To analyze if the implementation of a multidisciplinary extracorporeal cardiopulmonary resuscitation (ECPR) program in a tertiary hospital in Spain is feasible and could yield survival outcomes similar to international published experiences.
DesignRetrospective observational cohort study.
SettingOne tertiary referral university hospital in Spain.
PatientsAll adult patients receiving ECPR between January 2019 and April 2023.
InterventionsProspective collection of variables and follow-up for up to 180 days.
Main variables of interestTo assess outcomes, survival with good neurological outcome defined as a Cerebral Performance Categories scale 1–2 at 180 days was used. Secondary variables were collected including demographics and comorbidities, cardiac arrest and cannulation characteristics, ROSC, ECMO-related complications, survival to ECMO decannulation, survival at Intensive Care Unit (ICU) discharge, survival at 180 days, neurological outcome, cause of death and eligibility for organ donation.
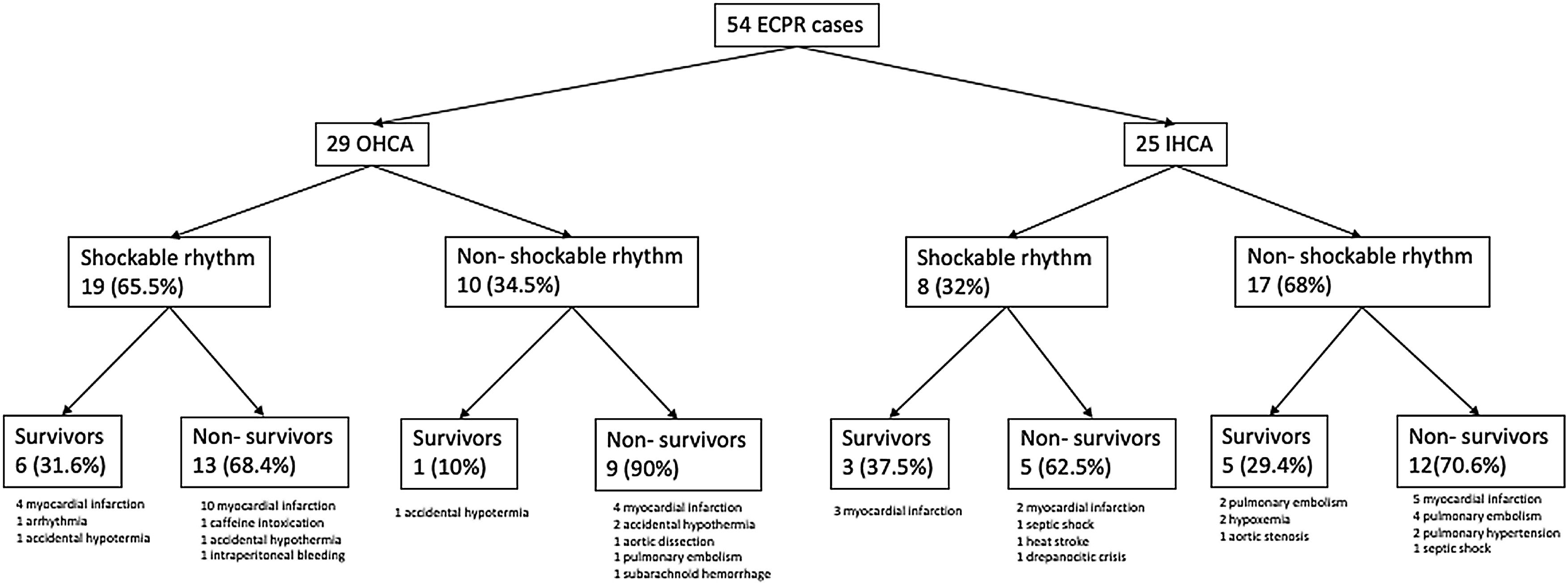
ResultsFifty-four patients received ECPR, 29 for OHCA and 25 for IHCA. Initial shockable rhythm was identified in 27 (50%) patients. The most common cause for cardiac arrest was acute coronary syndrome [29 (53.7%)] followed by pulmonary embolism [7 (13%)] and accidental hypothermia [5 (9.3%)]. Sixteen (29.6%) patients were alive at 180 days, 15 with good neurological outcome. Ten deceased patients (30.3%) became organ donors after neuroprognostication.
ConclusionsThe implementation of a multidisciplinary ECPR program in an experienced Extracorporeal Membrane Oxygenation center in Spain is feasible and can lead to good survival outcomes and valid organ donors.
Analizar si la implementación de un programa multidisciplinario de reanimación cardiopulmonar extracorpórea (ECPR) en un hospital terciario en España es factible y puede conseguir buenos resultados de supervivencia, similares a las experiencias publicadas internacionalmente.
DiseñoEstudio de cohortes observacional retrospectivo.
ÁmbitoHospital universitario de referencia terciaria en España.
PacientesTodos los pacientes adultos que recibieron ECPR entre enero de 2019 y abril de 2023.
IntervencionesRecogida de variables prospectiva y seguimiento hasta 180 días.
Variables de interés principalesPara evaluar los resultados, se utilizó la supervivencia con buen resultado neurológico definida como un valor de 1–2 a los 180 días en la escala Cerebral Performance Categories. Se recogieron variables secundarias incluyendo las características de la parada cardíaca, la canulación, complicaciones, resultados, causa de muerte y donación de órganos.
