Accidental hypothermia is an environmental condition with basic principles of classification and resuscitation that apply to mountain, sea or urban scenarios. Along with coagulopathy and acidosis, hypothermia belongs to the lethal triad of trauma victims requiring critical care. A customized healthcare chain is involved in its management, extending from on site assistance to intensive care, cardiac surgery and/or the extracorporeal circulation protocols.
A good classification of the degree of hypothermia preceding admission contributes to improve management and avoids inappropriate referrals between hospitals. The most important issue is to admit hypothermia victims in asystolia or ventricular fibrillation to those hospitals equipped with the medical technology which these special clinical scenarios require.
This study attempts to establish the foundations for optimum management of accidental hypothermia from first emergency care on site to treatment in hospital including, resuscitation and rewarming with extracorporeal circulation.
La hipotermia accidental es una patología ambiental con unos principios básicos de clasificación y reanimación que sirven tanto para el medio montañoso, marítimo o urbano. Esta patología ha formado parte, junto a la acidosis y la coagulopatía, de la famosa «tríada letal» de las víctimas traumáticas en situación crítica. En su manejo y asistencia está implicada toda una cadena asistencial que se extiende desde la medicina de urgencia prehospitalaria hasta la medicina intensiva, llegando incluso hasta la cirugía cardiaca y/o a los programas de circulación extracorpórea.
Una buena clasificación prehospitalaria del grado de hipotermia facilitará su manejo inicial y evitará traslados interhospitalarios o secundarios innecesarios. Lo fundamental es trasladar, con la mayor urgencia posible, a las víctimas hipotérmicas en asistolia o fibrilación ventricular hasta aquellos hospitales que tengan la capacidad tecnológica adecuada para el tratamiento de estas especiales situaciones clínicas.
Este artículo, trata de sentar las bases que faciliten un manejo adecuado de la hipotermia accidental desde la primera asistencia prehospitalaria hasta tratamiento final hospitalario, incluyendo la reanimación y el recalentamiento con circulación extracorpórea.
The management of severe accidental hypothermia is not exclusive of rescue or urgent pre-hospital medicine but can also be extended to Critical Care Medicine and even heart surgery and extracorporeal circulation programs. In the event of accidental hypothermia it is essential to correctly select the victims who might benefit from transfer to a higher level hospital center. Wrong decisions at the time of first aid can subject the patient to long and unnecessary transfer to a hospital that may not have the technology best suited for the management of severe hypothermia. The International Commission for Mountain Emergency Medicine (ICAR MEDDCOM), the International Society for Mountain Medicine and Medical Commission and the International Mountaineering and Climbing Federation (UIAA MEDDCOM) have published consensus guides for the classification and pre-hospital management of severe hypothermia victims secondary to mountaineering accidents.1 The basic principles for the classification, resuscitation and management of accidental hypothermia victims are the same in the maritime, mountaineering and urban settings.2
DefinitionHypothermia is defined as a decrease in core body temperature (CBT) to below 35°C. The condition is classified as mild when CBT is between 35 and 32°C, moderate when between 32 and 30°C, and severe when under 30°C. Accidental hypothermia is turn refers to a spontaneous, unintended decrease in CBT generally occurring in a cold environment, associated to an acute problem of some kind, and without prior damage of the hypothalamus, which is where the body thermostat is located.
Physiopathological alterations (Table 1)Cold is the clear and fundamental cause of accidental hypothermia, though its pathogenic action depends on the intensity of cold, the duration of exposure, and the environmental conditions. The usual causal situation is immobilizing injury in a cold scenario, cold exposure without adequate protection, or immersion in cold water (Table 1).
The most common alterations in hypothermia.
