The first generation of mechanical ventilators were controlled and cycled by pressure. Unfortunately, they did not allow control of the delivered tidal volume under changes in the dynamics of the respiratory system. This led to a second generation of ventilators that allowed volume control, hence favoring the ventilatory strategy based on normalization of the arterial gases.
Studies conducted in the 1980s which related lung injury to the high ventilator pressures utilized while treating acute respiratory distress syndrome patients renewed interest in pressure-controlled mechanical ventilation. In addition, new evidence became available, leading to the development of pulmonary protective strategies aiming at preventing the progression of ventilator-induced lung injury.
This review provides a detailed description of the control of pressure or volume using certain ventilatory modes, and offers a general view of their advantages and disadvantages, based on the latest available evidence.
En su primera generación los ventiladores fueron controlados y ciclados por presión. Lamentablemente no nos permitían asegurar el volumen suministrado ante variaciones de la impedancia respiratoria. Esto dio paso a una nueva generación que logró asegurar el volumen y favorecía la estrategia ventilatoria de normalización de los gases en sangre.
Estudios realizados durante los años 80 hicieron renacer el interés en la ventilación controlada por presión en pacientes con síndrome de distrés respiratorio agudo al relacionar las altas presiones inspiratorias con la injuria pulmonar. Estos hallazgos, sumados a la aparición de una nueva evidencia, dieron paso al desarrollo de una nueva estrategia ventilatoria protectora del pulmón tendiente a evitar la progresión del daño pulmonar.
Esta revisión pretende ofrecer una descripción detallada sobre cómo se realiza el control de la presión o el volumen en ciertos modos ventilatorios y brinda una visión general de sus ventajas y desventajas basadas en la última evidencia disponible.
The first ventilators used on a large scale in Intensive Care Units (ICUs) were introduced in the 1960s and were controlled and cycled by pressure. In those days the main objective of mechanical ventilation was to normalize the blood gases, and since these machines were unable to guarantee a stable tidal volume (Vt) or minute volume (Vmin) in the face of changing respiratory dynamics, other alternative system designs were explored.
Volume controlled ventilators were introduced in the early 1970s, and were regarded as more adequate for the management of a devastating respiratory disorder also described in that same period. In effect, “adult” respiratory distress syndrome (ARDS), as it was initially called, remains a challenge both for therapists and for the equipment used. The use of volume controlled ventilators proves ideal in the case of a disease with changing respiratory mechanics and the need to guarantee Vmin. In order to normalize the arterial blood gases it was very common to use volumes of up to 15ml/kg current weight–this giving rise to iatrogenic effects which in the light of posterior evidence proved more than evident.
In the 1980s,1–3 and due to evidence of the damage caused by the high pressures needed to ventilate these patients, renewed interest became focused on pressure controlled modes, and changes in ventilation strategies were made, accepting a degree of blood gas anomalies in order to protect the lungs from excessive pressures. The evidences that continuously emerge regarding the best way to protect the lungs have cast new light on the lung protecting strategies. However, it remains unclear whether it is best to ventilate the patient under either pressure or volume control. This has generated much debate, and no global consensus has been established regarding which ventilation mode is safer and more efficient.
A mechanical ventilator is simply a machine designed to alter, transmit or direct applied energy in a predetermined way, with a view to assisting or replacing the natural function of the respiratory muscles.
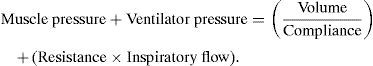
In order to understand how this is done, we use models of respiratory mechanics. These models illustrate and simplify the relationships between the variables of interest. Specifically, we are interested in the pressure needed to direct the gas flow toward the airway and to inflate the lungs. This mathematical model relating pressure, volume and flow during ventilation is known as the “equation of the dynamics of the respiratory apparatus”.4–6
This model has two basic functions in mechanical ventilation:
- 1.
Calculation of the lung resistance and distensibility (compliance) values based on prior data referred to pressure, volume and flow. This is used by the ventilators to monitor the condition of the patients during evolution of the disease or their response to treatment.
- 2.
