Before deciding increases in the number or capacitance of Intensive Care Units (ICUs), or the regionalization of Units, it is essential to know their present effectiveness.
ObjectiveTo analyze the daily occupancy rate of ICUs in Catalonia (Spain) and the frequency of denied admission due to lack of capacity.
DesignA prospective, observational multicenter study was carried out.
ParticipantsA total of 35 out of 40 ICUs of Catalonia (87%).
InterventionsDaily registry.
Variables of interestOpen beds and free beds, patients not discharged due to unavailability of ward beds, critically ill patients not admitted due to a lack of ICU beds, and rate of transfer to other ICUs.
Statistical analysisA descriptive cohort analysis was made.
ResultsDaily averages were 383 open ICU beds, 58 available beds (15%), and 16 patients not discharged due to unavailability of ward beds. Each day 6 patients on an average were not admitted due to a lack of ICU beds, and one of them (16%) was transferred to another ICU. The mean occupancy rate was 83±19%, and a 100% occupancy rate was reported in 35% of the registries. A subanalysis of the 24 public hospitals demonstrated slightly higher occupancy (87±16%), with a 100% occupancy rate reported in 38% of the registries.
ConclusionsThe mean occupancy rate of Catalonian ICUs may appear correct, but in some Units over-occupancy very often precludes early ICU treatment and even ICU admission for a significant number of critically ill patients.
Ante la demanda por aumentar el número de UCI o su capacidad, o por regionalizar servicios, es conveniente conocer su efectividad actual.
ObjetivoAnalizar la ocupación diaria de los Servicios de Medicina Intensiva (SMI) de Catalunya y con qué frecuencia pacientes críticos no pueden ingresar en UCI y/o son derivados a otros centros.
DiseñoProspectivo observacional multicéntrico.
ParticipantesTreinta y cinco de los 40 (87%) SMI de Catalunya.
IntervencionesRegistro diario.
Variables de interésCamas abiertas y camas libres, pacientes no altados de UCI por falta de camas en planta, pacientes críticos no ingresados en UCI por falta de cama y cuántos fueron derivados a otros centros. El análisis estadístico es descriptivo de cohortes.
ResultadosLos promedios diarios fueron: 383 camas de UCI abiertas, 58 (15%) camas libres y 16 pacientes no dados de alta por falta de cama en planta. Cada día 6 pacientes en promedio no ingresaron en UCI por falta de camas y uno (16%) fue derivado a otras UCI. La ocupación media fue del 83±19% con un 100% de ocupación en el 35% de los registros. El subanálisis de los 24 hospitales públicos mostró una ocupación ligeramente superior (87±16%) con 100% de ocupación en el 38% de los registros.
ConclusionesLa ocupación media de las UCI de Catalunya podría parecer correcta, pero existe sobresaturación muy frecuentemente en ciertas unidades lo que dificulta el ingreso precoz y además provoca que una cantidad significativa de pacientes críticos no puedan ingresar en UCI.
Intensive Care Medicine is facing great challenges as a result of the increase in life expectancy and the widespread use of more aggressive treatments with increasingly effective life support systems. There is no doubt about the social benefits of critical patient care in terms of survival and cost-effectiveness,1 though it is also true that such care implies an exponential increase in associated economic costs for society as a whole.
There is little information in the literature on the real and/or perceived effect of the limitation of technical and human resources in critical care,2 and certainly no recent data have been published in this regard during the current economic crisis. The imbalance between the needs of critically ill patients and the means available to cover such needs is basically a consequence of delays in patient admission to the Intensive Care Unit (ICU) or the impossibility of admission to the ICU.
Regarding delays in patient admission, there are sufficient references to the benefits of early treatment in a range of scenarios (sepsis, acute myocardial infarction, stroke, etc.), and in this respect mobile critical care teams have been created that take professionals not only to the emergency care room or hospital ward,3 but even to the home of the patient. It has also been shown that each hour of delay in admission to the ICU is associated to a decrease in patient life expectancy.4
Likewise, admission denial has been shown to have a negative impact upon patient survival,5,6 and in this regard a lack of free beds is one of the permanent factors underlying the decision not to admit a patient to the ICU.7
On the other hand, the limitation of economic and human resources prevents the unlimited expansion of critical care. In this respect, before deciding increases in the number and capacitance of ICUs or the regionalization of such Units,8–10 it is necessary to know the current distribution of the available means and their effectiveness.
