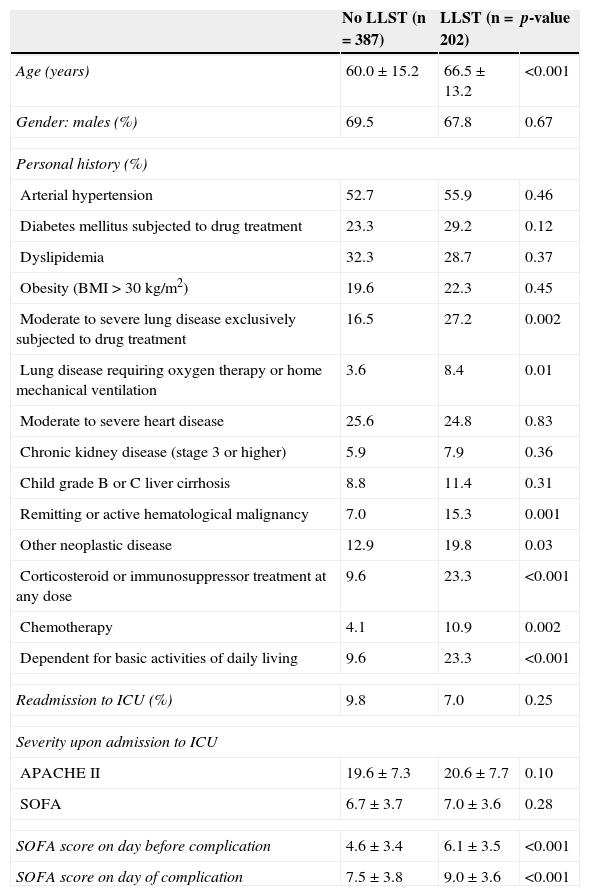
The patients included in the EPIPUSE study were between 18 and 94 years old. Limitation of life-sustaining treatment was proposed in 202 of the 589 patients included in the study (34.3%). Table 2 describes the baseline characteristics and information referred to admission of the included cases according to whether some form of LLST was considered or not.
Baseline characteristics and evolution during admission.
| No LLST (n=387) | LLST (n=202) | p-value | |
|---|---|---|---|
| Age (years) | 60.0±15.2 | 66.5±13.2 | <0.001 |
| Gender: males (%) | 69.5 | 67.8 | 0.67 |
| Personal history (%) | |||
| Arterial hypertension | 52.7 | 55.9 | 0.46 |
| Diabetes mellitus subjected to drug treatment | 23.3 | 29.2 | 0.12 |
| Dyslipidemia | 32.3 | 28.7 | 0.37 |
| Obesity (BMI > 30kg/m2) | 19.6 | 22.3 | 0.45 |
| Moderate to severe lung disease exclusively subjected to drug treatment | 16.5 | 27.2 | 0.002 |
| Lung disease requiring oxygen therapy or home mechanical ventilation | 3.6 | 8.4 | 0.01 |
| Moderate to severe heart disease | 25.6 | 24.8 | 0.83 |
| Chronic kidney disease (stage 3 or higher) | 5.9 | 7.9 | 0.36 |
| Child grade B or C liver cirrhosis | 8.8 | 11.4 | 0.31 |
| Remitting or active hematological malignancy | 7.0 | 15.3 | 0.001 |
| Other neoplastic disease | 12.9 | 19.8 | 0.03 |
| Corticosteroid or immunosuppressor treatment at any dose | 9.6 | 23.3 | <0.001 |
| Chemotherapy | 4.1 | 10.9 | 0.002 |
| Dependent for basic activities of daily living | 9.6 | 23.3 | <0.001 |
| Readmission to ICU (%) | 9.8 | 7.0 | 0.25 |
| Severity upon admission to ICU | |||
| APACHE II | 19.6±7.3 | 20.6±7.7 | 0.10 |
| SOFA | 6.7±3.7 | 7.0±3.6 | 0.28 |
| SOFA score on day before complication | 4.6±3.4 | 6.1±3.5 | <0.001 |
| SOFA score on day of complication | 7.5±3.8 | 9.0±3.6 | <0.001 |
The reasons for admission to the ICU were highly varied: 14.4% of the patient were admitted because of pneumonia, 13.9% due to sepsis in some other location, 12.9% because of respiratory failure of other origins, 7.9% due to cardiological reasons, 5.9% following recovered cardiorespiratory arrest, and 9.9% due to neurological causes. The remaining 35.1% corresponded to diseases of lesser prevalence (postoperative conditions, trauma, gastrointestinal problems, etc.).
Regarding the complications or adverse events leading to inclusion in the study, 19.3% corresponded to pneumonia, 17.8% to other infections, 14.9% to respiratory failure of other origins, and 8.9% to neurological complications.
The mortality rate in the ICU was 21.6% among the cases in which LLST was not considered and 82.7% in those in which limitation measures were considered (p<0.001). The in-hospital mortality rate was 28.7% and 93%, respectively (p<0.001).