ResultadosCincuenta y cuatro pacientes recibieron ECPR, 29 por parada cardíaca extrahospitalaria y 25 por intrahospitalaria. Se identificó un ritmo inicial desfibrilable en 27 (50%) pacientes. La causa más frecuente de parada cardíaca fue el síndrome coronario agudo [29 (53.7%)] seguido de la embolia pulmonar [7 (13%)] y la hipotermia accidental [5 (9.3%)]. Dieciséis (29.6%) pacientes estaban vivos a los 180 días, 15 con buen resultado neurológico. Diez pacientes de los fallecidos (30.3%) fueron donantes de órganos.
ConclusionesLa implementación de un programa ECPR multidisciplinario en un centro de referencia de ECMO en España es factible y puede conducir a buenos resultados de supervivencia y donantes de órganos válidos.
Cardiac arrest, defined as the sudden cessation of cardiac activity, is the third leading cause of death in Europe,1 where the incidence of out-of-hospital cardiac arrest (OHCA) ranges between 67–170 cases per 100,000 inhabitants.2 Reported survival rates at hospital discharge are poor, ranging between 0%–18%1,2; in Spain they are around 13%.3 The incidence of in-hospital cardiac arrest (IHCA) varies between 1.5–2.8 per 1000 hospital admissions and outcomes are also unfavorable, with a reported survival to hospital discharge between 15%–35% despite the easier access to advanced cardiopulmonary resuscitation (CPR).2,4
The probability of achieving the return of spontaneous circulation (ROSC) is directly related to the duration of CPR and falls to near zero if the duration of conventional CPR is longer than 40 min.5,6 This phenomenon is attributable both to the deteriorating metabolic state of the patient and the impossibility of treating the precipitating cause under ongoing CPR.7
Current guidelines recommend the use of venoarterial extracorporeal membrane oxygenation (V-A ECMO) in cardiac arrest (ECPR) in selected refractory cases.8 However, the scientific evidence is unclear. Three landmark randomized clinical trials (RCT) investigated efficacy and safety of ECPR in OHCA showing different results. However, after a first single center randomized clinical trial that was stopped due to significant evidence of benefit in the ECPR treatment branch,9 a second one failed to show any difference in survival with good neurological outcome.10 A third, pragmatic, multicenter clinical trial did not show evidence of benefit for the ECPR approach.11 One of the main conclusions derived from the analysis of these studies is the significant impact of organizational aspects on the outcomes of ECPR programs and the need for strict monitoring, especially in the first phases of development.
In Spain, no well-designed regionally organized ECPR programs are in place, and no large series have been reported to date.12,13 The ability of our healthcare system to replicate the favorable outcomes achieved in some international studies is unknown, as well as the optimal way to organize teams for this purpose. The objective of this study was to determine whether the implementation of an ECPR program in a high-volume ECMO center is feasible and can yield 180-day survival outcomes comparable to international experiences.
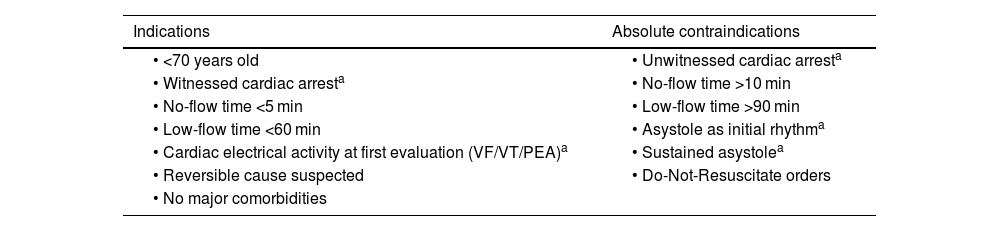
Patients and methodsStudy designRetrospective observational study of prospectively collected data from all consecutive patients between 18 and 75 years old who received ECPR for both OHCA and IHCA between January 2019 and April 2023 in a tertiary referral university hospital in Spain. The criteria for ECPR are detailed in Table 1. ECPR was defined as the application of V-A ECMO in patients in cardiac arrest where conventional CPR measures are unsuccessful in achieving a sustained ROSC, according to the Extracorporeal Life Support Organization (ELSO) definition.14 The follow-up ended at 180 days after cardiac arrest.
Extracorporeal cardiopulmonary resuscitation indications and contraindications.
| Indications | Absolute contraindications |
|---|---|
| • <70 years old | • Unwitnessed cardiac arresta |
| • Witnessed cardiac arresta | • No-flow time >10 min |
| • No-flow time <5 min | • Low-flow time >90 min |
| • Low-flow time <60 min | • Asystole as initial rhythma |
| • Cardiac electrical activity at first evaluation (VF/VT/PEA)a | • Sustained asystolea |
| • Reversible cause suspected | • Do-Not-Resuscitate orders |
| • No major comorbidities |
VF: ventricular fibrillation; VT: ventricular tachycardia; PEA: pulseless electrical activity.
The primary objective of our study was to evaluate whether the implementation of an ECPR program in an experienced ECMO center in Spain can yield results comparable to published experiences, for which survival with good neurological outcome at 180 days was analysed and compared side-by-side with the published literature. Good neurological outcome was defined as a 1–2 score on the Cerebral Performance Categories (CPC) scale.15 A CPC 1 score indicates full or near-full recovery of brain function, allowing for a normal life with minimal disability, while a CPC 2 score signifies moderate disability, enabling independent living and work with some limitations. As secondary objectives, we investigate the incidence of in-hospital complications and potential for organ donation of patients who did not survive due to neurological damage.
Clinical variables were prospectively collected, including demographics and comorbidities, cardiac arrest and cannulation characteristics, ROSC, ECMO-related complications, survival to ECMO decannulation, survival at Intensive Care Unit (ICU) discharge, survival at 180 days, neurological outcome, cause of death and eligibility for organ donation. Definitions of variables can be seen in Supplementary material.