The present study was carried out to analyze the daily occupancy rate of ICUs in Catalonia (Spain) and the frequency of denied admission due to lack of capacity, and/or referral to other centers.
Material and methodsThe study was carried out during 30 days (from 12 November to 12 December 2012) in the 35 out of 40 (87%) Departments of Intensive Care Medicine (DICMs) in Catalonia (Annex 1) that agreed to participate. Given the observational nature of the study, patient informed consent was not required.
Each DICM used a web form (Google docs) to register the following variables every morning (8a.m.): number of open beds; number of free beds; number of patients not discharged from the UCI due to a lack of ward beds the day before; critically ill patients not admitted due to a lack of beds in the ICU in the last 24h; and the number of such patients referred to other centers. In order to determine the real availability of admission to the ICU, we subtracted the number of beds already reserved for scheduled admissions from the calculated number of free beds.
A simple cohort analysis was made, reporting the quantitative variables as the mean±deviation, or as the median and interquartile range, where applicable.
ResultsAll the participating ICUs were polyvalent Units, with the exception of a single purely surgical ICU. Twelve ICUs (34%) belonged to third-level hospital centers, 20 (57%) to second-level hospitals, and three (9%) corresponded to first-level centers. We obtained 1085 out of 1116 expectable registries, i.e., the compliance rate was 97%.
The daily averages in intensive care were: 383 open beds, 58 free beds and 16 beds occupied by patients not discharged due to a lack of available ward beds. An average of 6 patients could not be admitted each day to the UCI because of a lack of beds, and of these only one (16%) was transferred to another ICU. According to the type of center, the 24 public hospitals contributed 277 beds (72%), with an average of 12 beds per Unit, while the 11 private centers contributed 106 beds (28%), with an average of 10 beds per Unit.
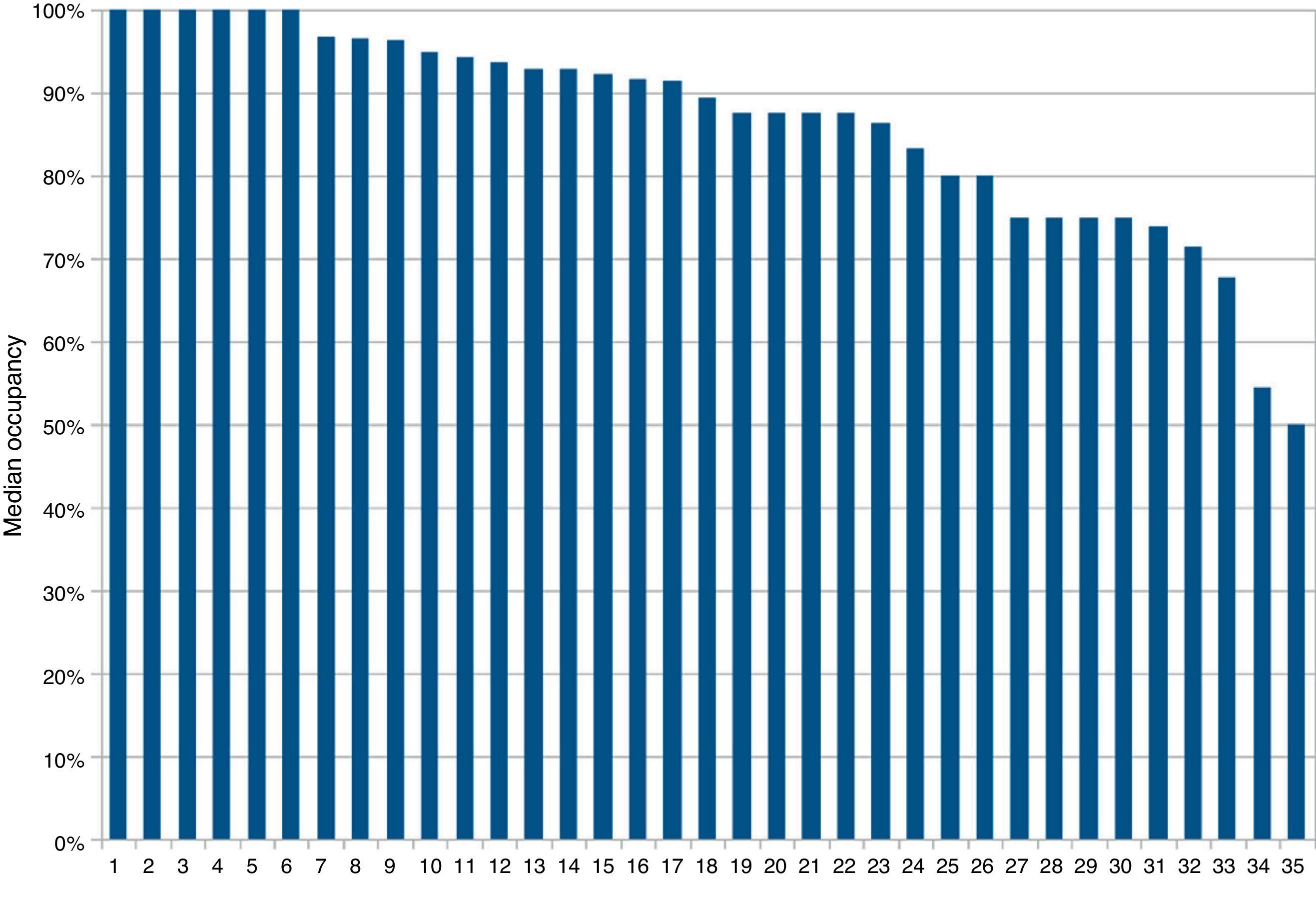
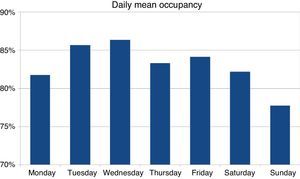
The mean occupancy rate was 83±19%, and a 100% occupancy rate was reported in 35% of the registries. By hospitals, we found that 6 DICMs (17%) had a median occupancy rate of 100%, which means that immediate admission of critical patients was not possible on one-half or more of