Differences were also found between the duration of stay in the ICU and in hospital. Specifically, the duration of stay in the ICU was 35.6±29.6 days among the patients in which LLST was not considered, versus 27.3±22.1 days in those in which limitation measures were considered (p<0.001). In turn, the duration of stay in hospital was 58.8±38.7 and 38.3±31.1 days, respectively (p<0.001).
At the end of the follow-up period, 9 patients were still in the ICU and an additional 14 had been moved to the hospital ward. None of the included patients had issued previous written instructions referred to LLST. A total of 16 patients (2.7%) were admitted to the ICU with the previous decision not to apply some concrete type of treatment (e.g., intubation).
No statistically significant differences were recorded on comparing the characteristics of the patients in which LLST was considered versus those in which no limitation measures were contemplated, with the exception of age.
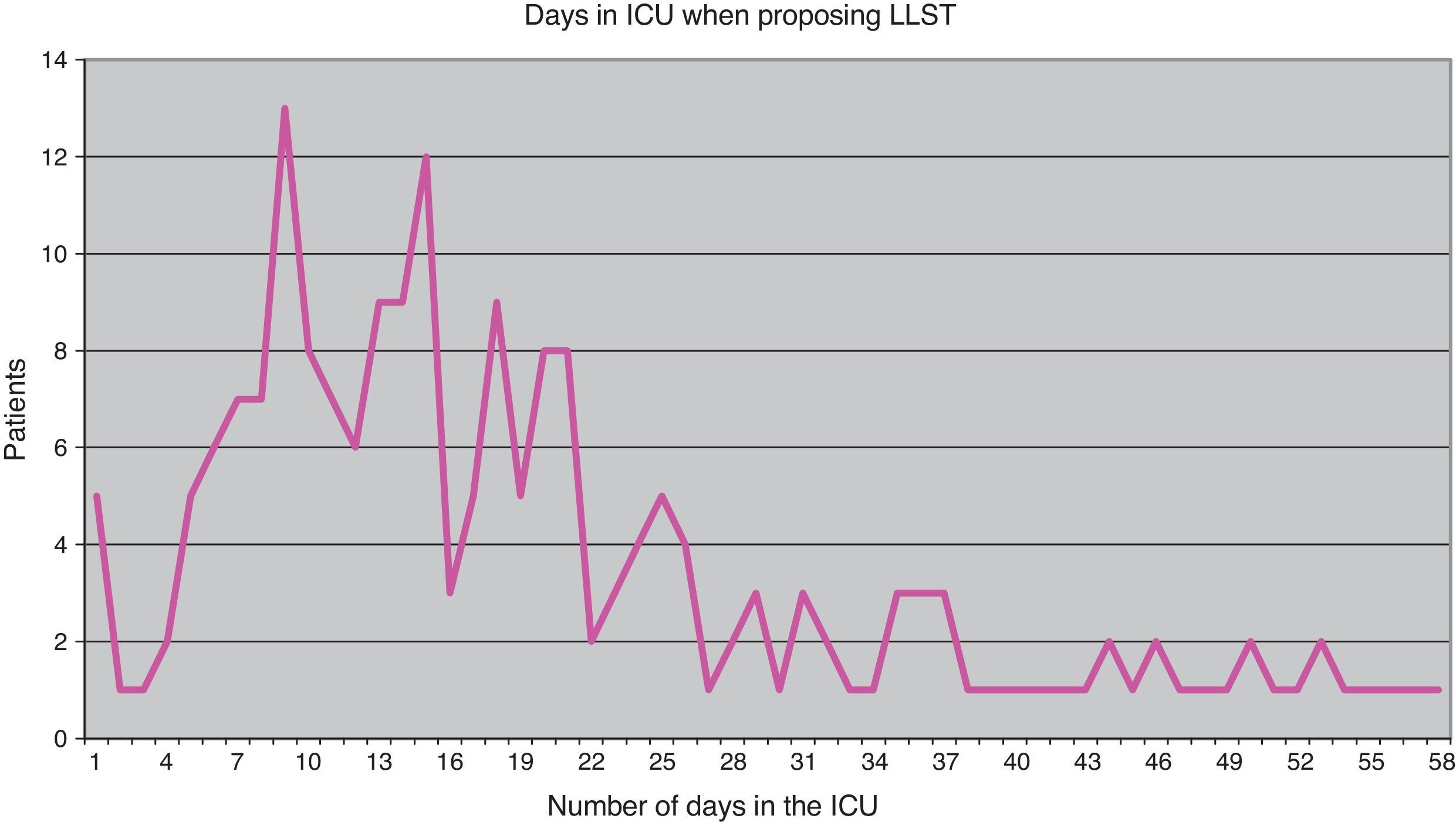
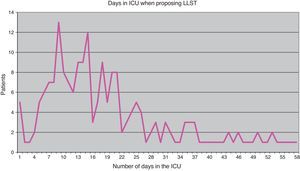
Of the 202 cases in which the limitation of some kind of treatment was considered, the decision to do so was made in 196 cases (97%), and LLST was finally put into practice in 183 cases (90.6%). The moment in which LLST was first considered proved highly variable (Fig. 1). On average, the possibility was considered on day 23 of admission, though the standard deviation was large (20 days). The median corresponded to day 13, and the interquartile range to 11–27. The time from LLST proposal to the actual decision to apply LLST was also variable, though in 118 cases (60.2%) the decision was made on the same day on which LLST was proposed, in 34 cases (17.3%) the decision was made on the following day, and in 33 cases (16.8%) the decision to apply LLST was made in the course of the following week. In 11 cases the decision was made at a later time. Regarding the time elapsed from the decision to apply LLST to actual implementation of the limitation measures, in most cases application was on the same day (150 cases, 82%), while in 17 cases (9.3%) application was on the next day, in 13 cases (7.1%) it took place in the course of the same week, and finally in three cases application took place at a later point in time.