This study has been approved by the Ethics Committee for Drug Research and Research Projects Commission of the Vall d’Hebron University Hospital with code ECPRVH and number of registry PR(AG)466/2023 and was done in accordance with internationally accepted recommendations for clinical investigation (Declaration of Helsinki of the World Medical Association). Due to the retrospective observational nature of the study and the characteristics of the patients, an exemption from informed consent was obtained.
SettingOur center serves as a referral center for cardiac arrest, ECMO and accidental hypothermia, providing round-the-clock full resources for ECMO support, cardiac surgery, cardiac catheterization, interventional vascular radiology, and other advanced interventions. Cardiac arrest patients are admitted to the polyvalent ICU within the Department of Intensive Care Medicine or to the Acute Cardiovascular Care Unit ascribed to the Cardiology Department, depending on the etiology of the arrest, and are managed by a multidisciplinary team.
Our ECMO program provides V-V and V-A ECMO support with a case volume of more than 100 cases/year, with a fully trained multidisciplinary ECMO team and ELSO-based management. The program started to provide ECPR in selected patients with cardiac arrest in 2017.
ECPR programBefore 2019 sporadic cases with very specific clinical context were considered for ECPR. During the years 2018 and 2019, a specific hospital protocol was developed and agreed upon by all participants (Intensive Care Medicine, Cardiology, Cardiac Surgery, Emergency Medicine, and Transplant Coordination), which outlined the indications, contraindications, complete procedure, team organization, and management of the patient before, during, and after ECMO cannulation. All these aspects were structured in the form of standardized operating procedures. A role chart was created, specifying 10 minimum positions required to perform the procedure (Supplementary material). Modifications were made to the conventional advanced cardiopulmonary resuscitation algorithm for refractory cases, and pauses for rhythm checks, defibrillations and adrenaline administration were forfeited to minimize interruptions in high quality chest compressions.
After protocol implementation, training sessions were conducted, and a training plan based on in-situ clinical simulation was initiated. A complete cannulation team, comprising an intensivist with cannulation competency and two ECMO specialists (ICU nurses with competency in ECMO initiation and management) was available on-site 24/7. A pre-primed circuit and the cannulation equipment were organized to be portable and readily available when a patient meeting ECPR criteria was identified.
Cannulation was primary performed by intensivists using ultrasound-guided percutaneous technique. Ultrasound guidance for the placement of the guidewires was performed using transthoracic echocardiography from the subcostal view, except for patients located in the catheterization laboratory (CCL), where the procedure was supported with fluoroscopy guidance by interventional cardiologists. Surgical backup for cannulation was provided by cardiac surgery. Patients were cannulated in situ at the location of arrest for IHCA cases and in the Emergency Department or the CCL for OHCA cases depending on availability. The preferred cannulation approach was right femoro-femoral, utilizing a 23–25 Fr, 55 cm drainage cannula and a 15−17 F, 15 cm return cannula (HLS, Getinge AB, Sweden). A 6–8 Fr distal reperfusion catheter was inserted later. ECMO support was initiated using CardioHelp and 7.0 circuit (Getinge AB, Sweden) or Novalung with XLung circuit (Fresenius Medical Care, Germany) depending on availability. All patients received mechanical chest compressions using LUCAS® (Stryker Corporation, Michigan, USA). Once ECMO was initiated and a stable blood flow of >2.5 L/min was achieved, chest compressions were stopped. The initial gas flow was set at 1 L/min with 50% oxygen concentration. Coronary angiography was performed based on etiological suspicion, and a whole-body CT scan was requested for all patients per protocol. The need for left ventricular unloading was individualized on a case-by-case basis. In cases where primary angioplasty was performed, the need for unloading was decided after evaluating an echocardiogram after revascularization. The intraaortic balloon pump was prioritized as unloading device, reserving Impella-CP® (Abiomed, US) for patients with very poor ventricular function, absence of aortic valve opening, and clinical parameters with a high possibility of good neurological outcome. Post-resuscitation care included targeted temperature management at 33 or 35 °C (clinical decision based on the patient’s condition) and multimodal assessment of neurological prognosis.
Statistical analysisAn initial descriptive analysis was performed. Variables were described using mean and standard deviation (SD), median and interquartile range (IQR) (distance between the 25th and 75th percentiles) or frequency and percentage. Survivors and non-survivors at three months were compared in a univariate analysis using Chi2 test or Fisher’s exact test for categorical variables. The distribution of continuous variables was assessed using the Saphiro–Wilk test, and Kruskal–Wallis H test, Mann Whitney U test or Student t test were used for univariate comparisons as appropriate. Statistical significance was considered when p < 0.05. Analyses were performed using Stata (version 17.0BE, StataCorp, College Station, Texas, USA).