the days. Considering that an occupancy rate of over 90% also complicates optimum patient flow, we observed that another 11 DICMs (31%) had a median occupancy rate of between 90 and 100% (Fig. 1).
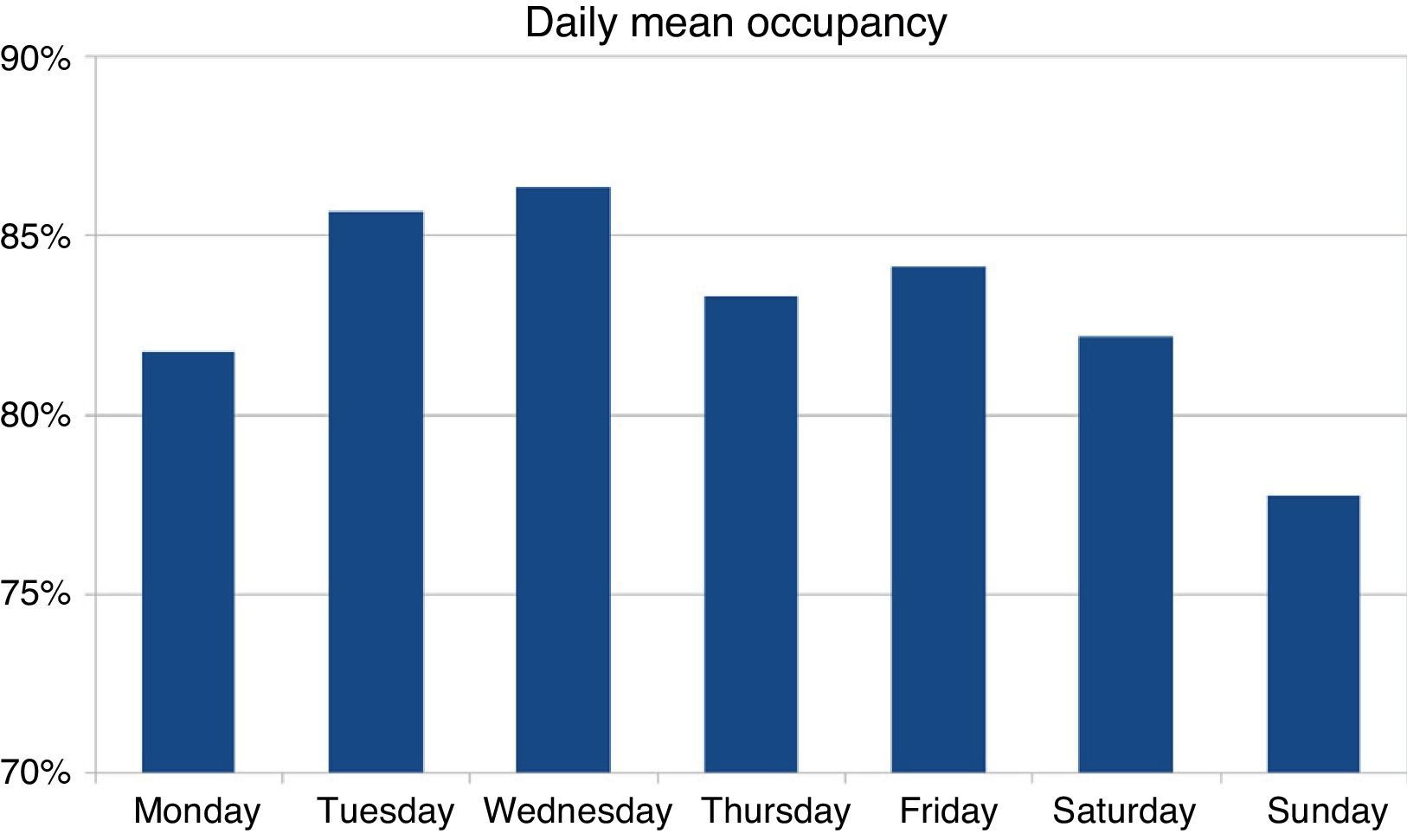
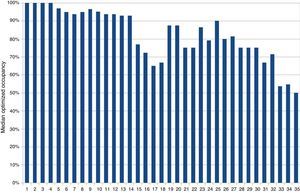
The analysis by day of the week revealed a moderately heterogeneous distribution, with maximum occupancy on Wednesday (86±17%) and minimum occupancy on Sunday (78±22%) (Fig. 2).
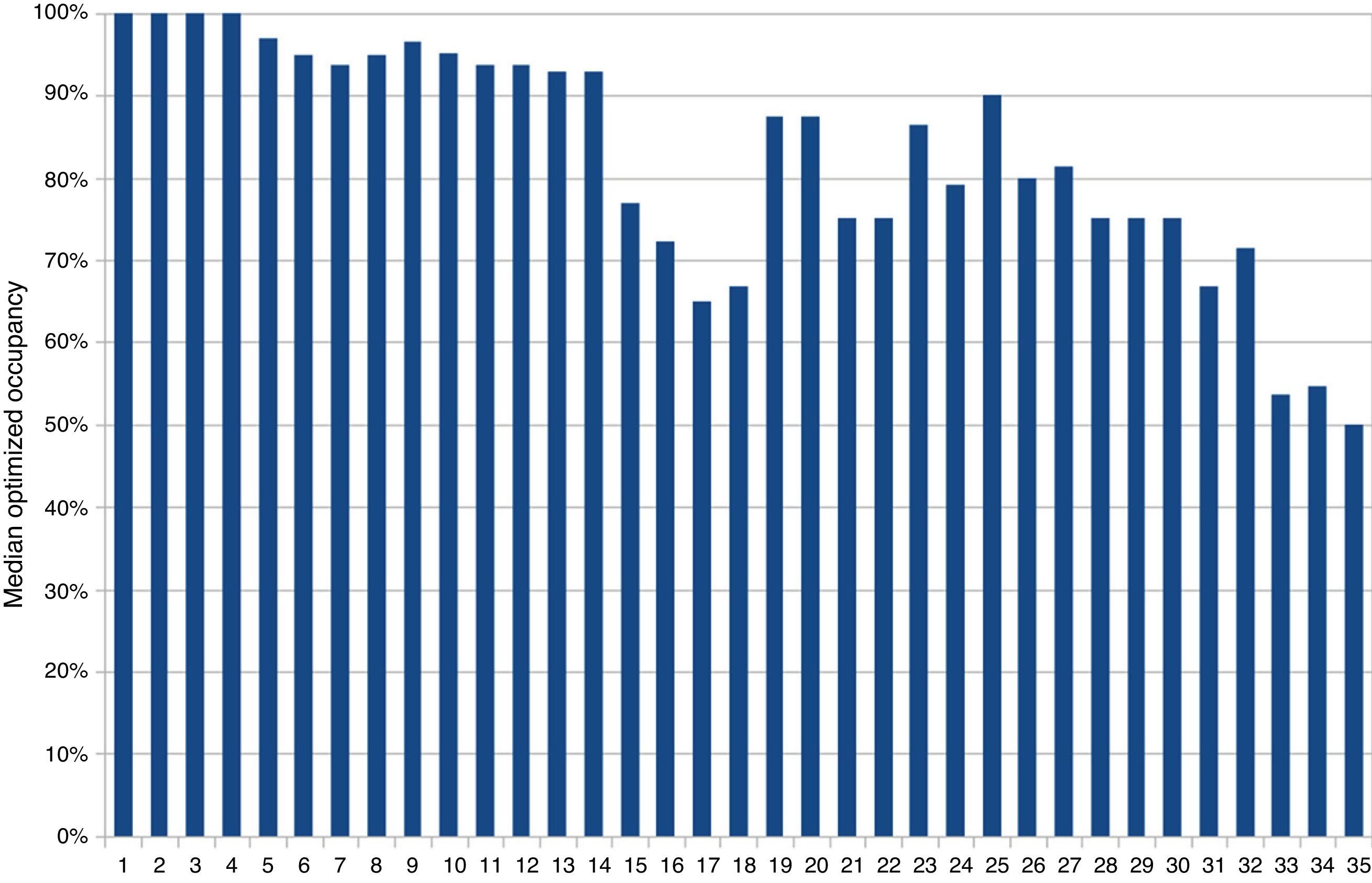
If ward beds had been available for all the patients with conditions for discharge, the mean occupancy rate would have dropped to 79%, and the number of registries reflecting 100% occupancy would have decreased from 35% to 27%. However, this effect was likewise not homogeneous. Of the 6 centers with a median occupancy of 100%, four would remain in the same situation due to a lack of patients with conditions for discharge, while two would have been able to lower occupancy to 95%. We also recorded hospitals with occupancy rates between 90 and 99% that would not experience changes, while others would be able to lower occupancy to 60% (Fig. 3).
The sub-analysis according to the type of center showed the 24 public hospitals to have a slightly higher mean occupancy rate (87±16%), and 38% of the registries revealed 100% occupancy, while the 11 private centers had a mean occupancy rate of 76±12%, and 27% of the registries revealed 100% occupancy.
The sub-analysis according to hospital complexity showed trends that failed to reach statistical significance, probably because of the limited sample size. The mean of the median occupancy rate was 93%, 85% and 70% in the case of third-, second- and first-level hospital centers, respectively. In other words, the frequency with which a median occupancy of 100% was reported was 25% and 15% in the third- and second-level hospital centers, respectively, while none of the three first-level centers reported such occupancy. After adjusting for the patients who could have been moved to the hospital ward, the optimized occupancy that continued to be 100% exhibited the same trend (17% in third-level centers and 10% in second-level centers).
DiscussionThis regional study for the first time describes the magnitude of the over-occupancy found in certain DICMs, and its impact in terms of critically ill patients who cannot be admitted to intensive care.
Some aspects of the study deserve closer examination.