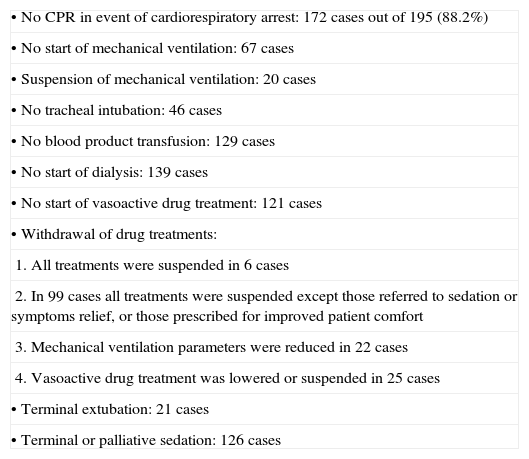
The limited treatments or attitudes adopted in 195 of the 196 cases of the study are reflected in Table 3.
Limited treatments and other interventions.
| •No CPR in event of cardiorespiratory arrest: 172 cases out of 195 (88.2%) |
| •No start of mechanical ventilation: 67 cases |
| •Suspension of mechanical ventilation: 20 cases |
| •No tracheal intubation: 46 cases |
| •No blood product transfusion: 129 cases |
| •No start of dialysis: 139 cases |
| •No start of vasoactive drug treatment: 121 cases |
| •Withdrawal of drug treatments: |
| 1. All treatments were suspended in 6 cases |
| 2. In 99 cases all treatments were suspended except those referred to sedation or symptoms relief, or those prescribed for improved patient comfort |
| 3. Mechanical ventilation parameters were reduced in 22 cases |
| 4. Vasoactive drug treatment was lowered or suspended in 25 cases |
| •Terminal extubation: 21 cases |
| •Terminal or palliative sedation: 126 cases |
Of the 183 cases in which some type of LLST was finally applied, the mortality rate was 97.8%. The time from the moment of application of LLST to death was as follows: 94 patients (51.4%) died on the same day as the application of LLST, 42 patients (23%) died on the following day, and 30 patients (16.4%) died in the course of the same week. The remaining 13 deaths occurred in the course of the month, with the exception of a single patient who died after 51 days.
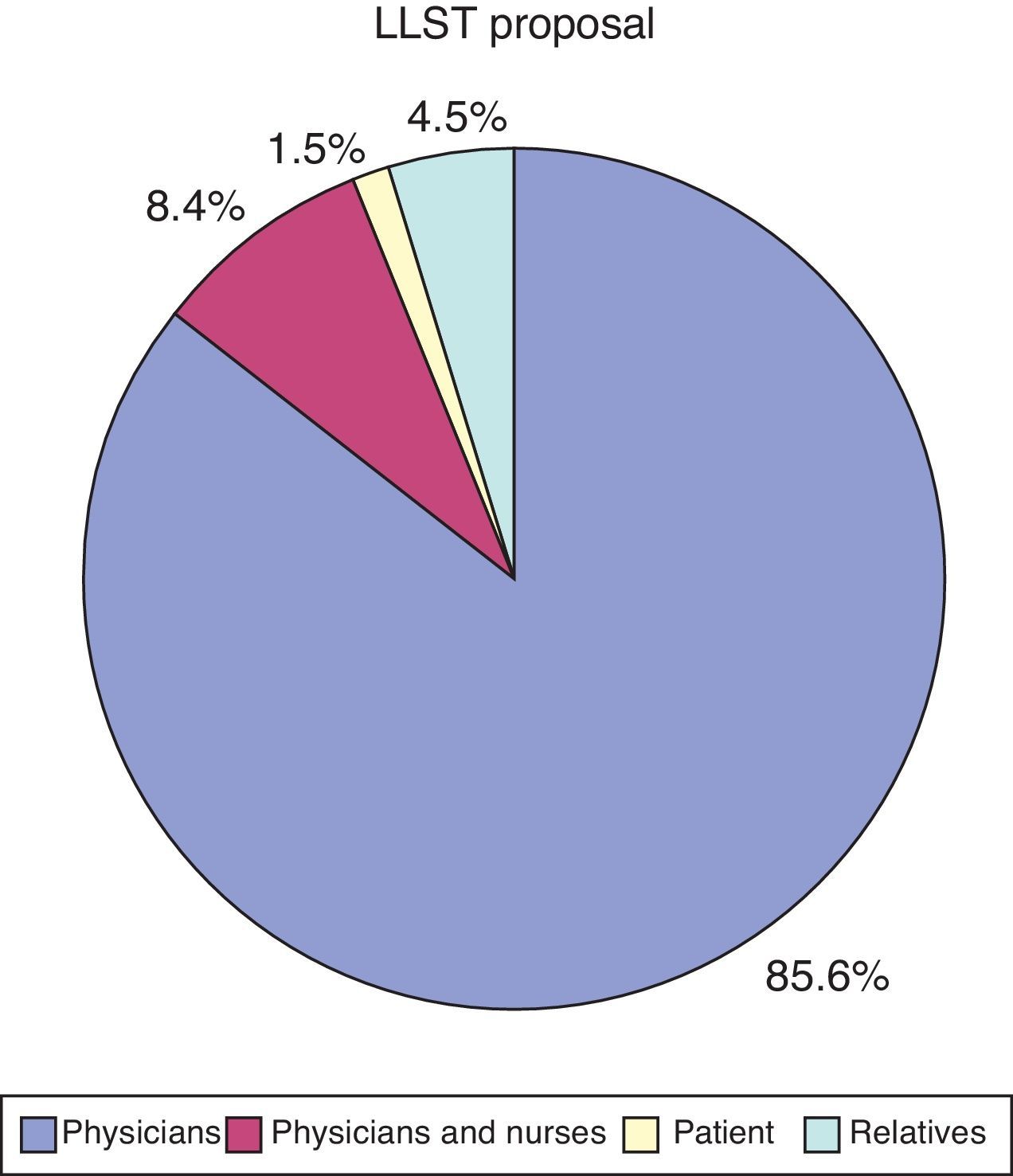
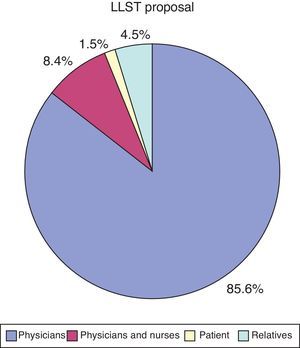
The proposal to apply LLST came from the healthcare personnel attending the patient in 190 cases (Fig. 2). In three cases the proposal came from the patient in person; in 172 cases (85.1%) the patient was in coma or was considered unable to participate in the proposal; in three cases (1.5%) the patient did not participate but was informed of the proposal; and in the remaining 24 cases (11.9%) the patient was neither consulted nor informed.
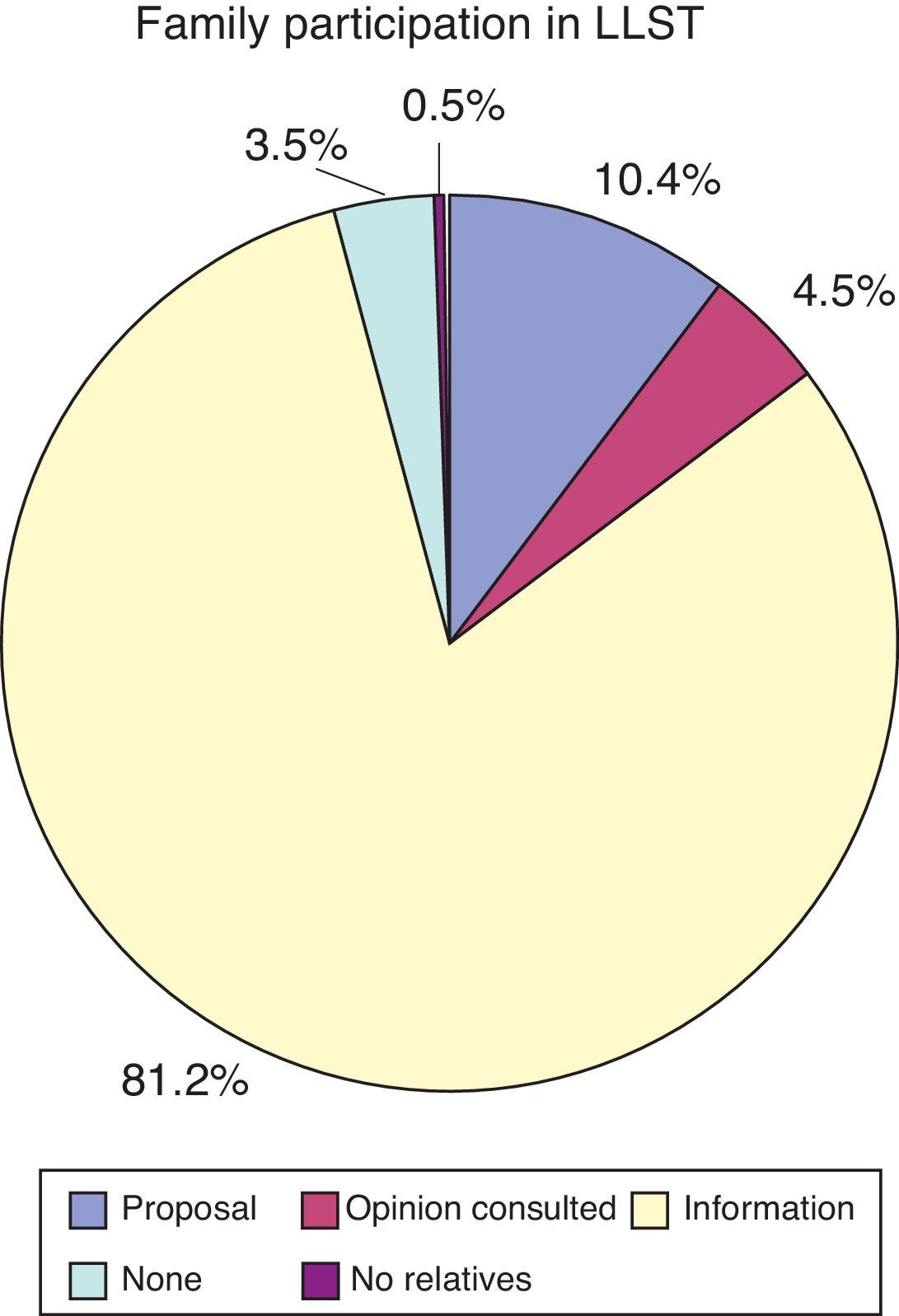
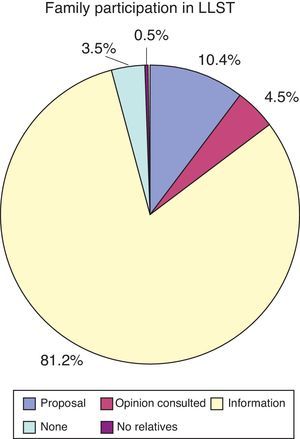