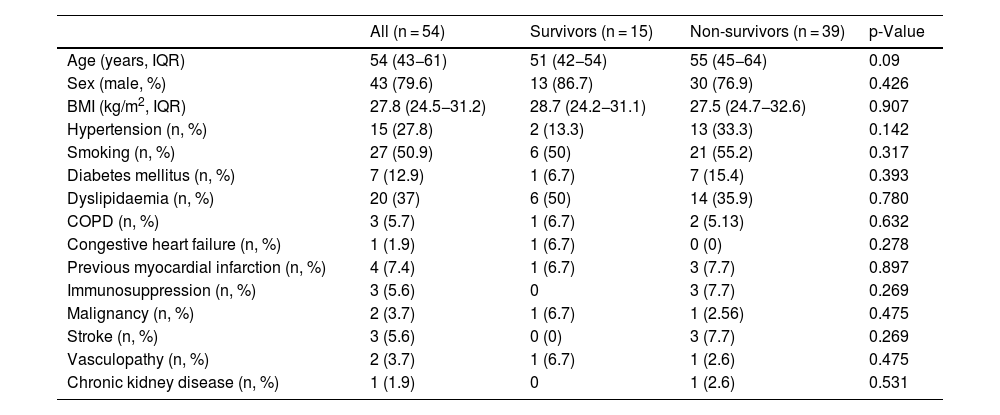
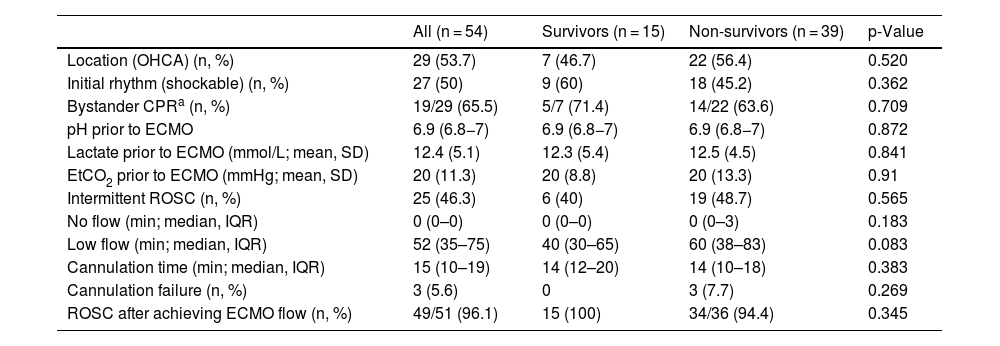
ResultsBaseline, cardiac arrest and cannulation characteristicsDuring the study period, 54 patients received ECPR. Twenty-nine suffered OHCA and 25 IHCA. The baseline characteristics for survivors and non survivors are detailed in Table 2. The cardiac arrest characteristics are described in Table 3. The most common cause for cardiac arrest was acute coronary syndrome [29, 53.7%] followed by pulmonary embolism [7 (13%)] and accidental hypothermia [5 (9.3%)].
Baseline characteristics for survivors and non-survivors (deceased and CPC >2 combined).
| All (n = 54) | Survivors (n = 15) | Non-survivors (n = 39) | p-Value | |
|---|---|---|---|---|
| Age (years, IQR) | 54 (43−61) | 51 (42−54) | 55 (45−64) | 0.09 |
| Sex (male, %) | 43 (79.6) | 13 (86.7) | 30 (76.9) | 0.426 |
| BMI (kg/m2, IQR) | 27.8 (24.5−31.2) | 28.7 (24.2−31.1) | 27.5 (24.7−32.6) | 0.907 |
| Hypertension (n, %) | 15 (27.8) | 2 (13.3) | 13 (33.3) | 0.142 |
| Smoking (n, %) | 27 (50.9) | 6 (50) | 21 (55.2) | 0.317 |
| Diabetes mellitus (n, %) | 7 (12.9) | 1 (6.7) | 7 (15.4) | 0.393 |
| Dyslipidaemia (n, %) | 20 (37) | 6 (50) | 14 (35.9) | 0.780 |
| COPD (n, %) | 3 (5.7) | 1 (6.7) | 2 (5.13) | 0.632 |
| Congestive heart failure (n, %) | 1 (1.9) | 1 (6.7) | 0 (0) | 0.278 |
| Previous myocardial infarction (n, %) | 4 (7.4) | 1 (6.7) | 3 (7.7) | 0.897 |
| Immunosuppression (n, %) | 3 (5.6) | 0 | 3 (7.7) | 0.269 |
| Malignancy (n, %) | 2 (3.7) | 1 (6.7) | 1 (2.56) | 0.475 |
| Stroke (n, %) | 3 (5.6) | 0 (0) | 3 (7.7) | 0.269 |
| Vasculopathy (n, %) | 2 (3.7) | 1 (6.7) | 1 (2.6) | 0.475 |
| Chronic kidney disease (n, %) | 1 (1.9) | 0 | 1 (2.6) | 0.531 |
BMI: body mass index; COPD: chronic obstructive pulmonary disease; IQR: interquartile range.
Cardiac arrest characteristics for survivors and non survivors (deceased and CPC >2 combined at 180 days).
| All (n = 54) | Survivors (n = 15) | Non-survivors (n = 39) | p-Value | |
|---|---|---|---|---|
| Location (OHCA) (n, %) | 29 (53.7) | 7 (46.7) | 22 (56.4) | 0.520 |
| Initial rhythm (shockable) (n, %) | 27 (50) | 9 (60) | 18 (45.2) | 0.362 |
| Bystander CPRa (n, %) | 19/29 (65.5) | 5/7 (71.4) | 14/22 (63.6) | 0.709 |
| pH prior to ECMO | 6.9 (6.8−7) | 6.9 (6.8−7) | 6.9 (6.8−7) | 0.872 |
| Lactate prior to ECMO (mmol/L; mean, SD) | 12.4 (5.1) | 12.3 (5.4) | 12.5 (4.5) | 0.841 |
| EtCO2 prior to ECMO (mmHg; mean, SD) | 20 (11.3) | 20 (8.8) | 20 (13.3) | 0.91 |
| Intermittent ROSC (n, %) | 25 (46.3) | 6 (40) | 19 (48.7) | 0.565 |
| No flow (min; median, IQR) | 0 (0–0) | 0 (0–0) | 0 (0–3) | 0.183 |
| Low flow (min; median, IQR) | 52 (35–75) | 40 (30–65) | 60 (38–83) | 0.083 |
| Cannulation time (min; median, IQR) | 15 (10–19) | 14 (12–20) | 14 (10–18) | 0.383 |
| Cannulation failure (n, %) | 3 (5.6) | 0 | 3 (7.7) | 0.269 |
| ROSC after achieving ECMO flow (n, %) | 49/51 (96.1) | 15 (100) | 34/36 (94.4) | 0.345 |
OHCA: out of hospital cardiac arrest; CPR: cardiopulmonary resuscitation; EtCO2: end-tidal CO2; ROSC: return of spontaneous circulation; No flow: time from cardiac arrest to cardiopulmonary resuscitation; Low flow: time from cardiopulmonary resuscitation to ECMO initiation; SD: standard deviation; IQR: interquartile range.
