Edited by: Rosario Amaya Villar - Unidad de Cuidados Intensivos, Hospital Universitario Virgen del Rocio, Sevilla, España
Last update: December 2023
More infoObstructive pulmonary diseases often require invasive mechanical ventilation.1,2 Flow limitation is a dynamic condition where expiratory flow reaches its maximum value despite the increase of the different pressure between alveoli and airway. The exact mechanisms and anatomical location of the limitation are still unclear, which is why, in most cases, small collapsible airways are responsible for this.3 During the mechanics of ventilation there is a higher peak pressure, resistance pressure, and plateau pressure (Pplat) with lower compliance and hyperinflation with generation of intrinsic PEEP (iPEEP) that is suggested when the expiratory flow-volume curve does not reach zero. This expiratory flow-volume curve can show sudden changes of the gradient due to dynamic collapse and reduction of flow to the point of reaching a “square-root” morphology.
Hyperinflation and iPEEP are associated with certain adverse events. There is a reduced left ventricular end-diastolic volume and arterial hypotension at hemodynamic level. There is hypoventilation at pulmonary level despite the increased minute volume due to local overdistension of areas that do not empty during expiration and compress adjacent structures, and barotrauma.4 We can draw a line between hypotension due to hyperinflation or barotrauma. If the patient is disconnected for 15 s and arterial blood pressure increases, the cause is pulmonary hyperinflation. If not, we should think of the possibility of pneumothorax. Another side effect here is the increased work of breathing for the patient with the appearance of asynchronies. This is so because to activate the ventilator the patient first needs to overcome the pressure generated by iPEEP, and then activate the ventilator trigger. If he cannot comply, ineffective effort asynchronies appear.3–5
Entrapment can occur due to inadequate programming of the ventilation as it is the case with elevated respiratory rates that just do not allow total lung emptying. The effects that ventilator adjustments have on pulmonary hyperinflation in patients with respiratory distress syndrome have been assessed recently. It was concluded that in sedated patients on neuromuscular blocking agents, and without a known obstructive pulmonary disease, iPEEP is insignificant and does not affect the mechanical properties of ventilation.6 Nonetheless, each case should be handled individually to assess the effect aerial entrapment has on the mechanics of ventilation and hemodynamics, especially if the patient has not been deeply sedated or for the lack of neuromuscular blocking agents.
The most widely used way to measure iPEEP is through the expiratory hold maneuver provided that the patient does not make any respiratory efforts. Therefore, it is important to see the expiratory hold curve and make sure that the measurement is correct. However, this maneuver is not associated with the appearance of complications but it is indeed associated with end-inspiratory lung volume (EILV) (tidal volume plus trapped volume). Therefore, the total volume of gas exhaled after 60 s of apnea is estimated in such a way that EILV > 20 mL/kg will be predictive of complications. Roesthuis et al. assessed easier-to-use methods at the patient’s bedside that can show EILV more accurately.7
Whenever the expiratory hold maneuver is used what we’re doing is measuring the air that is in contact with the upper airway. However, when at the end of expiration, the airway is closed, the air trapped from behind is not in contact with the primary airway, and the ventilator cannot measure the pressure it produces. This unmeasured pressured is called hidden PEEP (hPEEP). It can be suspected when despite managing to reduce iPEEP after different maneuvers, the Pplat does not go down. A maneuver capable of measuring iPEEP closer to reality is the disconnection/connection maneuver where we measure the different Pplat before and after.5
The management of these patients is mainly based on medical therapy and non-invasive mechanical ventilation. However, if there is no clinical improvement, intubation should not be delayed.8 The different maneuvers used to adjust the ventilator are aimed at increasing expiratory time (ET)9:
–Increase the I:E ratio.
–Low respiratory rate and tidal volume allow hypercapnia. However, special attention should be paid to cases of neurocritical patients or reduced myocardial contractility.
–Increased inspiratory flow without exceeding 50 cmH2O of peak pressure and less inspiratory hold.
Expiratory time constant (RCEXP) is the product of lung compliance and airway resistance. Proper ET is, at least, 3 times RCEXP. However, if <2 times then there is a risk of hyperinflation. Patients with obstructive pulmonary diseases have regional differences regarding mechanical properties and this heterogeneity prevents the use of a single RCEXP for the entire lung.10
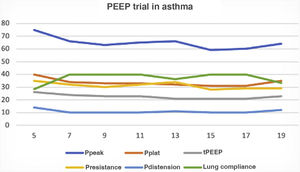
Another therapeutic parameter is extrinsic PEEP (ePEEP) that traditionally should be 80% of iPEEP. However, since the maneuvers used to measure iPEEP do not take hPEEP into consideration, as it is the case with restrictive disease, a PEEP trial is required to know what ePEEP is the right one to keep the airway opened and allow lung emptying. Pplat and/or total PEEP can be measured while ePEEP is going up at a ratio of 2 cmH2O/min. When, after increasing ePEEP we can see that Pplat or total PEEP do not go up or do so <2 cmH2O, this is indicative that lung emptying is happening (Fig. 1). Another beneficial effect of ePEEP in the presence of spontaneous breathing is that it reduces work of breathing and the appearance of asynchronies.3
Trial to know optimal PEEP in patient with flow obstruction. We can see how, after increasing extrinsic PEEP from 5 cmH2O up to 19 cmH2O (abscise axis), no significant increase of plateau pressure, total PEEP or less lung compliance can be seen up to 17 cmH2O this being the most adequate PEEP. Pdistension, distension pressure; Ppeak, peak pressure; Pplat, plateau pressure; Presistance, resistance pressure, tPEEP, total PEEP.
The target of adjusting mechanical ventilation in patients with obstructive pulmonary diseases is to increase ET and perform a PEEP trial after individualizing each particular case.
Conflict of interestNone.