| - Central nervous system: | - Endocrine: |
| • Progressively diminished consciousness (<32°C) | • Hyperglycemia |
| • Coma (from 28°C) | • Decreased hypophyseal hormones |
| • Respiratory center depression | - Renal: |
| • Cough reflex depression | • Pollakiuria |
| • Diminished EEG tracing amplitude (<32°C), | • Renal failure |
| • Flat EEG tracing (from 18°C) | - Hematological: |
| - Hemodynamic: | • Anemia/hemoconcentration |
| • Dehydration (cold diuresis) | • Thrombocytopenia |
| • Lowered cardiac output | • Disseminated intravascular coagulation |
| • Arterial hypotension, shock | - Gastrointestinal: |
| - ECG alterations: | • Pancreatitis |
| • J-wave (Osborn) (<31°C) | • Ileus |
| • ST alterations and prolonged QT | • Diminished liver activity |
| - Cardiac arrhythmias: | • Wischnevsky ulcers |
| • Sinus bradycardia | |
| • Atrial flutter and fibrillation | - Airway alterations: |
| • Idioventricular rhythm | • Initial hypersecretion due to cold |
| • Ventricular fibrillation and asystolia (<28°C) | • Posterior mucosal dryness |
| - Respiratory: | • Diminished vital capacity |
| • Initial tachypnea to bradypnea | • Diminished mucociliary activity |
| • Lowered tidal volume | • Atelectasis |
| • Alveolar hypoventilation | - Infections: |
| • Altered ventilation/perfusion | • Pneumonia |
| • Increased solubility of O2 and CO2 | • Sepsis |
| • Hypoxemia | - Vasoactive drug toxicity: |
| • Hypocapnia | • Alteration adrenergic receptors |
| - Metabolic: | • Altered drug clearance |
| • Reduction of oxygen consumption: 6% per 1°C decrease | - Vulnerability to freezing |
Thermoregulation is the balance between heat production (thermogenesis) and heat elimination (thermolysis). This active equilibrium, which keeps body temperature as close as possible to 37°C, allows the enzyme systems to function within a narrow optimum metabolic window or margin. In situations of mild hypothermia, the thermoregulatory mechanisms operate at a maximum in an attempt to combat heat loss, with trembling (shivering), cutaneous vasoconstriction, diminished peripheral perfusion, increased cerebral blood flow, increased diuresis (cold diuresis), increased heart rate, increased respiratory rate, increased cardiac output and increased blood pressure. If the condition of the victim worsens and the CBT drops to below 30–32°C, enzymatic activity is slowed, the capacity to generate heat decreases, the thermoregulatory system becomes exhausted, the functions of different body organs progressively decrease, and death ultimately results due to cardiorespiratory failure.3–7
Of the physiopathological alterations reflected in Table 1, four are particularly relevant:
- (1)
Ventricular fibrillation (VF) and asystolia may occur below a CBT of 28°C. However, some authors consider that asystolia does not usually manifest above 23°C, unless there is some other concomitant cause, and that asystolia presenting before the temperature drops to 23°C implies a poorer prognosis.8
- (2)
Inadequate patient management, e.g., involving sudden postural changes, can trigger ventricular fibrillation.
- (3)
At a temperature of 18°C the brain can tolerate periods of cardiac arrest 10 times longer than at 37°C.4
- (4)
Oxygen consumption decreases by 6% for every 1°C drop in CBT, and this reduction also affects the central nervous system (CNS) (brain and spinal cord). The decrease in oxygen consumption causes hypothermia to exert a preventive effect upon brain and spinal cord hypoxia, allowing complete neurological recovery after prolonged immersion in icy water, in serious head and spinal cord injury victims, or in cases of cardiorespiratory arrest.4,9,10
Until well into the 1980s, the “lethal triad” of hypothermia, acidosis and coagulopathy was considered to be the main cause of mortality in critical trauma patients. Even in urban settings, and logically conditioned to the climate and temperature, when the duration of transport to the nearest hospital is about 15min, close to 50% of all penetrating injury victims suffer hypothermia upon admission to the emergency room.11 According to different studies in trauma victims, the mortality rate among hypothermic versus normothermal patients increases up to 50%.12 Those particularly vulnerable are burn victims, patients with serious head injuries, or individuals with upper spinal cord injuries affecting the sympathetic chain. Age also exerts an influence, and in this sense vulnerability is greatest among the very young and the very old, due to their scant capacity to respond to body heat loss. Preventive measures to minimize heat loss and, where indicated, the start of active rewarming, are two key elements for good trauma victim management.13
Etiological classification of hypothermiaAcute hypothermiaIn acute hypothermia the exposure to cold is so great and sudden that the capacity of the body to resist cold is overwhelmed even though heat production is maximum or close to maximum. This situation is characteristic of people buried in snow avalanches or in cold water immersion victims. In those individuals who initially survive with effective thermoregulatory mechanisms, hypothermia takes about 30min in becoming established.14 The duration of survival depends on the balance among the efficacy of the thermoregulatory response, the insulation possibilities, clothing, and the environmental or water temperature.15
Subacute hypothermiaIn this case the critical factor is exhaustion and depletion of the body energy reserves leading to a drop in CBT. This situation is typically seen in hikers and mountain climbers. Since the condition is usually accompanied by hypovolemia secondary to fluid transfer among the different body compartments, rewarming measures should be associated to intravenous fluid administration.
Subchronic hypothermiaSubchronic hypothermia occurs when there is prolonged exposure to slight cold aggression and a thermoregulatory response that is insufficient to counter such aggression. The onset tends to be insidious and slow. The classical example is that of an elderly person lying immobile on the floor after a fall at home, with femoral neck fracture. Resuscitation is complex and implies important mortality, due to the existing hemodynamic instability, the typical comorbidities found in elderly people, and frequent complications in the form of respiratory tract infections and myocardial ischemia or ischemia of the extremities. Rewarming must be slow and careful in such weak victims.