Regarding participation of the relatives in the decisions referred to LLST, 21 families (10.4%) proposed the limitation measures, and in 9 cases (4.5%) the relatives were asked about their opinion. In 164 cases (81.2%) they were informed of the decision once it had been made, and finally in 7 cases (3.5%) the medical team did not inform the relatives of the decision on LLST. In no case did a patient ask that the relatives not be informed (Fig. 3).
Regarding the degree of agreement within the medical team on the final decision referred to LLST, in 172 cases (87.8%) agreement was unanimous, while in 13 cases (6.6%) the decision was supported by 60–90% of the team members, and in three cases (1.5%) it was supported by only 40–50% of the medical team.
Lastly, regarding the impact of the proposition/decision on LLST upon the physician–patient–family relationship, the investigators considered that the decision improved the relationship with the patient or relatives, or both, in 73 cases, worsened the relationship with the relatives in 12 cases, and produced no significant changes in the physician–patient–family relationship in 110 cases.
DiscussionThe forms of LLST applied in the ICU setting can be highly diverse. Patient admission to the Unit may be rejected, or admission may be accepted having pre-established certain limitations in the life support measures to be applied. Another option is to not start or to withdraw some or all support measures, such as CPR, mechanical ventilation, oxygen therapy, extrarenal filtration, vasoactive drug support, etc. In the case of patients who are already in the ICU, although consensus is lacking, protocols have been proposed for application once the physicians realize that the patient will probably die and that intensive treatment is not warranted.14,15 In fact, there are important differences in attitude between teams and even between members of one same team.16–22 Undoubtedly, training in ethical issues influences decision making.23,24