Most patients [34 (63%)] were cannulated outside working hours (8 am–5 pm Monday to Friday). This was equally common in OHCA as in IHCA (68% vs 56%, p-value 0.325). Most common cannulation technique was percutaneous (50 cannulations, 92.6%). Thirty patients (55.6%) were cannulated “in situ” or in the ED; twenty (37%) were cannulated in the CCL and four patients (7.4%) required surgical cannulation. Cannulation was successful in 51 patients (94.4%). Thirteen patients (24.1%) suffered vascular complications derived from the cannulation. The most common complication was cannulation site bleeding [8, (14.8%)], followed by accidental veno-venous cannulation [2, (3.7%)]. Severe complications occurred in 5.5% of cases (1 accidental decannulation and 2 arterial dissections).
For IHCA cases, the most common initial rhythm was pulseless electrical activity (PEA) [16 (64%)]. The median low flow time was 35 min (IQR 27.5–47.5). All patients were cannulated in the arrest location, 10 (40%) in the ICU, 7 (28%) in the CCL, four (16%) in the emergency department (ED), three (12%) in conventional wards and one (4%) in the operation room (OR).
For OHCA cases, the most common initial rhythm was ventricular fibrillation (VF) [19 (65.5%)]. The median low flow time was 68 min (IQR 52−86). Fifteen patients (51.7%) were cannulated in the ED, nine (31%) in the CCL, four (13.8%) in the ICU and one (3.5%) in the OR.
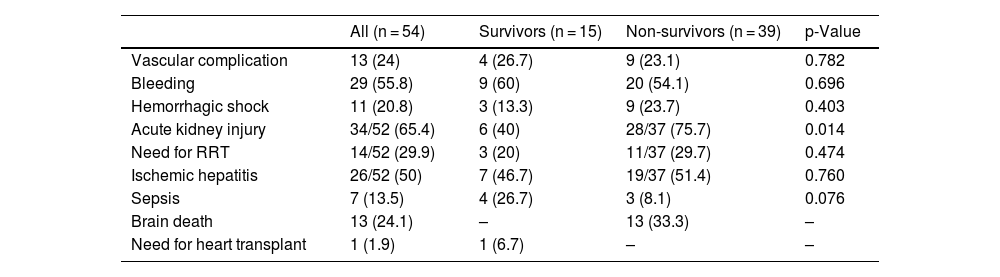
Post-arrest management and complicationsEmergent coronary angiography was indicated in 34 patients (63%), a culprit lesion was found in 28 (51,85%) patients and percutaneous coronary intervention was performed in 26 cases (48.1%). Left ventricle unloading was indicated in 15 patients (27.8%) (13 with intra-aortic balloon pump and 2 with microaxial blood pump) based on clinical decision. During their ICU stay, 34 (65.4%) patients developed acute kidney injury and 26 (50%) presented ischemic hepatitis. Hemorrhagic complications that required intervention such as blood product transfusion were evidenced in 29 (55.8%) patients and 11 (20.8%) developed hemorrhagic shock. Seven (13.5%) patients developed a septic complication. A more detailed summary of complications can be found in Table 4.
Complications for survivors and non survivors (deceased and CPC >2 combined at 180 days).