Measurement of CBTIn first care it is essential to determine CBT using an epitympanic (ear) or esophageal thermometer allowing low temperature measurements.1 Esophageal temperature measurement is the most adequate and reliable option, however. Epitympanic measurements can give rise to false readings in certain circumstances such as very low external temperatures, blocking of the auditory canal with snow or water, and the absence of carotid flow (as in cardiac arrest). Epitympanic measurement can be useful in spontaneously breathing patients, but is categorically discarded in deceased subjects.3
Classification of hypothermia in first care and according to the clinical situationThe ICAR MEDDCOM and the UIAA MEDDCOM proposed a practical method based on the clinical signs and their relation to CBT. This classification, which could also be used by minimally trained, non-medical personnel, divides hypothermia into 5 grades1:
- •
Grade I: The victim is conscious and trembling (35–32°C).
- •
Grade II: The victim is drowsy and is not trembling (32–28°C).
- •
Grade III: The victim is unconscious but with positive vital signs (28–24°C).
- •
Grade IV: Absence of vital signs; apparent death (24–13.7°C?).
- •
Grade V: Death secondary to irreversible hypothermia (CBT<13°C).
Since there are severe hypothermia victims who have successfully recovered after several hours of asystolia10; since the lowest CBT resulting in recovery without neurological sequelae has been 13.7°C16; and since the rescue medical teams working “on the ground” may have doubts as to whether they are dealing with a grade IV victim with associated lesions but in a potentially reversible condition, or whether they are dealing with a grade V victim implying death due to irreversible hypothermia, the ICAR MEDDCOM and UIAA MEDDCOM consensus guide on accidental hypothermia contemplates a series of clinical data that allow us to differentiate between these two hypothermia grades and thus avoid futile resuscitation attempts. These data are summarized below1:
- (1)
The chest and abdomen are not compressible.
- (2)
The heart is permanently in asystolia (in grade IV there may be asystolia or VF).
- (3)
The core temperature is <13.7°C (?), this being the lowest CBT resulting in successful resuscitation recorded to date.16
- (4)
Serum potassium is >12mEq/l. This latter criterion is only applied in cases of hypothermia caused by asphyxia, as in avalanche or water immersion victims. In other etiologies of hypothermia with the associated possibility of hemolysis or rhabdomyolysis, as in polytraumatized patients for example, further studies are needed.
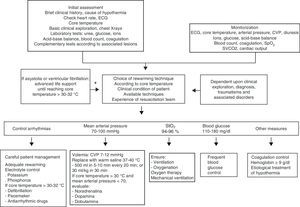
The general objectives of pre-hospital care are withdrawal and insulation from the cold environment, the prevention of a posterior drop in CBT (afterdrop), careful management of the victim and transfer to a hospital with the technological means required for treating this grade of hypothermia. As protection and insulation measures, and in addition to isolating the victim from the floor and affording protection from rain, wind or snow, it is useful to change wet clothes to dry clothes, cover the victim with a cap or hat, gloves, woolen blankets or sleeping or survival (bivouac) bag. The recommendations for management of the different grades of hypothermia are detailed below1,17 (Fig. 1).
Pre-hospital care algorithm for severe accidental hypothermia severe victims (up to grade IV). ECC, extracorporeal circulation; CPR, cardiopulmonary resuscitation; ALS, advanced life support; ICU, Intensive Care Unit.
Since in this scenario the patient is conscious and has mobility, we not only provide thermal protection and insulation but also encourage physical exercise, which warms faster than shivering alone (caution: this may produce CBT afterdrop). Hot beverages with sugar can be administered. Transfer to hospital is indicated only in the presence of comorbidity or suspected occult injuries.
Grade II (32–28°C)In this case shivering has been abolished and the patient is vulnerable to fatal arrhythmias (VF/ventricular tachycardia (VT) and asystolia), particularly when management is moreover inadequate (e.g., wet clothing should be removed by cutting, not pulling). If the level of consciousness is low, the patient should be placed in the horizontal position to avoid CBT afterdrop or peri-rescue collapse (see below). Rewarming should be started with the means available: warm and humidified air or oxygen therapy, warm water bags or chemically heated packs applied to the truncal arterial regions (neck, armpits, groin)—though always avoiding direct contact with the skin. If the nausea reflex is preserved and there is no risk of bronchoaspiration, hot beverages with sugar can be administered. Evacuation to hospital is indicated, with the possibility of intensive care.
Grade III (28–24°C)The victim shows diminished consciousness, with a high probability of fatal arrhythmias. Initial management should be very careful, with thermal protection and insulation, humidified and warm oxygen therapy (40–45°C), and monitorization of the ECG tracing and CBT. The triggering of VF as a result of the oxygenation and airway protection measures to prevent bronchoaspiration is considerably less likely than when tracheal intubation is attempted. This technique should only be performed where indicated according to the applicable advanced life support (ALS) algorithm, and when it can be maintained during transfer to hospital. If a venous line proves necessary (made difficult as a result of the peripheral vasoconstriction), it should be performed without causing a delay of over 5min—with due evaluation of the risk of a further drop in temperature, and avoiding central catheterization with access to cardiac cavities, due to the risk of triggering VF. The above mentioned rewarming and insulation measures should be adopted. Warm fluid therapy on the ground is scantly efficient, and only saline solution is indicated. As hypothermia progresses, the sodium levels tend to decrease while potassium increases, presumably due to a reduction in enzymatic activity of the cell membrane sodium–potassium pump. Evacuation should be carried out without delay to a hospital with the means needed for extracorporeal warming.