In recent years there have been many publications on the type and frequency of LLST applied in the ICU. Because of its size and proximity, we will describe the results of the English registry corresponding to the period 1995–2001.25 According to this registry, all active treatment was suspended in 9.9% of the patients, with a mortality rate of 99%, but with important differences between Units–thus suggesting non-uniform application of such decisions. Mortality among the patients subjected to LLST in the ICU represented approximately one-third of the overall deaths at hospital discharge. Data fitting to different models identified a number of factors associated to the decision to suspend all active treatment, including patient age, pre-existing serious illness, emergency surgery or emergency admission to the ICU, the application of CPR in the 24h prior to admission, and the need for ventilation or sedation/neuromuscular block in the first 24h of admission–with few changes over the course of the study period. Similar risk factors were described by Meissner et al.26 in a postsurgery ICU.
In a similar manner, though in the context of an international study, the data on the ICUs that participated in the development of the SAPS 3 scale27 showed that some type of LLST was applied in 8.6% of the patients admitted to the ICU (in about one-half of the cases the measure consisted of not starting a certain treatment, and in the other half it consisted of suspending a treatment). It was confirmed that one-third of the overall deaths at hospital discharge corresponded to cases in which LLST had been applied, with an in-hospital mortality rate of 80–95% among the patients subjected to LLST. The time from admission to the decision on LLST was 2–4 days. It is interesting to consider the factors associated to the decision on LLST, since there were clinical causes (most of the severity variables contemplated by the SAPS 3) and also structural or organizational factors. In effect, LLST was seen to be more common in hospitals lacking an Emergency Care Department, in small ICUs and in Units with a low nurse/patient ratio, a larger number of physicians per bed, centers in which multidisciplinary meetings are held, and in centers where nurses and intensivists jointly visit the patient. In contrast, LLST was less frequent in ICUs with the presence of an intensivist on a continuous basis.