| All (n = 54) | Survivors (n = 15) | Non-survivors (n = 39) | p-Value | |
|---|---|---|---|---|
| Vascular complication | 13 (24) | 4 (26.7) | 9 (23.1) | 0.782 |
| Bleeding | 29 (55.8) | 9 (60) | 20 (54.1) | 0.696 |
| Hemorrhagic shock | 11 (20.8) | 3 (13.3) | 9 (23.7) | 0.403 |
| Acute kidney injury | 34/52 (65.4) | 6 (40) | 28/37 (75.7) | 0.014 |
| Need for RRT | 14/52 (29.9) | 3 (20) | 11/37 (29.7) | 0.474 |
| Ischemic hepatitis | 26/52 (50) | 7 (46.7) | 19/37 (51.4) | 0.760 |
| Sepsis | 7 (13.5) | 4 (26.7) | 3 (8.1) | 0.076 |
| Brain death | 13 (24.1) | – | 13 (33.3) | – |
| Need for heart transplant | 1 (1.9) | 1 (6.7) | – | – |
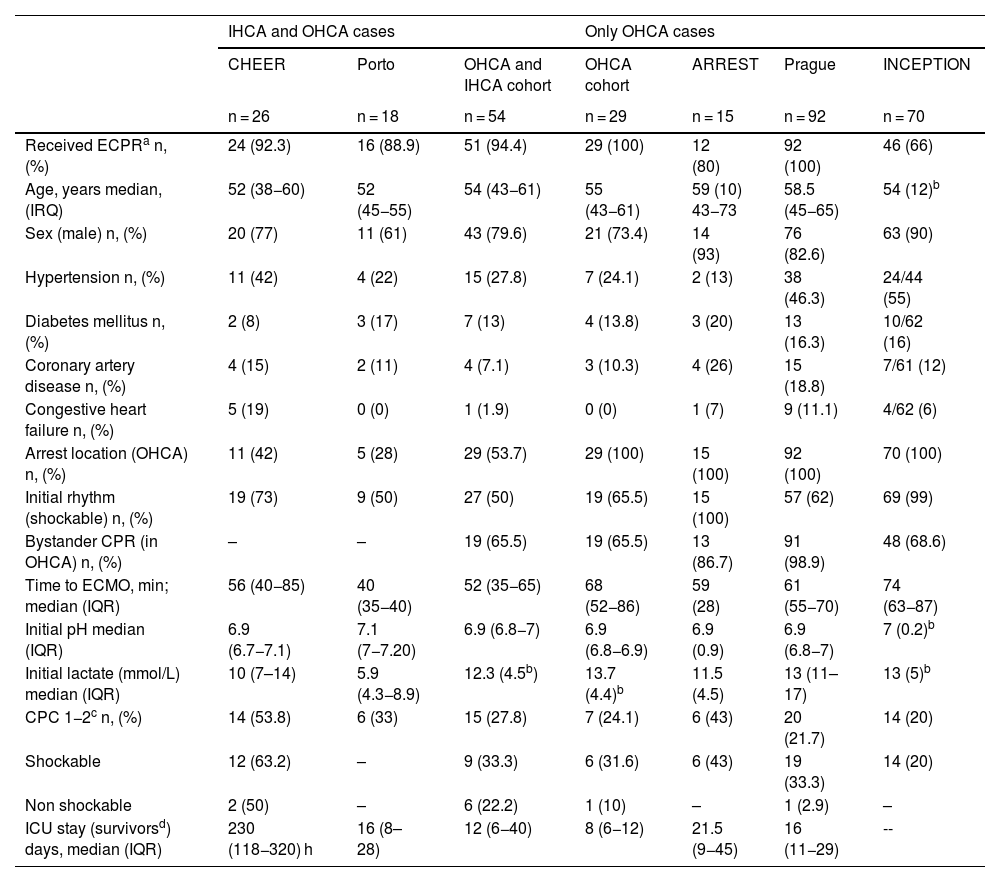
A summary of the outcomes is detailed in Fig. 1. Side-by-side comparison with international experiences are shown in Table 5.
| IHCA and OHCA cases | Only OHCA cases | ||||||
|---|---|---|---|---|---|---|---|
| CHEER | Porto | OHCA and IHCA cohort | OHCA cohort | ARREST | Prague | INCEPTION | |
| n = 26 | n = 18 | n = 54 | n = 29 | n = 15 | n = 92 | n = 70 | |
| Received ECPRa n, (%) | 24 (92.3) | 16 (88.9) | 51 (94.4) | 29 (100) | 12 (80) | 92 (100) | 46 (66) |
| Age, years median, (IRQ) | 52 (38−60) | 52 (45−55) | 54 (43−61) | 55 (43−61) | 59 (10) 43−73 | 58.5 (45−65) | 54 (12)b |
| Sex (male) n, (%) | 20 (77) | 11 (61) | 43 (79.6) | 21 (73.4) | 14 (93) | 76 (82.6) | 63 (90) |
| Hypertension n, (%) | 11 (42) | 4 (22) | 15 (27.8) | 7 (24.1) | 2 (13) | 38 (46.3) | 24/44 (55) |
| Diabetes mellitus n, (%) | 2 (8) | 3 (17) | 7 (13) | 4 (13.8) | 3 (20) | 13 (16.3) | 10/62 (16) |
| Coronary artery disease n, (%) | 4 (15) | 2 (11) | 4 (7.1) | 3 (10.3) | 4 (26) | 15 (18.8) | 7/61 (12) |
| Congestive heart failure n, (%) | 5 (19) | 0 (0) | 1 (1.9) | 0 (0) | 1 (7) | 9 (11.1) | 4/62 (6) |
| Arrest location (OHCA) n, (%) | 11 (42) | 5 (28) | 29 (53.7) | 29 (100) | 15 (100) | 92 (100) | 70 (100) |
| Initial rhythm (shockable) n, (%) | 19 (73) | 9 (50) | 27 (50) | 19 (65.5) | 15 (100) | 57 (62) | 69 (99) |
| Bystander CPR (in OHCA) n, (%) | – | – | 19 (65.5) | 19 (65.5) | 13 (86.7) | 91 (98.9) | 48 (68.6) |
| Time to ECMO, min; median (IQR) | 56 (40−85) | 40 (35−40) | 52 (35−65) | 68 (52−86) | 59 (28) | 61 (55−70) | 74 (63−87) |
| Initial pH median (IQR) | 6.9 (6.7−7.1) | 7.1 (7−7.20) | 6.9 (6.8−7) | 6.9 (6.8−6.9) | 6.9 (0.9) | 6.9 (6.8−7) | 7 (0.2)b |
| Initial lactate (mmol/L) median (IQR) | 10 (7–14) | 5.9 (4.3−8.9) | 12.3 (4.5b) | 13.7 (4.4)b | 11.5 (4.5) | 13 (11–17) | 13 (5)b |
| CPC 1−2c n, (%) | 14 (53.8) | 6 (33) | 15 (27.8) | 7 (24.1) | 6 (43) | 20 (21.7) | 14 (20) |
| Shockable | 12 (63.2) | – | 9 (33.3) | 6 (31.6) | 6 (43) | 19 (33.3) | 14 (20) |
| Non shockable | 2 (50) | – | 6 (22.2) | 1 (10) | – | 1 (2.9) | – |
| ICU stay (survivorsd) days, median (IQR) | 230 (118−320) h | 16 (8–28) | 12 (6−40) | 8 (6−12) | 21.5 (9−45) | 16 (11−29) | -- |
Notes: for the Porto study, only the ECPR cohort was considered.