Grade IV (24–13.7°C?)In this situation the victim suffers severe hypothermia and appears to be dead. The absence of reflexes and pupil dilatation should not be regarded as signs of death: “nobody is dead without being warm and dead”. Cardiopulmonary resuscitation (CPR) is to be started immediately, with the condition that once started, CPR should not be interrupted until reaching the reference hospital center.18,19 As in the previous grades of hypothermia, the appropriate measures for avoiding posterior temperature drops should be adopted. These victims are to be transferred immediately to a third level hospital offering the possibility of rewarming with an extracorporeal circulation pump (ECP) or extracorporeal membrane oxygenation (ECMO). Initial transfer to a hospital without these options may waste crucial time for patient survival. In more isolated or remote scenarios with no third level hospital within range, use can be made of other management guides,20 or we can evaluate the possibility of evacuating the patient to the nearest hospital center with intensive care facilities and the possibility of continuous venous–venous hemofiltration and hemoperfusion (CVVHP).21
Assessment and resuscitation of snow avalanche victimsIn the mountain regions of Europe and North America, the practice of winter sports causes an average of 150 deaths each year due to snow avalanches. Such accidents tend to affect a number of victims and typically take place in areas that are difficult to reach by the rescue teams. Death is a result of asphyxia, trauma or accidental hypothermia. The above described classification of hypothermia and its treatment is closely related to people who have been buried by an avalanche and are in a situation of cardiorespiratory arrest.22
Three factors are implicated in patient classification and survival in cardiac arrest resulting from burial in a snow avalanche: the duration of burial in the snow, the presence or absence of a snow-free airway, and the CBT of the victim. Based on these three factors, and knowing that the cooling rate of an avalanche victim with a free airway is 3°C/h (after 90min buried in snow the CBT has dropped to 32°C), there are a number of individuals who cannot survive in the presence of cardiac arrest:
- (1)
Those buried for more than 35min and with airway obstruction at the time of extraction.
- (2)
Those buried for more than 35min, with a snow-obstructed airway and a CBT of ≤32°C.
- (3)
Buried victims with airway obstruction and initial serum potassium >12mmol/l.
In these three cases the death of the victim is certified at the site of the accident, in the same way as in the presence of fatal injuries. However, there are two additional situations where ALS maneuvering should be started, according to the current international recommendations, with transfer to a hospital center equipped with the means needed for intensive care and, where applicable, the start of rewarming1,17:
- (1)
Victims extracted within 35min or less. If no response is obtained following 20min of resuscitation, death as a result of asphyxia is certified.
- (2)
Victims buried for over 35min, with a CBT of ≤32°C (grade II or higher), and doubts as to obstruction or no obstruction of the airway.
The considerations referred to the rescue of snow avalanche victims are summarized in Table 2,23 and the assessment and treatment algorithm is shown in Fig. 2.22,24
Considerations referred to the rescue of snow avalanche victims.23
| 1. Do not rupture the breathing chamber. Only the rescue team should enter the avalanche zone in order to avoid stepping on the snow and rupturing the possible breathing chamber which the victim may have around the airway. |
| 2. Do not dig vertical. Digging should always be diagonal, from the valley side, and ensuring a cavity large enough to allow monitorization of the victim and the start of CPR. |
| 3. Whenever possible, a physician should be available at the time of extraction. The physician should assess the presence or absence of a breathing chamber. |
| 4. Careful management of the victim. Sudden movements can trigger VF or temperature afterdrop. |
| 5. An initial horizontal positioning of the patient prevents peri-rescue collapse. Posteriorly, if the hypothermia victim is unconscious and under spontaneous breathing, a lateral safety position may be adopted, except when spinal injuries are suspected. |
| 6. CPR started in patients with an extraction time of over 35min and without a permeable airway is pointless and poses an added risk for the rescue team. |
| 7. If the victim has a snow-free airway, CPR should not be interrupted until reaching hospital (nobody is dead without being warm and dead). |
Algorithm for the assessment and treatment of avalanche victims at the site of the accident.
