Recommendations to establish adequate visiting hours have already been published in the guidelines of different scientific societies.1 SEMICYUC2 believes that relaxing visiting hours may be an indicator of the quality of care provided to critically ill patients (2017). Also, it is considered a priority in the implementation of humanization plans.3
The goal of this study was to know the opinion of healthcare providers, patients, and families on the actual visiting system of the ICU of the Galdakao-Usánsolo Hospital while the study was being conducted. Also, to assess the possibility of achieving consensus in the implementation of an open-door policy. This was a descriptive, correlational study conducted in an intensive care unit with 15 polyvalent wards. During 2017, 1081 patients were admitted, 607 of whom remained hospitalized for over 48h.
Data mining was conducted through an anonymous survey specifically designed for this purpose and for every participant group including socio-demographic variables and working characteristics, matters of opinion, and open questions.
Variables were expressed as frequency and percentage. The bivariate analysis was conducted using the chi-squared test and Fisher's exact test. P values<.05 were considered statistically significant.
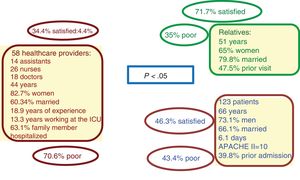
This study included 58 healthcare providers (the entire ICU personnel), 120 close relatives (78.3% were spouses or first-degree relatives), and 123 patients whose basic characteristics are shown in Fig. 1. Sixty-five-point-five percent of the healthcare providers, 53.7% of the patients, and 28.3% of the relatives were not satisfied with the actual visiting system. Seventy-seven-point-six percent of the healthcare providers, 56.9% of the patients, and 43% of the relatives said the system was actually poor. This means that healthcare providers and patients are less satisfied with the actual system and that, basically, it is the healthcare providers who demand changes.
The fact that most relatives are satisfied would be explained by the fact that family expectations are low when a loved one has been admitted to an ICU. First because of the patient's severity. Second, because general wisdom suggests that visiting hours should be limited in an ICU. These low expectations raise their level of satisfaction as other studies have described.4,5
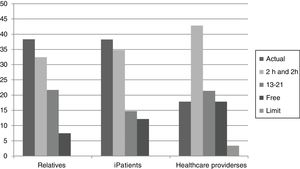
Five possible time schedules were proposed (limit the actual schedule that goes from13:00 to 14:00h and from 20:00 to 21:00h; keep it; add 2 more hours in the morning and 2 in the afternoon; extend it from 13:00 to 21:00h or free visiting hours). The most popular proposals from the 3 groups involve extending the actual visiting system without significant differences among the 3 groups (Fig. 2). The most voted time schedule extension of all is the most restrictive one (add 2 more hours in the morning and 2 in the afternoon). When asked for the extension from 13:00 to 21:00, most healthcare providers (55.2%), patients (60.2%), and relatives (51.2%) disagree.
We did not find any correlations between the socio-demographic variables collected and the wish or rejection to extend the schedule. No significant differences were seen either except for age being patients<50 more prone to extending the schedule (77%) compared to patients>50 (40% of whom opposed extending the schedule, P<.01). This is probably the age group who have lived visiting hour restrictions and other needs as a necessary evil.
Ninety-three-point-one percent of the relatives believe that the family helps during recovery; healthcare providers (58.6%) and patients (71.3%) are of the same opinion but in a lower percentage (P<.0001). However, almost 40% of the relatives believe that their presence can be bad for the patients or themselves. This has been reported in other studies6 that attributed visits a stress factor for both patients and relatives who have to abandon their obligations, go to the ICU, etc.
Neither the relatives nor the patients believe that extending the time schedule will generate conflicts with the healthcare personnel. However, the healthcare providers remain quiet on this regard. Our study compared the opinion of doctors and nurses and confirmed the differences reported by other publications.7,8 Over half of the nursing staff say that extending the time schedule may generate conflicts compared to only 16.7% of the doctors. These percentages have already been reported in other studies.9,10
Opinions on the visits of minors are varied. Although most people from the 3 groups oppose it, patients have a significantly more favourable attitude towards it (27.8%) maybe because they see these visits as a powerful stimulus for recovery.
The presence of relatives during the performance of non-aggressive medical acts is accepted by most healthcare providers despite they feel they’re being audited. However, it is not accepted by most relatives and patients who think this presence can be disturbing. The 3 groups openly oppose the presence of relatives in aggressive medical acts.
Two are the basic problems included in the open questions asked to the 3 groups: disturbing the patient and disturbing the healthcare provider. The suggestions made here are minor extensions of the time schedule and hour flexibility. We believe that this suggested flexibility is unfeasible without a wide enough schedule to meet the needs of every individual. This means that extending the schedule should come before flexibility.
Unlike healthcare providers and patients, relatives are mostly satisfied with the actual visiting system. They all want more flexibility and visiting hours far beyond the open-door policy. Maybe the historic lack of this freedom is now blurring how necessary it actually is.
This study (Humanization Plan of the intensive care unit of the Galdakao-Usansolo Hospital. April 2018) has allowed us to make proper plans regarding the needs of patients and relatives. Consistent with other studies, it also shows the red lines regarding extended visiting hours.8 Finally, it has helped changed this hospital visiting hours and implemented a huge humanization plan.
Conflict of interestNone of the authors has any conflicts of interest and no funding has been received to conduct this study.
We wish to thank the entire ICU personnel who participated in this survey and shared their time and opinions with us. Also, we wish to thank the hospital Research Service for its collaboration and willingness to conduct the study statistical analysis.
Please cite this article as: Arnaiz Arnaiz V, Esteban Galbete MT, Olaechea Astigarraga PM, Legarreta Olabarrieta MJ. Escuchando a profesionales, pacientes y familiares: estudio sobre el régimen de visitas en una Unidad de Cuidados Intensivos. Med Intensiva. 2020;44:254–256.