Prediction of pressure, volume and flow based on the lung resistance and compliance data. This function constitutes the basis of ventilator control theory and of the recently proposed classifications.7
The most significant revelation of the equation of the dynamics of the respiratory apparatus is that any ventilator we can imagine is able to control only one variable at the same time during inspiration (control of pressure or volume or flow, but not two variables simultaneously). This greatly facilitates our understanding of how ventilators work, in the same way as the fact that volume and flow are inversely related (flow being the derivative of volume, and volume the integral of flow). We consequently only refer to ventilators controlled by pressure or by volume.8 Thus, ventilators can be viewed simply as machines that control the waveform of the pressure curve or of the volume curve.9 We therefore refer to pressure or volume as the “control variable”. The latter could also be referred to as the “independent variable”, since it is not modified by changes in lung compliance or resistance (respiratory impedance of the system), while the other variable does undergo changes and therefore represents the “dependent variable”.
In order to establish which is the control variable, we need to evaluate the pressure/time and volume/time curves.
PressureWhen pressure is controlled in ventilation mode, the waveform of the pressure/time curve remains unchanged in response to variations in the respiratory impedance of the system. In contrast, the volume/time and flow/time curves undergo changes in both waveform and values (e.g., Vt and peak inspiratory flow (PIF)).
On controlling pressure, the left side of the equation reflecting the dynamics of the respiratory apparatus is determined by programming of the ventilator. A ventilator that controls pressure can do so in two ways:
- 1.
Controlling pressure at body surface level, causing the latter to descend with respect to the airway pressure during inspiration. Such systems can be classified as “negative pressure ventilators” (e.g., iron lung).
- 2.
Controlling pressure at airway level, causing the latter to increase to above the pressure at body surface level during inspiration. Such systems can be classified as “positive pressure ventilators”. The present review only addresses these positive pressure systems, which are the ventilators we use in daily clinical practice.
When volume is controlled in ventilation mode, the waveform of the volume/time and inspiratory flow/time curves remain unchanged in response to variations in the respiratory impedance of the system. In contrast, the pressure/time curve undergoes changes in both waveform and values (e.g., peak inspiratory pressure (PIP)).
Ventilators that control volume measure the latter directly either from the displacement of a piston or bellows mechanism, or through calculation based on the inspiratory flow signal. Ventilators such as the NPB 840, Servo-i, and Neumovent Graphnet, display the volume values, but all of them currently measure and control inspiratory flow and calculate volume as reported information. Therefore, while technically correct, all of them are actually “flow controllers”.9
While this distinction is important from the engineering perspective and for understanding ventilator operation at the patient bedside, such differentiation between the control of volume or flow does not appear to be relevant.
Definitions and technical descriptionsDefinition is required of a series of important concepts allowing us to better understand the difference between pressure or volume control in a given ventilation mode.
A ventilation mode is a predetermined pattern of interaction between the patient and the ventilator. A well defined mode must provide information on a specific combination of control, phase and conditional variables established for both mandatory or spontaneous respirations, or a combination of both. The absence of part of this information can give rise to confusion among professionals, alter the ventilatory strategies, and place the patient at risk.
The “phase variables” describe the events that take place within a ventilatory cycle (in any of the possible ventilation sequences), and thus afford increased information regarding a given mode. A ventilatory cycle can be divided into four phases: 1. Transition from expiration to inspiration; 2. Inspiratory phase; 3. Transition from inspiration to expiration; 4. Expiratory phase. In each phase a variable is measured and used to start, develop and end the phase. “Trigger variable”: all ventilators measure one or more variables or signals associated with the equation of the dynamics of the respiratory apparatus, and the inspiratory phase is started when the variable reaches a predetermined value. During the inspiratory phase, pressure, flow and volume increase to above their values at the end of expiration. This stage takes place over a period of time that can be directly programmed or not, and which can be fixed or variable. It is in this stage when the “control variable” exerts its action. On the other hand, a variable that does not increase beyond a prefixed value during inspiration and which is not used for terminating inspiration is referred to as a “limited variable”. By definition, on controlling a variable we are effectively limiting it. The “cycling variable” in turn is a variable which upon reaching a predetermined value ends the inspiratory phase, thereby giving rise to the start of expiration (phase 3). To this effect the variable must be measured and used as feedback signal. During the expiratory phase, the ventilator returns to the level specified by the “base variable”, which is the variable controlled during expiration, and is generally referred to as the end-expiratory pressure or PEEP (peak end-expiratory pressure).
Ventilation sequencesThere are three ventilation sequences7 reflecting the possible combinations between mandatory and spontaneous respirations, as specified below:
Continuous mandatory ventilation (CMV), in which all respirations are mandatory, i.e., spontaneous breathing is not allowed. The term CMV encompasses all respirations, whether started by the machine (controlled) or by the patient (assisted), and terminated or cycled by the machine in either case. In CMV we program a minimum frequency (FR), though this can be increased by the patient.