Since the vital signs may be absent or undetectable in severe hypothermia (grade IV), they are of little use in certifying patient death. In these cases, where the pulse and breathing can be practically imperceptible and it is easy to make mistakes, most authors are of the opinion that the pulse is irrelevant in hypothermia,24 though some authors recommend large artery pulse palpation for at least 40s.25 Before concluding that cardiac arrest has occurred, it is advisable to monitor the ECG tracing for at least 1min. Cardiac monitorization is also essential to detect fatal arrhythmias. When the skin of the victim is extremely cold or damp, it may prove difficult to obtain an ECG tracing with adhesive electrodes. In such situations needle electrodes are advised.24 The current portable echocardiography or Doppler devices can be very useful for assessing the presence of cardiac output.
If cardiac arrest has been confirmed, or if there is no pulse, immediate CPR should be started, with a compression/ventilation ratio identical to that used in the resuscitation of normothermal patients, and provided the continuity of CPR can be guaranteed until reaching the hospital—particularly considering that the absence of a pulse does not necessarily imply cardiac arrest, and that CPR itself may trigger VF, as a result of which interruption would prove fatal for the patient. If necessary, orotracheal intubation is to be carried out, with mechanical ventilation adopting a protective ventilatory strategy [low positive end-expiratory pressure (PEEP) and tidal volume], or the administration of warm, lactate-free fluid therapy, since in the context of hypothermia the liver metabolization of lactic acid may be affected, thereby causing lactic acidosis.26 It has been shown that adrenalin improves coronary perfusion in asystolia due to hypothermia, though it was not found to improve survival in experimental studies in pigs.27,28 When the CBT does not exceed 30°C, adrenalin and other vasoactive drugs should be administered with great caution, since the adrenergic receptors respond poorly to low temperatures, and the reduction of vasoactive drug metabolism may give rise to potentially toxic concentrations when administered on a repeated basis. Amiodarone poses the same problems.29 When the CBT with rewarming exceeds 30°C, the intervals between successive drug doses should be doubled until the CBT is again close to normal. From this point onwards, the doses used can be those usually administered in resuscitation in general.
The rhythm disorders that appear in hypothermia, with the exception of fatal arrhythmias, tend to resolve spontaneously as the core temperature returns to normal. Sinus bradycardia can be regarded as physiological, and no pacemaker is needed unless the condition persists after rewarming. Although patient response to defibrillation is usually not seen until the CBT has exceeded 30°C, it can be attempted at lower temperatures and before reaching hospital. If defibrillation proves ineffective, no more than three discharges should be applied, and the technique should only be attempted again once the CBT has exceeded 30°C.30,31 In Spain, a case of VF reversion has recently been described with a CBT of 26°C.10
Effect of rewarming afterdrop and shockTemperature afterdrop refers to the additional decrease in CBT occurring once the patient has already been protected from the cold and rewarming has been started. This serious complication, which can trigger ventricular fibrillation,32 is related to peripheral vasodilatation, with the return of cold blood from the extremities towards the core blood circulation compartment,33–35 and active external rewarming. Other authors consider afterdrop to be a physical phenomenon not necessarily related to peripheral vasodilatation and attributable to the existing thermal gradient once cold exposure has ceased, between the peripheral compartment (skin and extremities), which is still cold, and the internal or core compartment (internal organs) which is warmer and transmits heat to the peripheral compartment.36 Rewarming shock or collapse is likewise observed during rewarming and related to the afterdrop effect; according to some authors, it is also related to active external rewarming and peripheral vasodilatation,37 while other investigators consider both phenomena to be independent of the form of rewarming involved.36
Peri-rescue collapsePeri-rescue collapse is generally associated to cases of hypothermia resulting from exposure to very cold water, in which the patient suffers clinical worsening after rescue and before rewarming is started (post-immersion collapse).38 Such hypovolemic shock may manifest after cessation of the hydrostatic pressure exerted by the water upon the body.39 There are examples of victims apparently stable and conscious after rescue who develop shock with symptoms ranging from syncope to VF and asystolia.40 There have been reports of deaths immediately before, during or immediately after rescue, and up to 24h afterwards.41–43 Since vertical extraction of the victim can increase this risk, due to losses and changes in the distribution of the body fluids,40 it can be prevented by keeping the patient in a horizontal position.
Insulation and rewarmingOnce insulation and protection against cold have been secured with the aforementioned measures, and without neglecting the possibility of afterdrop, rewarming can be started in the following forms:
- -
Endogenous rewarming: encouraging the patient to tremble or do exercise to generate warmth.
- -
Passive external rewarming: adequate for conscious victims, with mild hypothermia and who are able to shiver. Passive external rewarming raises CBT between 0.1 and 0.7°C/h, and is best achieved in a warm environment, covering the victim with woolen blankets, aluminum foil, a cap or hat (up to 50% of body heat can be lost from the head), etc.
- -
Active external rewarming: the most practical and easy method is to place warm water bags or chemically heated packs over the areas of the major vessels (neck, armpits, chest, abdomen and groin), avoiding direct contact with the skin (due to the risk of burns).44 Such measures are adequate for victims with moderate hypothermia, and raise the CBT between 1 and 2°C/h.