The largest study on LLST in European ICUs was carried out in the years 1999 and 2000: the End-of-Life Practices in European Intensive Care Units (ETHICUS) study,28 with data on the ICUs of 17 countries, and in which important differences in relation to decisions on LLST were observed among the different countries. In the subanalysis of the reasons given by physicians for deciding LLST, the most frequent reason was the principal disease condition of the patient (79%), particularly failure to respond to treatment (46%), while chronic diseases (12%), quality of life (4%), age (2%), and patient or family request (2%) were infrequent reasons.
Regarding the frequency of LLST decisions in the ICU, and although the results of the different series vary, it can be concluded that 40–90% of all deaths in the ICU were preceded by some form of LLST.29–36 The frequency with which such decisions are made is not clear but is probably underestimated.37 As an example, in a recent study in the region of Murcia (Spain), the authors underscored the low frequency with which patients are asked about their end-of-life wishes.38
In our study, of the 589 patients who developed complications beyond day 7 of admission to the ICU, the application of LLST was considered in 202 cases (34.3% of the patients). Similar figures have been reported by other series.
In many studies on the factors associated to LLST, patient age is cited as a minor criterion. In our series, the mean age of the patients subjected to LLST of some kind was 66.5 years, and was significantly different from the age of the patients who did not undergo LLST. However, the recorded mean age does not suggest patient age to have been an important factor. In any case, the study was not designed to know the reasons for proposing LLST but to simply describe such practices.
In general, it can be affirmed that the profile of the patient in which LLST is considered is comparable to that of the rest of the patients in the sample, though with some significant differences. In effect, among the patients subjected to LLST of some kind, the presence of moderate to severe lung disease, cancer, or corticosteroid or immunosuppressor therapy was comparatively more common. Likewise, in the group of individuals who ultimately underwent LLST there was a larger presence of dependent patients. Therefore, and in coincidence with different descriptive studies,25,27 the personal history or antecedents of the patients were seen to influence the decision to adopt LLST measures.
Most LLST proposals were seen to come from the medical team, as has already been described by Esteban et al.39 Likewise, we found that usually there is agreement in applying LLST once it has been proposed. Indeed, LLST was finally applied in 97% of the cases in which it was initially considered. There are a number of possible explanations for this. On one hand, it may be assumed that there is great caution among patients, relatives and professionals in proposing LLST, given the consequences of the decision. However, we all know that decision making may prove difficult in medical practice, and that different actions are proposed by different physicians in reference to one same patient. If this is so in any clinical decision, it can also be expected to occur in the case of LLST–though this is not supported by our data. On the other hand, it may be assumed that great confidence is placed in the physician treating the patient (as the subject who most often proposes LLST) by the rest of the healthcare professionals as well as by the patients and relatives, and this causes them to support the proposal in the great majority of cases. Regardless of the explanation, it must be taken into account that our sample was limited to patients suffering a serious complication in the context of prolonged admission to the ICU. The data are therefore not directly extendable to LLST decisions in other scenarios. In concordance with this, it should be noted that the decision referred to LLST was made around day 13 of admission to the ICU, and this probably reflects the fact that in many cases LLST is proposed after having confirmed the futility of treatment in the ICU.
The fact that LLST was applied in most cases in which it was proposed is also related to generally unanimous agreement within the medical time in deciding LLST (the figure being 87.8% of the cases in our series), in line with the recommendation of the SEMICYUC.12 Nevertheless, here again there is important room for improvement, since it is surprising that in 12.2% of the cases some team members were not agreed with LLST, though the limiting measures were applied anyway. Similar data have been published by Iribarren-Diarasarri et al.40
Our study reflects a low percentage of cases in which the proposal to limit treatment came from the nursing personnel. This is probably because in many ICUs the nurses do not participate in the clinical sessions, and so their personal opinion may not have been reflected in the collected data.41,42
Many studies have examined the physician–patient–family relationship in the context of LLST decision making.43–45 In this respect, our data indicate a good relationship between the professionals and the patients and relatives. Admittedly, our assessment is based on subjective physician appraisal of the quality of the relationship with the patients and relatives; however, the number of responses indicating improvement in the relationship suggests that the finding is genuine. As the days go by, and on the basis of the visits and the information received, it is common for the relatives to realize that the poorly evolving patient has few chances of surviving. Furthermore, close knowledge and familiarity with the ill patient in many cases causes them to subjectively feel that he or she will not be able to survive. In this situation, if the physician moreover confirms their “suspicion”, the relatives tend to suffer anxiety due to the possibility of “bad dying” (dysthanasia), and the suggestion of modifying the management strategy by adopting LLST is usually well accepted.
As a treatment measure in the most extreme situation, the most frequently considered type of LLST is not to perform CPR in the event of cardiorespiratory arrest. One of the difficulties in our study is the possible under-reporting of decisions referred to future actions (particularly the non-application of some treatment). Although the most common of these decisions regarding future treatments refers to the withholding of CPR if the patient suffers cardiac arrest, it is possible that not all the decisions referred to the avoidance of intubation, ventilation, dialysis, transfusion, etc. have been duly reflected. What leads us to consider this possibility is the fact that the intention not to intubate the patient was only recorded in 23.6% of the cases–though it is also possible that this percentage may be due to a high proportion of patients who are already intubated at the time the decision is made. Other actions associated to a similar incidence of decisions not to perform future treatments are renal replacement therapy (71.3%), the transfusion of blood products (66.2%) and the use of vasoactive drugs (62.1%).