Continuous spontaneous ventilation (CSV), in which all respirations are started and ended by the patient. These can be pressure supported (pressure supported ventilation (PSV)) or not (continuous positive airway pressure (CPAP)). There are no mandatory respirations, and FR is determined by the patient.
Synchronized intermittent mandatory ventilation (SIMV), characterized by a combination of mandatory and spontaneous respirations. Only FR of the mandatory respirations is programmed, and between them the patient can breathe spontaneously and increase the total FR.
Before each breath, the ventilator must establish a specific pattern of “control variables” and “phase variables”. The decision regarding the pattern or profile to be applied is established by means of the “conditional variables”. This pattern is kept constant in the ventilation sequences such as CMV and CSV; therefore, use is made of the same “control variable” in all the respirations. However, in contrast to CSV, in CMV we can choose between pressure control or volume control, while in the case of CSV we can only control pressure, since this is a spontaneous mode in which the patient decides the inhaled Vt–not the machine. On the other hand, since SIMV is a combination of mandatory and spontaneous respirations, the ventilator must decide when to introduce a different pattern for each of them. Therefore, in SIMV we must select a control variable for the mandatory respirations (pressure or volume), while in the case of spontaneous respiration, pressure will always be the controlled variable. This shows that different control variables may coexist in SIMV (e.g., volume in mandatory respirations and pressure in spontaneous respirations, or alternatively pressure can be the controlled variable in both types of respirations).
ControlConfusion has gradually grown in the field of mechanical ventilation due to the many different names used by the manufacturers in referring to the ventilation modes, and because of the persistent use of poorly defined or wrongly applied terms that only contribute to increase the confusion.
The word “control” is and has often been used in mechanical ventilation to describe aspects of ventilation and/or of the patient, and this sometimes means that it is not quite clear what we are controlling. In many cases the term “control” can cause the health professional to think of “controlled ventilation”, in which the patient is paralyzed by neuromuscular blockers, and patient interaction with the ventilator is avoided. In this case the ventilator takes full “control” of the aspects relating to ventilation, instead of the patient.
We can also find “control” on the ventilation mode selection display, under the term “Assist/Control” (A/C). The term A/C means that in this mode respiration can be started by the patient (the ventilator responds by “assisting” patient inspiratory effort) or by the machine (which controls the start of patient ventilation when the patient fails to do so). However, also in SIMV, respiration can be started by both the patient and the machine (in the same way as any other ventilation mode lacking a CSV sequence); consequently, we are technically unable to differentiate these two modes. Because of this, A/C should be replaced by continuous mandatory ventilation (CMV), in which each respiration can be activated by the patient or by the machine at the programmed FR, and information is moreover provided on the ventilation sequence (A/C does not afford such information). Unfortunately, the term A/C, while technically erroneous, is still used today by many ventilators.
We will now examine the word “control” included under the term “control variable”, and which specifies the variable which the ventilator uses as feedback signal for controlling inspiration. It should be explained that on talking about pressure or volume controlled ventilation modes, these are not ventilation modes in themselves (they neither define nor specify the mode); rather, they simply inform us of the variable controlled during inspiration in a ventilation mode, but not of which mode, since both pressure and volume can be controlled in sequences such as CMV or SIMV. Therefore, in order to define and refer to a given ventilation mode, we must jointly cite the “control variable” and the “respiratory sequence” (e.g., V-CMV or P-CMV, V-SIMV or P-SIMV). We can also further define SIMV in the same way (e.g., V-SIMV+PS or P-SIMV+PS).
Another application of the word “control” is found in the term “dual control”, which has given rise to the “dual modes” classification. Although we have already mentioned that the ventilator can control pressure or volume during inspiration, but not both at the same time, such “dual control” can shift from one variable to the other during an inspiration. This is the case of modes that start an inspiration controlling the pressure and which switch or shift to volume control (or vice versa) on predicting that the proposed or desired objective will not be reached. Some authors also use the term “dual control” to include the pressure adjustments made in different successive respirations to approach a proposed or desired volume. Although pressure always remains a “controlled variable”, automatic adjustments of this pressure level are made but “volume is never controlled”; rather, the intended objective is to come as close as possible to it–and in some situations this is not achieved. The above leads us to underscore another possible mistake in the use of the word “control”, as included under the term Pressure Regulated Volume Control (PRVC) mode, in which (as explained above) “volume is never controlled”, and the only control variable is pressure.10
Volume-controlled ventilationSince there are two modes in which we can control volume, i.e., V-CMV and V-SIMV, it must be mentioned that the present review focuses on V-CMV, also known as V-A/C (volume assist-control).