- -
Active internal rewarming: in victims with severe hypothermia but preserving an active cardiac rhythm we can infuse warm intravenous fluids, administer warm and humidified oxygen for breathing,45,46 or use warm saline solution to irrigate the organic cavities such as the stomach, pleural space, peritoneum, colon and/or bladder cavity. This technique is able to raise the CBT between 1 and 7°C/h. In victims under cardiac arrest, rewarming should be carried out via extracorporeal circulation—this being a more aggressive and invasive method than the above techniques, and which will be commented further below. The CBT is raised between 8 and 12°C/h in this case.
Active rewarming should not be started before the victim has been rescued, insulated and protected from the cold, and has been moved to a safe place under control, provided the means are available, pre-hospital care can include endogenous rewarming and passive and/or external rewarming, with due CBT monitorization in all cases. Pre-hospital internal rewarming with warm fluid therapy and humidified gases can also be used but is not particularly efficient. In the case of pre-hospital rewarming, two specific methods should be considered:
- (1)
The so-called “arteriovenous shunt technique”. This facilitates active external rewarming and can be applied in a base camp, mountain refuge or onboard a ship. The arms and/or legs of the victim are immersed in water at temperature of 42–45°C, resulting in rewarming at a mean rate of 6.1°C and 9.9°C/h, respectively.47,48 Such rewarming is possible because the arteriovenous anastomoses of the hands and feet act as heat exchangers.
- (2)
As an alternative to the administration of warm and humidified air or oxygen, many mountain rescue teams are equipped with an active internal rewarming system known as a “little dragon” or “thermal parachute”. This is a cylinder weighing 2.2kg capable of warming air or oxygen taken from the exterior and administered to the patient through a connected face mask. Rewarming is achieved thanks to a chemical reaction taking place within the cylinder between carbon dioxide and medical-grade caustic soda. The system is also available in a non-caustic version. It is able to warm the air/oxygen passing through the cylinder for 5h, at a temperature of 40–50°C, and to humidify oxygen at a rate of up to 10lpm.21
The hospital management of hypothermia constitutes the third and last link in the patient care chain, which starts with first care (extraction, evaluation, protection, resuscitation), is followed by a second care step (vigilance, rewarming, resuscitation, transfer), and ends with patient arrival and admission to hospital.
Once the patient arrives in hospital, and depending on the grade of hypothermia, admission to the Emergency Department or to Intensive Care is decided (Fig. 3).49 The general measures applied to all such victims admitted to hospital are the following:
- (1)
Initial evaluation and compilation of the case history, including the aspects most relevant to the antecedents and etiology of the accident.
- (2)
Exclusion of other causes of cardiac arrest such as alcohol, pharmacological or drugs of abuse overdose, and other reversible causes, using the four Hs and Ts approach of the advanced life support (ALS) algorithm.50
- (3)
Monitorization of the main vital signs, including CBT, which is also essential for assessing the effectiveness of rewarming. Oxygen saturation measured by pulsioxymetry is usually not useful, due to the intense peripheral vasoconstriction seen in hypothermia victims.
- (4)
Continuous ECG monitorization for the detection of arrhythmias.
- (5)
Pertinent biochemical and hematological tests.
- (6)
Monitorization involving catheters inserted in the right-side cavities (e.g., Swan-Ganz catheters) should be avoided, since such devices are able to induce serious arrhythmias.
- (7)
Initial volume replacement using lactate-free crystalloids. The monitorization of urine output and central venous pressure is very useful for assessing volume replacement.
- (8)
During rewarming, the victims require large volumes of warm fluids, since vasodilatation causes expansion of the intravascular space.
Algorithm for the management of hypothermia victims in a hospital with intensive care facilities.49 ECP, extracorporeal circulation pump; ECMO, extracorporeal membrane oxygenation; CVVHP, continuous venous–venous hemofiltration and hemoperfusion.
This initial intervention and posterior patient management (Fig. 4) do not differ much from the algorithm proposed by the Steering Committee of the National CPR Plan of the SEMICYUC as a protocol for the objectives-oriented optimization of the management of post-cardiac arrest syndrome.51 During rewarming it is necessary to take the following into account:
- (1)
Metabolic and water-electrolyte corrections should be carried out parallel to volume replacement.
- (2)
The initial hyperglycemia does not require insulin use for correction. It usually normalizes during rewarming as the energy requirements increase and pancreatic insulin secretion normalizes. It is advisable to maintain a tolerable level of hyperglycemia, between 110 and 180mg/dl, in order to avoid hypoglycemia.
- (3)
Hypopotassemia and hypophosphatemia can cause serious complications during rewarming.
- (4)
The hypothalamus–hypophyseal dysfunction produced by the generalized slowing of enzyme activity requires no replacement therapy (including corticosteroids).