Although the results come close to describing the situation in a global region (Catalonia), it must be underscored that 13% of the DICMs did not participate in the study, and some of them have a very large number of admissions.11 Nevertheless, indirect sources show that these DICMs usually have very high occupancy rates; the overall conclusions of our study therefore probably would not have changed had they been included in the analysis. On the other hand, the methods used to register occupancy probably differ greatly, since at Spanish national level the document “Statistics of healthcare centers with patient admission, 2012” (“Estadística de establecimientos sanitarios con regimen de internado, 2012”)12 indicates that there are 3463 polyvalent ICU beds in public centers and 823 in private centers in the country, with a mean occupancy rate of 65% and 45%, respectively.
The time frame of the study also deserves mention, since it covered a single month and involved a period which a priori would not be expected to be particularly biased by either an excess of patients in the winter months or a decrease in patients in summer. Nevertheless, precisely because of this, the findings of our study cannot be extrapolated to other time frames in which the offer and demand might be very different.
Our description of occupancy is referred to a concrete time of day, coinciding with the end of the duty shift and the start of routine daily activity. Occupancy therefore might differ in the course of the day depending on the admissions and discharges that have occurred.13 The ESICM Working Group on Quality improvement14 found the percentage of ICU beds with respect to total hospital beds in Europe to be between 5 and 10%, depending on the complexity (level) of the center. The corresponding percentage is higher in the United States. Regarding occupancy, a standard of 75% has been defined (calculated in hours) in order to allow sufficient margin for the management of emergencies.
The negative consequences for critical patients of non-admission to the ICU are well known.15,16 However, our study does not address the possible deleterious effects of ICU over-occupancy, causing hours of delay in treating certain patients, even if the latter are finally admitted to the Unit. In this regard, each hour of delay in being admitted to the ICU has been estimated to result in a 1.5% increase in mortality risk.4
In our study, the point frequency of patients not discharged from intensive care due to a lack of hospital ward beds was 4%. Compared with the standard 9% defined as quality indicator by the SEMICYUC,17 our figure could be regarded as good. However, this statistic also coincides with a significant number of patients who could not be admitted to the ICU–with the resulting deleterious consequences. The mentioned indicator therefore reflects the negative impact of the percentage of patients not discharged to ward beds, associated to the percentage of critical patients who cannot be admitted to intensive care. Likewise, the impact of the patients not discharged was not homogeneous, and it was precisely in the DICMs characterized by 100% occupancy where this circumstance proved least relevant. In a sense, the results obtained suggest that a delay in discharge to the hospital ward is more tolerated in those Units that still have free beds, and is much less tolerated in those with maximum occupancy.18,19
The measures adopted with patients who could not be admitted to the ICU because of a lack of free beds also deserves mention, since only one out of every 6 such individuals was finally transferred to another ICU. We have no data on the severity of the condition of these patients, and do not know whether they required intensive care or only monitoring. Balancing the expected benefit in a remote UCI against the inherent risk of patient transfer remains subject to controversy. Critical patients transferred to regional centers have greater mortality,8,9 though this fact is probably conditioned by delays in admission and/or a lack of optimum previous care.3 On the other hand, there are saturated third-level hospital ICUs that do not contemplate the possibility of critical patient transfer to other Units. In this respect, a coordinating center would be needed to seek the best critical patient allocation in each case, based on the existing availability.
A limitation of our study is the fact that we cannot determine whether the differences in ICU occupancy are due to an inadequate territorial distribution of ICU beds or types of hospital, or to differences in management (reduction of sedation, early mobilization, lesser incidence of nosocomial infections, etc.) that might account for very different mean stays for one same case-mix and a greater availability of free beds. We likewise cannot gain deeper insight to the reasons for the apparently greater congestion seen in more complex hospital centers. On one hand, such hospitals usually have a larger ICU, which should permit greater internal adjustments–though it is also possible that such Units must accept a larger number of complex surgery patients or act as obligate reference Units for other peripheral hospital centers. In any case, the estimated impact of collapse due to a lack of discharge to hospital wards was seen to be of similar magnitude in both the third- and second-level centers.