Only the ECPR cohort from all studies has been considered.
***Hours.
Sixteen (29.6%) patients were alive at 180 days, 15 with a CPC 1–2 (93,7%). Survival with good neurological outcome in IHCA was 32% (8 out of 25), whereas in OHCA it was 24.1% (7 out of 29). In the case of initial shockable rhythms, survival was 33.3% (9 patients) and in non-shockable rhythms 21.2% (7 patients). One (6.7%) survivor required heart transplant due to refractory heart failure. Median ICU stay of survivors was 12 (IQR 6–36) days, with a hospital length of stay of 23 (IQR 12–62) days.
After successful cannulation ROSC was not obtained in two (3.9%) patients and were declared dead. For the rest of the patients who died, the most common cause of death was anoxic encephalopathy (17 patients, 51.5%): ten (30.3%) suffered brain death and in seven (21.2%) patients support was withdrawn after neuroprognostication. Multiorgan dysfunction was the second most common cause of death [12 patients (36.4%)]. Five (15.2%) patients died of complications occurring during their ICU stay. Ten (30.3%) patients became organ donors [4 (40% after brain death and 6 (60%) through donation after cardiac death) and a total of 16 kidneys, seven livers and four lungs were explanted.
DiscussionThis study presents the first published experience in Spain in the use of ECPR for OHCA and IHCA. We describe a comprehensive model of care for refractory cardiac arrest provided by a multidisciplinary ECMO team, with round the clock coverage and associated to an organ donation program, with good survival with adequate neurological outcome, comparable to published data from experienced centers.
The optimal approach to respond to refractory cardiac arrest through an ECPR program is not yet established and needs to be individualized depending on the characteristics of every region. In Spain, consensus documents have been developed in recent years regarding the organization of ECMO programs, but none specifically reference ECPR.16–18 Our study presents a functional ECPR model that allows to respond to any cardiac arrest, regardless of its etiology, 24 h, 7 days, 365 days a year.
Few studies focusing on ECPR and detailing the program organization have been published. Stub et al. shared the results of the CHEER trial, conducted in Melbourne, Australia, in 2015.19 Eligible patients were cannulated in situ or in the ED by intensivists and subjected to a bundle of therapeutic hypothermia and early invasive coronary assessment. In this trial, 26 patients (15 IHCA and 11 OHCA) were supported with ECPR, with the majority (73%) presenting initial shockable rhythms. The study showed a 54% survival with CPC 1–2, with an average low-flow time of 56 (40 85) min, which was significantly shorter in the survivor group (40 min [IQR 27–57]). Roncon-Albuquerque Jr et al. published another observational study in 2018, detailing the results of a comprehensive ECPR program linked with an uncontrolled donation after circulatory death (uDCD) program.20 Eighteen patients met ECPR criteria (72% IHCA) including patients with shockable and non-shockable rhythms (50% VF). Survival to hospital discharge with good neurological outcome was 33% after an average low-flow time of 40 (35–50) min. Although our study shares similarities with both studies (single-center study including IHCA and OHCA cases), both report higher prevalence of shockable rhythms and lower low flow times.
Three clinical trials based on different ECPR models have recently been published with disparate results.9–11 The ARREST trial published in 2020 and conducted at a single center in Minnesota, randomized patients with OHCA and initial shockable rhythms to receive either ECPR or conventional CPR at hospital arrival. This study was prematurely terminated after 30 randomized patients due to a significant difference in survival favorable to the ECPR group (43% vs 7% at hospital discharge).9 The differences in survival compared with our study can be explained by the strict selection of only shockable rhythms and a shorter low-flow time. Comparatively, in our study only 27 (45%) of patients presented an initial shockable rhythm, which was more frequent in the cohort of patients suffering OHCA, and low flow times were longer, especially in the OHCA cohort.
Two years later, Belohlavek et al. published a second randomized study on OHCA in Prague, including shockable and non-shockable rhythms. Patients were randomized to intra-arrest transport for a bundle of treatment that included ECPR and early invasive assessment and treatment versus continuation of conventional CPR on-site. No differences were found in the intention-to-treat analysis, but crossovers were allowed from the control group to the invasive arm.10 In a secondary analysis the overall survival with favorable neurological outcome was 21.7% for those who received ECPR, with a significant difference in survival between patients with an initial shockable rhythm (33.3%) and those with a non-shockable rhythm (2.9%).21 Interestingly, our study yielded similar results in the OHCA cohort (survival was 31.6% for shockable rhythms and 10% in non-shockable rhythms) but when including IHCA cases survival increased to 22.2% for non-shockable rhythms.
The causes of IHCA comprise a higher prevalence of pathologies leading to non-shockable rhythms in the very initial assessment. Oppositely, non-shockable rhythms in OHCA might be identified in later phases of a cardiac arrest with an initial shockable rhythm, suggesting low quality CPR or excessively prolonged low flow times, which may lead to lower survival rates. Notably, these differences suggest that the role of the initial rhythm in IHCA may not be as relevant as in OHCA and may have to be excluded in the decision algorithm in this setting.