- (5)
The prophylactic use of antibiotics to prevent lung infections is not indicated. The victims of avalanches or aquatic accidents that have been immersed in snow or cold water but have survived are at a high risk of suffering respiratory complications.52
- (6)
Cardiovascular stability is only established once the CBT no longer decreases and rewarming has started. As has been commented above, vasoactive drugs and antiarrhythmic agents should not be used with low CBT values, and any such a use requires extreme caution.
- (7)
The hypothermic heart does not easily respond to atropine, defibrillation or pacemaker implantation. Although defibrillation is usually not effective until the CBT has exceeded 30°C, there has been a report of successful defibrillation at a CBT of 20.4°C.53
- (8)
As the CBT decreases, an increase is seen in the blood solubility of CO2 and in the pH value. Blood gas analyzers are usually programmed for a CBT of 37–38°C, and if the actual CBT values of the patient are not entered, the values obtained will not reflect the true situation. Theoretically, for every 1°C of temperature below 37°C, the pH value increases by 0.0147, PaO2 decreases 7.2% and PaCO2 decreases 4.4%.5 This means that after correction we can obtain very low PaO2 values (25mmHg).3,9 The important consideration is not so much the correction of values but the performance of serial controls during rewarming, and the comparison of results.
- (9)
Oxygen consumption increases greatly during rewarming. In this context oxygenation is to be monitored, oxygen should be administered according to need, and mechanical ventilation should be introduced if required. Hypocapnia is frequently seen in patients subjected to mechanical ventilation.
- (10)
The maintenance of moderate metabolic acidosis is recommended, with a pH value of about 7.25, to compensate for the left shift induced by hypothermia and facilitate oxygen uptake and release at tissue level.
- (11)
Reductions in hematocrit should be monitored in hypothermia victims with associated traumatisms.
- (12)
Coagulation alterations are to be monitored: thrombocytopenia, platelet dysfunction, prolonged clotting time due to alteration of the extrinsic coagulation pathway, and disseminated intravascular coagulation.6,7
- (13)
Neither the method nor the rate of rewarming is dependent upon the patient CBT. The decision should be based on the presence or absence of a cardiac rhythm and its influence upon cardiac output and peripheral perfusion.
- (14)
After rewarming with peritoneal lavage, there have been reports of fatal mesenteric ischemia caused by the difference in gradients between the cold blood of the mesenteric circulation and the warm saline of the peritoneal lavage. Such situations have caused the technique to be questioned. However, these problems have also been described as middle-term complications of the extracorporeal circulation rewarming of severe hypothermia patients.54
- (15)
In the presence of severe hypothermia, where the priority concern is to restore an effective cardiac rhythm as quickly as possible, the techniques guaranteeing faster rewarming are the extracorporeal approaches such as ECP and ECMO. A hospital lacking these techniques but with a critical care unit could resort to continuous venous–venous hemofiltration and hemoperfusion (CVVHP).55,56 Promoting the latter technique in second level hospitals or centers with critical care units would offer an alternative in the organization of the management of accidental hypothermia victims and could obviate the need for transfer to a third level hospital equipped with ECP and/or ECMO, which possibly would take longer and prove more costly. The two additional advantages of CVVHP are the following:
The technique is more accessible, less costly and very probably closer to the accident site than ECP or ECMO found in third level centers—though according to some authors CVVHP has not been as effective in victims with asystolia or ventricular fibrillation.
- •
This system has the added advantage that the circuit can be operated without heparin; as a result, it can be useful in application to victims with traumatisms contraindicating rewarming with ECP or ECMO.
Extracorporeal rewarming is the technique affording the fastest recovery of patient CBT (up to 10°C/h). According to many authors, it is the best option for rewarming patients under cardiac arrest.57–60 Extracorporeal rewarming can resuscitate hypothermia victims with complete neurological recovery and no ulterior sequelae, even after 2h of asystolia—though such full recovery has also been possible in longer cardiac arrests without such invasive techniques.10 According to these authors, the use of such an invasive technique implies an important delay in the start of treatment. One of the largest studies published to date found the delay associated with these rewarming procedures to be 141±50min.57 The survival rate among those patients without asphyxia prior to hypothermia can reach 64%, though the prognosis is much poorer when asphyxia effectively precedes hypothermia, as in immersion or avalanche victims.61
The rewarming rate depends on the relationship between the temperature of the blood and the flow allowed by the extracorporeal pump. High temperature gradients between the blood within the circuit and the patient CBT are related to a poorer neurological prognosis.62 Normally the pump is operated with a circuit/patient temperature gradient of between 5 and 10°C, which allows internal and external rewarming and at the same time minimizes the afterdrop effect. Temperatures in excess of 40°C can cause denaturalization of the blood cellular and humoral components.