When using V-CMV we must program Vt, FR, the way in which Vt is administered, and the rest of programmings common to other ventilation modes such as PEEP and FiO2, including the alarms.
On selecting Vt, we determine that it will be administered in each mandatory respiration, and we designate volume as the “control variable”. In this case volume will be the “independent” variable, and Vt will be maintained independently in the event of changes in respiratory system resistance and compliance, or changes in patient inspiratory effort.
When volume is controlled, pressure becomes the “dependent” variable. Thus, an increase in respiratory impedance will result in an increase in airway pressure. A decrease in thoraco-pulmonary compliance or an increase in resistance in any part of the system (water in the tubing, tubing compression, water-saturated heat-moisture exchangers (HMEs), secretions in the endotracheal tube (ETT) or in the airway, bronchospasm or activation of the expiratory muscles (cough)) can be the cause.
An increase in distensibility or a decrease in resistance gives rise to a drop in PIP, which may even become negative in the case of major inspiratory effort or exertion on the part of the patient.
Mention is made below of how Vt is administered by programming the peak inspiratory flow (PIF), the waveform of the inspiratory flow or the inspiratory time (Ti). These parameters can be very important for determining the distribution of Vt within the lungs, the mean airway pressure (MAP), and patient tolerance and comfort under mechanical ventilation. Although all of these variables are related, not all of them are available for programming by the different types of ventilators. Some ventilators offer the possibility of selecting peak flow and the waveform of the inspiratory flow–the most common nowadays being the “constant” (rectangular) and “descending ramp” (wrongly called decelerating) waveforms. Ti is mathematically determined as a function of Vt and the inspiratory flow waveform, and PIF. other ventilators offer the possibility of programming Ti and the flow waveform, while inspiratory flow is calculated mathematically according to the programmed Vt.11
There is debate regarding the best inspiratory flow waveform. It is generally accepted that a “descending ramp” flow waveform is more closely associated with a better distribution of Vt, a lower PIP, better patient tolerance or comfort, and lesser respiratory effort or work of breathing (WOB). The algorithms for decreasing inspiratory flow differ among the different models of ventilators, and some of them can offer different “descending ramp” forms. It should be noted that when a healthy individual breathes against resistance, his or her inspiratory flow shows a “descending ramp” waveform. On switching from “constant” flow to a “descending ramp” waveform, Ti increases and the expiratory time (Te) consequently shortens, and PIP likewise decreases. Switching in the opposite sense in turn implies inversion of these effects. We generally think that volume-controlling modes cycle by “volume”, but this is incorrect, since on programming volume and the way of administering the inspiratory flow, we are determining the time which the machine will take to administer Vt; consequently, these modes cycle by “time”. For the correct selection, evaluation and adjustment of inspiratory flow, use can be made of the “pressure/time” chart.
A major limitation of volume control is the fact that administration of the inspiratory flow in each respiration is fixed in its values, and if the patient is active, he or she may have a variable inspiratory demand, generating “dyssynchrony due to inadequate inspiratory flow” or also a “double trigger” effect in requiring a volume larger than the programmed volume. In addition, volume can more easily be directed toward areas of lesser resistance or increased compliance, thereby producing “overdistended areas”.
The main alarms in relation to volume control are the “maximum pressure alarm”, alerting us of increased PIP; the “minimum pressure alarm”, which alerts us of inadequate inspiratory flows; and FR, which informs us of a very active patient and the possibility of generating auto-PEEP. Programming of the alarms must be adjusted according to the policies of each institution.
The greatest advantage of volume control is that the operator exercises direct control upon Vt and minute-ventilation. However, alveolar ventilation (AV) can decrease in the event of a drop in mandatory FR, a decrease in Vt, or an increase in dead space (Vd), whether mechanical or alveolar.
Pressure-controlled ventilationSince there are different modes in which we can control pressure, such as P-CMV (P-A/C), P-SIMV+PS, PS, PRVC, etc., it is necessary to point out that only P-CMV will be addressed below.
When using P-CMV, we must program the limiting or maximum pressure, the inspiratory time (Ti), FR and the rest of values common to other modes such as PEEP level, FiO2 and the alarms. All these initial parameters can subsequently be adjusted to optimize ventilation according to the ventilation strategy we wish to use.