Regarding the actions to be applied at the actual time of the decision, mention must be made of terminal or palliative sedation (in 64.6% of the cases), and terminal extubation (10.8%).
Another relevant aspect is drug management in LLST. The most common practice was found to be the suspension of all drugs except those used to afford patient comfort or analgesia. However, in some cases absolutely all drug treatment was suspended–this undoubtedly being a point amenable to improvement. Likewise, as a more gradual way to apply LLST, reduction of the mechanical ventilation parameters was decided in 11.3% of the cases, while in 12.8% of the patients the decision was made to lower or suspend vasoactive medication without suppressing other treatments. The data recorded in these cases were not enough to explain or justify this attitude, which should be revised. In 12.3% of the cases the LLST decision was to not increase the level of treatment–a fact that may explain the mortality rate of under 100%.
We consider that this study has some strengths that should be pointed out. A first consideration is the large sample, comprising over 2500 patients with prolonged admission to the ICU over a recruitment period of three months. Also significant is the large number and wide distribution of the participating centers, covering practically all of Spain. This makes the sample representative of the current situation in Spanish ICUs. Such heterogeneity, also manifested by the broad range of diseases involved, makes it possible to extrapolate the findings to other centers.
Our study also has a series of limitations that must be commented. According to the EPIPUSE study inclusion criteria, the patients were required to present complications from the second week of admission. As a result, we only documented patients suffering complications with organic repercussions in the context of prolonged admission to the ICU; consequently, the data obtained can only be extrapolated to this particular patient subpopulation. Given the recruitment period in our study (three months), we cannot rule out the possibility that seasonal differences might influence the results.
ConclusionsSome type of limitation of life-sustaining treatment (LLST) is applied to one-third of all patients who develop complications or adverse events with organic repercussions from the second week of admission to the ICU. Decisions referred to LLST are more frequent in patients with lung disease, cancer or with dependency for basic activities of daily living. In general, such decisions arise from the medical team and are established by consensus within the team, with the agreement of the relatives and, to a lesser extent, of those patients in condition to participate in the decision making process. In our clinical setting, previous instruction documents are usually not available for decision making.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Thanks are due to Ms. Elia Pérez, of the Research Unit of Hospital Universitario Fundación Alcorcón, for her contribution to the methodology and statistics.
ANDALUSIA: Francisco José Saldaña González (Clínica Santa Isabel), José Manuel Galván Martín (Hospital Costa del Sol), Rocío Monterroso (Hospital Jerez de la Frontera), José Rubio Quiñones (Hospital Puerta del Mar), Ramón Díaz Alersi (Hospital Puerto Real), Dolores María Mayor García e Isabel Rodríguez Higueras (Hospital Torrecárdenas), Mercedes Barranco Ruiz (Hospital Universitario Virgen de las Nieves), José Antonio Sánchez Román (Hospital Universitario Virgen de Valme). ARAGON: Miguel Ángel Suárez Pinilla and Carlos López Núñez (Hospital Clínico Universitario Lozano Blesa), Juan Carlos García Ronquillo (Hospital de Barbastro), Mónica Zamora Elson (Hospital General San Jorge), José Carlos Torralba Allué (Hospital Obispo Polanco), Gabriel Tirado Anglés (Hospital Royo Villanova). BALEARIC ISLANDS: Rosa Poyo-Guerrero Lahoz and Catalina Forteza Cañelas (Hospital Son Llàtzer). CANARY ISLANDS: Ruth Santacreu (Complejo Hospital Universitario de Canarias), Montserrat Sisón Heredia (Hospital Doctor José Molina Orosa), Dácil Parrilla Toribio and Sergio Tomás Rodríguez Ramos (Hospital Universitario Nuestra Señora de la Candelaria). CANTABRIA: Mónica Cordero Vallejo and Álvaro Castellanos Ortega (Hospital Universitario Marqués de Valdecilla). CASTILLA-LA MANCHA: Ana Bueno González (Hospital General Universitario de Ciudad Real), Jerusalén Villegas del Ojo (Hospital Santa Bárbara), Carmen Benito Puncel (Hospital Universitario de Guadalajara), Pilar Sánchez Rodríguez (Hospital Virgen de la Salud). CASTILLA Y LEÓN: Christian J. Sala Scarbay (Complejo Asistencial de Soria–Hospital de Santa Bárbara), Teresita Loreto Álvarez