As has been commented, during the rewarming of victims subjected to mechanical ventilation, respiratory alkalosis due to hypocapnia is observed, more or less altered by other variables such as previous metabolic acidosis. There is ongoing debate over the best way to manage pH and patient ventilation under these circumstances. Management in “pH-stat” form keeps the pH value stable by supplying extra CO2 to ventilation of the patient. Management in “alpha-stat” form in turn is based on lowering ventilation to keep the pH stable at 7.40. The experts recommend this latter approach.57–61
Extracorporeal rewarming techniques in hypothermia victims49The indications of extracorporeal rewarming techniques can be applied to: (1) victims with positive and sufficient cardiac output; and (2) victims with inexistent or insufficient cardiac output.
Victims with sufficient cardiac outputVenous–venous rewarming circuitThis system consists of a simple circuit with a tubing element, a centrifuge pump and a heat exchanger. The fact that it is able to operate without heparin favors the rewarming of trauma victims.63 Access is via the percutaneous route, preferably the femoral vein.
Continuous venous–venous hemofiltrationThis system is similar to that described above, but with the possibility of offering dialysis. The maximum flow capacity of 500ml/min limits the rewarming potential.
Both systems can be used in victims in asystolia, provided that ALS is not interrupted. The recovery of CBT can be very slow, because during rewarming, and in order not to alter the balance between oxygen supply and tissue oxygen consumption, cardiac output cannot be higher than that obtained with external cardiac massage (approximately 20% of normal).56
Victims in asystolia or ventricular fibrillationExtracorporeal circulation pump (ECP)The ECP is the system classically used in heart surgery units, and is useful for patients weighing over 40kg. Pediatric systems are used in the event of patients of lesser body weight. The flows that ensure the best support of gas exchange and cardiac output are 2.4l/m2/min and above. The system consists of a vena cava-aorta circuit, a venous reservoir, a pump impelling the blood towards the membrane oxygenator, a heat exchanger, and an impurities filter before returning to the aorta. The system also has a suction function that returns lost blood to the vascular bed. Since zones of blood stasis are found within the circuit and full heparinization is required (3mg/kg/h), the technique is contraindicated in severe trauma patients, particularly those with head injuries. The heparin must be antagonized once the ECP has been disconnected.
In addition to a perfusionist, management of the system requires a surgical team specialized in cava-aorta cannulation through the midline sternotomy approach. This technique, by allowing direct decompression of the left ventricle, often achieves spontaneous VF reversion to sinus rhythm. Sternotomy is also preferred in small children. The femoral vessels are of little use in these subjects because of their limited caliber, and jugular-carotid cannulation increases the risk of brain damage.64 In older children or in adults, femoral vessel cannulation is possible.65
Extracorporeal membrane oxygenation (ECMO)ECMO involves technology similar to that of ECP. It is also used in intensive care medicine to provide prolonged cardiorespiratory support. Its advantages over ECP in relation to rewarming are:
- •
The fact that the circuit lacks a venous reservoir and suction system means that it allows anticoagulation far lower than that required in ECP (0.3–0.6mg/kg/h). Indeed, in the presence of traumatisms or signs of bleeding, ECMO can be used with heparin microdoses (0.1mg/kg/h). The current ECMO systems are made of polymethyl pentenes (PMP) coated with heparin, and can be used for short periods of time without intravenous heparin.63 In addition, the systemic inflammatory response is far lower than in the case of ECP.66 Since there are no bubble traps, air must not be allowed to enter the circuit, in order to prevent neurological damage.
- •
Since the prolonged administration of supplementary oxygen is allowed, in cases of severe respiratory failure the system may be very useful for rewarming patients with associated chest injuries, lung damage or severe respiratory failure secondary to immersion.
- •
In victims in asystolia or VF, the usual practice is to connect the system through the femoral artery-vein, using long cannulas to secure a sufficient flow. Venous–venous connection is also possible provided cardiac massage is maintained.60 Transthoracic cannulation is preferred in small children.
Since both ECP and ECMO favor rapid rewarming, if VF fails to revert with cardiac decompression, defibrillation may be attempted. The latter in turn should not be repeated until the CBT reaches 30°C. If after defibrillation at 30°C ventricular fibrillation is seen to persist, the administration of magnesium or amiodarone may facilitate cardioversion.
Post-resuscitation care- -
Hyperthermia should be avoided during and after rewarming.
- -
Post-resuscitation care should be continued after rewarming has been achieved, including the maintenance of mild hypothermia if necessary.51
- 1.
International Commission for Mountain Emergency Medicine: www.ikar-cisa.org. Access confirmed in November 2011.
- 2.
International Society for Mountain Medicine: http://www.ismmed.org. Access confirmed in November 2011.
- 3.
Medical Commission of the International Mountaineering and Climbing Federation: http://www.theuiaa.org/medical.html. Access confirmed in November 2011.
The authors declare no conflicts of interest.
Please cite this article as: Avellanas ML, et al. Manejo de la hipotermia accidental severa. Med Intensiva. 2012;36:200–12.