Another limitation of our study is that no in-depth analysis could be made of the clinical impact of ICU collapse, since we do not know whether such collapse resulted in the cancelation of scheduled surgeries or high-risk procedures. We likewise were not able to follow-up on the patients who could not enter the ICU, and do not know whether the patients finally transferred to other ICUs suffered negative consequences because of the delay or due to transfer itself. Our community is characterized by a centralized critical patient coordinating system that allows us to ensure specialized patient care during transfer. The hospital network allows access to an ICU in under one hour in the worst of cases. However, it must be taken into account that most third-level hospitals are concentrated in the area of Barcelona, which may cause transfer to take up to two hours from the most peripheral areas.
On the other hand, we did not register whether the hospitals with the greatest problems of collapse decided early discharges or nocturnal discharges, which some authors have associated to poorer outcomes.20
The different occupation level of DICMs according to the day of the week is also a novel aspect. It is probably conditioned to the perception of the professionals and may contribute to coordination with other services. On one hand, there is a group characterized by critical patients scheduled for complex surgery, etc., which is not performed on weekends–though even such cases are rarely scheduled according to the anticipated availability of free beds in the ICU.
In conclusion, the mean occupancy rate of Catalonian ICUs may appear correct, but in some Units over-occupancy very often precludes early ICU treatment and even ICU admission for a significant number of critically ill patients.
Financial supportNone.
Conflicts of interestNone.
H. Clínic Barcelona, AVI (Josep M. Nicolas).
H. Clínic Barcelona, UCI Quirúrgica Anestesiología y Reanimación. IDIBAPS (Elizabeth Zavala and Jordi Mercadal).
H. U. Germans Trias i Pujol (Jordi Klamburg).
H. U. de Girona Dr. Josep Trueta (Josep M. Sirvent).
H. Sant Pau i Santa Tecla. Tarragona (Fernanda Bodí).
H. U. de Tarragona Joan XXIII. UCI (Maria A. Bodí).
H. U. de Tarragona Joan XXIII, Semicríticos (Monica Magret).
Consorci Hospitalari de Vic (Jose Luis Lopera).
H. Sant Pau, Servei de Medicina Intensiva (Jordi Mancebo).
H. General de Catalunya (Francisco Baigorri and Sandra Barbadillo).
H. U. Arnau de Vilanova (Angel Rodriguez).
Clínica Sagrada Familia (Lluis Asmarats).
H. de Barcelona (Lluis Cabre).
H. del Mar (Jose Felipe Solsona).
H. de Mataró (Juan Carlos Yebenes).
H. de Granollers (Pau Garro).
H. de Terrassa (Joaquin Amador).
H. de Igualada (Montserrat Casanovas).
H. Verge de la Cinta de Tortosa (Gaspar Masdeu).
H. General de Hospitalet (Josep Masip).
H. de Sabadell, UCI (Antonio Artigas).
H. de Sabadell, Semicríticos (Gemma Goma).
H. Santa Maria de Lleida (J. Falip).
Fundació Althaia Manresa (Rafael Fernandez).
Clinica del Pilar-Sant Jordi (Mauricio Valencia).
H. U. Mutua de Terrassa (Ricard Ferrer).
H. Sant Joan de Reus (Inmaculada Vallverdu).
Institut U. Dexeus (Carme Cambray).
Clínica del Remei (Carles Triginer).
H. Moises Broggi (Josep Masip).
H. Sagrat Cor (Javier Ruiz).
H. San Camil (Rosa M. Díaz Boladera).
Clínica Corachan (Dolors Garcia).
Centre Mèdic Delfos (Francisco Fernandez).
Clínica de Ponent (Teresa Farre and Carme Barberà).
Please cite this article as: Fernandez R, por el Grupo de Trabajo de Gestión Clínica de la Societat Catalana de Medicina Intensiva i Crítica. Ocupación de los Servicios de Medicina Intensiva de Catalunya: un estudio analítico prospectivo de cohortes. Med Intensiva. 2015;39:537–542.
Presented as a communication at the XLVIII National Congress of the SEMICYUC. Tenerife, 9–12 June 2013.