Pérez and F. Concepción Tarancón Maján (Complejo Asistencial de Zamora–Hospital Virgen de la Concha), Myriam González (Complejo Asistencial Universitario de León–Hospital de León), Ramón Cicuéndez Ávila (Hospital Clínico Universitario de Valladolid). CATALONIA: Joaquín Amador Amérigo (Consorci Sanitari de Terrassa–Hospital de Terrassa), Glòria Miró Andreu (Consorci Sanitari del Maresme–Hospital de Mataró), Antoni Mas and Aníbal Silva (Corporació Sanitària Clínic–Hospital Universitari Clínic de Barcelona IDIBAPS–UCI de Enfermedades Digestivas), Elisabeth Zavala (Corporació Sanitària Clínic–Hospital Universitari Clínic de Barcelona IDIBAPS–UCI Quirúrgica), Olga Rubio Sanchiz (Fundació Althaia–Hospital Sant Joan de Déu de Manresa), Marta Basas (Hospital del Mar), Miguel León Vallés and Silvia Iglesias Moles (Hospital Universitari Arnau de Vilanova de Lleida), Marcos Ibáñez (Hospital Universitari Joan XXIII), Isabel Cherta (Hospital Universitari Mútua Terrassa). EXTREMADURA: María José García Ramos and Federico Minaya González (Complejo Hospitalario de Cáceres–Hospital San Pedro de Alcántara), Noemí Mara Gil Pérez (Complejo Hospitalario del Área de Salud de Mérida–Hospital de Mérida). GALICIA: María Sandra Gómez Canosa (Complejo Hospitalario Arquitecto Marcide-Novoa Santos–Hospital Arquitecto Marcide), Santiago Freita Ramos (Complejo Hospitalario de Pontevedra), Iván Astola Hidalgo and Mónica Mourelo Fariña (Complejo Hospitalario Universitario de A Coruña–Hospital A Coruña), Eva Saborido Paz (Complejo Hospitalario Universitario de Santiago–Hospital Clínico Universitario), Miguel Ángel Pereira Loureiro (Complejo Hospitalario Universitario de Vigo–Hospital Meixoeiro–UCP), Mélida García Martul and María José Rodríguez Fernández (Complejo Hospitalario Universitario de Vigo–Hospital Xeral Cies), José Vicente Bravo Doviso (Complejo Hospitalario Xeral-Calde de Lugo–Hospital Universitario Lucus Augusti). COMMUNITY OF MADRID: María Cruz Martín Delgado (Hospital Universitario de Torrejón), María Belén Estébanez Montiel (Hospital del Tajo), José Manuel Gómez García (Hospital General Universitario Gregorio Marañón), Eduardo Arias Sarmiento (Hospital Universitario 12 de Octubre), Ricardo Andino Ruiz, Marta García Costas and Ana Leal Micharet (Hospital Universitario de La Princesa), Teresa Honrubia Fernández (Hospital Universitario de Móstoles), María Victoria Enciso Calderón (Hospital Universitario del Henares), Alberto Hernández-Tejedor (Hospital Universitario Fundación Alcorcón), Domingo Díaz Díaz (Hospital Universitario Infanta Leonor), Gonzalo Hernández (Hospital Universitario Infanta Sofía), Abelardo García de Lorenzo (Hospital Universitario La Paz–UCI Quemados), José Alberto Gallardo Álvarez and Ángel Luis Córdoba Sánchez (Hospital Universitario Madrid Norte Sanchinarro), José Andrés Cambronero Galache (Hospital Universitario Príncipe de Asturias), Inmaculada Fernández Simón and Miguel Valdivia de la Fuente (Hospital Universitario Puerta de Hierro Majadahonda), Félix Lacoma (Hospital Universitario Quirón Madrid), Isidro Prieto del Portillo (Hospital Universitario Ramón y Cajal). REGION OF MURCIA: Antonia López Martínez (Hospital General Universitario Morales Meseguer), Luis Herrera Para and Salvador Moreno Aliaga (Hospital General Universitario Santa Lucía), Carmen M. Susarte Juliá (Hospital Universitario Reina Sofía de Murcia), María Martínez Martínez (Hospital Universitario Virgen de la Arrixaca). NAVARRE: Pablo Monedero (Clínica Universidad de Navarra), María Barber Ansón (Complejo Hospitalario de Navarra–UCI-A–Hospital de Navarra), Eva Regidor Sanz and Laura Macaya Redín (Complejo Hospitalario de Navarra–UCI-B–Hospital Virgen del Camino). BASQUE COUNTRY: Mónica Domezain del Campo (Hospital Universitario Cruces), Alberto Manzano Ramírez and Yolanda Poveda Hernández (Hospital Universitario de Araba–Sede Santiago), Juan Fernando Castedo González (Hospital Universitario de Araba–Sede Txagorritxu), Itziar Mintegui Malcorra and Itxaso Elosegui Plaza (Hospital Universitario Donostia). LA RIOJA: José Luis Monzón Marín and Lidia Martínez Camarero (Hospital San Pedro), VALENCIAN COMMUNITY: Manuel Palomo Navarro (Hospital de Sagunt), Ana Llamas Álvarez (Hospital General Universitario de Elche), Pedro Kot (Hospital Universitario y Politécnico La Fe de Valencia).
The names of the investigators and participating centers are listed in Appendix A.
Please cite this article as: Hernández-Tejedor A, Martín Delgado MC, Cabré Pericas L, Algora Weber A, miembros del grupo de estudio EPIPUSE. Limitación del tratamiento de soporte vital en pacientes con ingreso prolongado en UCI. Situación actual en España a la vista del Estudio EPIPUSE. Med Intensiva. 2015;39:395–404.