The latest clinical trial to date was the multicenter INCEPTION trial, published in 2023. It included ECPR cases performed in 10 hospitals in The Netherlands and compared transportation for in hospital ECPR versus continuation of conventional CPR on scenes. In this study, survival was low in both groups (20% with CPC 1–2 in the intervention group and 16% in the control group), with only 61.4% of patients receiving ECPR in the intervention group and remarkably longer low-flow and cannulation times compared with the previous clinical trials. Interestingly, most centers received a low volume of cases and most of the centers reported no previous ECPR experience.11 This may explain the higher survival rate in our study, as it portrays the results of a comprehensive ECPR program implemented at a high-volume ECMO center, with significant prior experience and specific ECMO team training.
To reach this point, it has been essential to have a large and highly experienced human team, specifically trained in ECMO and ECPR. This has enabled us to provide excellent coverage for IHCA, but OHCA remains a significant challenge. Firstly, for a patient to be eligible for ECPR, no flow time should be lower than five minutes, and in Spain bystander CPR is less common than in other European countries.22 Improving early access to CPR will have a global impact in survival with good neurological outcome in all cardiac arrest cases,23 not only in those requiring ECPR. Secondly, during the study period no specific transport and coordination operating procedure was in place in the prehospital setting and we believe that outcomes can be improved with better coordination between hospitals and emergency systems. Our emergency medical system is physician-led, and traditionally OHCA cases are not transported to the hospital unless ROSC is achieved, which may have led to longer low flow times and potentially worse neurological results. Implementing an ECPR program requires a change in the model and approach to these patients, as early transportation to receiving centers is essential. This may raise concerns, as on-site care for OHCA appears to have better survival outcomes than transport,24 making it crucial to determine the optimal timing and approach for transportation, as well as ensuring excellent coordination between hospitals and emergency medical services.
Other ECPR models for OHCA exist worldwide,25 including transporting hospital-based teams to cannulate in the prehospital setting.26 This adds significant logistical complexity and a human resource challenge, which our healthcare system will need to assess for feasibility and viability to extend ECPR to patients who cannot be transported within a sensible amount of time to a hospital with ECPR capabilities.
Unfortunately, between 50%–80% of patients who receive ECPR die despite all the efforts. However, most of the patients who died of neurological causes in our study became multiorgan donors showing how an ECPR program can produce a secondary good outcome by increasing organ donation.27 Additionally, patients with refractory cardiac arrest who do not meet ECPR criteria can potentially become donors through uncontrolled donation after cardiac death (uDCD) programs, in which Spain is an international pioneer.28 These programs require similar logistics and techniques, thus the synergies between ECPR and uDCD can offer significant benefits for patients and society.20
Designing, organizing, and implementing an ECPR program is highly complex. ECPR has emerged as a therapeutic option for refractory cardiac arrest, so we must strive to make its implementation a reality.
The main limitation of our study is its observational, retrospective, and single-center nature without control group. This program has been implemented in a high volume ECMO center in which cannulation and ECMO initiation is mostly performed by intensivists and ICU nurses, with surgical support in case of complications. This model facilitates rapid response as all required personnel for ECPR are already on site; this structure, however, is not common in our country, which may limit the generalizability of our results to other settings.
ConclusionsThe implementation of a multidisciplinary ECPR program in a single tertiary hospital with extensive ECMO experience is feasible and can lead to survival with good neurological outcomes comparable to those reported in international literature. In addition to the primary goal of achieving survival with good neurological outcomes, ECPR programs can also secondarily facilitate the emergence of organ donors.
Author’s contributionsMaría Martínez-Martínez gathered data, participated in the conceptualization and design of the study, writing and edition of the manuscript and performed the statistical analysis.
Maria Vidal gathered data, participated in the conceptualization and design of the study, and writing and edition of the manuscript.
Jordi Riera participated in the conceptualization and design of the study and writing and edition of the manuscript.
Aitor Uribarri participated in the conceptualization and design of the study and writing and edition of the manuscript.
Elisabet Gallart participated in the revision and edition of the manuscript.
Laia Milà participated in the revision and edition of the manuscript.
Pau Torrella gathered data and participated in the edition of the manuscript.
Irene Buera participated in the revision and edition of the manuscript.
Luis Chiscano-Camon participated in the revision and edition of the manuscript.
Bruno García del Blanco participated in the revision and edition of the manuscript.
Carlota Vigil-Escalera participated in the revision and edition of the manuscript.
José A. Barrabés participated in the revision and edition of the manuscript.
Jordi Llaneras participated in the revision and edition of the manuscript.
Juan Carlos Ruiz-Rodríguez participated in the revision and edition of the manuscript.
Cristopher Mazo participated in the revision and edition of the manuscript.
Jorge Morales participated in the revision and edition of the manuscript.
Ricard Ferrer participated in the revision and edition of the manuscript.
Ignacio Ferreira-Gonzalez participated in the revision and edition of the manuscript.
Eduard Argudo gathered data, coordinates the conceptualization and design of the study, and the writing and edition of the manuscript.
All the authors approved the final version.
Conflicts of interestAuthors declare no conflicts of interest.
FundingThis research has not received funding.
To all the medical, nursing, auxiliary, and porter staff from all departments of Vall d’Hebron Hospital who play a crucial role in making this program a reality.
To all the personnel of the Sistema d’Emergencies Mèdiques (SEM) who have made tremendous efforts to seek therapeutic options for their patients in refractory cardiac arrest.