On programming the limiting or maximum pressure, the latter will be administered in each mandatory ventilation during the programmed Ti, and so it is designated as the “control variable”. Pressure is the “independent variable”, and will be maintained constant and independent of changes in compliance, resistance and patient inspiratory effort. During pressure-controlled ventilation, volume is the “dependent” variable, and there can be substantial variations in Vt due to changes in resistance or compliance of the respiratory system, or in the inspiratory effort of the patient. Reductions in compliance or increased resistance of the airway will lower the administered Vt. An increase in compliance, a drop in resistance, or an increase in patient inspiratory effort will increase Vt.
When using pressure control modes, the ventilator produces the flow needed to quickly reach the limiting pressure and maintain it during the programmed Ti. The inspiratory flow waveform is “exponentially decreasing” (wrongly called decelerated, for although the gas molecules decelerate, flow does not). At present, most ventilators allow us to set the time the machine takes to reach the programmed limiting pressure, causing it to do so either more quickly or more slowly. This option is found on the parameters selection display as “Rise time”. It should be mentioned that if we wish to pressurize the system more quickly, the rise time must be shortened. This maneuver is sometimes referred to as “increasing the rise time”, which tends to produce confusion. The angle or slope of the decrease in inspiratory flow will depend on the respiratory system impedance or resistance and on patient effort. It should be noted that the flow is variable in its values but not in Ti, which remains fixed. Therefore, P-CMV cycles by time, and only some ventilators offer us the possibility of cycling by flow. In order to set the correct Ti, we can resort to the flow/time chart and select the Ti needed for inspiratory flow to reach the baseline.
The greatest limitation of pressure control modes is the variations in Vt that occur in the case of changes in impedance. Consequently, pressure control is not the best choice when we wish to control PCO2 or Vmin. Since this mode is characterized by a fixed Ti, any increase in FR without adjusting Ti can produce not only dyssynchrony but also auto-PEEP and its adverse effects. The combination of excessive inspiratory efforts with high pressures can also generate a large Vt, and this may give rise to lung injury.
The main alarms during pressure-controlled ventilation are minimum Vt, which alerts us of a worsening of impedance and the consequent hypoventilation. The maximum Vt alarm in turn informs us of possible alveolar overdistension. The low Vt and high FR alarms alert us of changes in the patient and the need for evaluation of the latter, with adjustment of the parameters. Likewise, the alarms referred to Pmin and Pmax alert us of maintenance of the programmed pressure level. As in the case of volume-controlled ventilation, programming of the alarms should be adjusted according to the policies of each institution.
An important advantage of pressure-controlled ventilation is that the more normal areas of the lung can be protected from overdistension through limitation of the inspiratory pressure–though this is only relative, since regional lung volume is more dependent upon transpulmonary pressure than on airway pressure. Another important advantage of the pressure-controlled mode may be improved comfort for the patient, who breathes spontaneously, since the ventilator can administer variable peak inspiratory flows and flow waveforms–adapting better to the variations in inspiratory effort of the patient, and thus improving synchrony between patient and machine.12
Volume-controlled ventilation versus pressure-controlled ventilationSurely at this time, and applying the principles of evidence-based medicine, it cannot be claimed or affirmed that any given technique is better than the rest, at least under all circumstances. The benefits depend on the type and clinical situation of the patient, the available equipment, and the preferences and knowledge of the medical and nursing personnel attending the patient. In general, it may be affirmed that PCV could offer advantages particularly in two situations: (1) patients requiring a protective ventilation strategy with strict pressure limitation; and (2) patients with poor adaptation to ventilatory support. In any case, the decision always must be individualized and based on the mentioned factors.
Why did such controversy arise between VCV and PCV? In fact, it was due to three factors:
- •
The old respirators comprised a gas emission system that generated turbulent flow in the pressure-controlled techniques.
- •
It was believed that pressure-controlled methods are less safe (on the grounds that they do not ensure Vt in each respiration).
- •
The old aims of mechanical ventilation favored the use of volume-controlled techniques, since the fundamental objective of mechanical ventilation were the same as those of spontaneous ventilation, i.e., to guarantee a Vmin affording adequate oxygenation and a normal PCO2 level.13
Worldwide epidemiological studies of mechanical ventilation have found VCV to be the ventilation mode most frequently used throughout the duration of patient ventilatory support (reaching 60% of the total mechanical ventilation time). In addition, it has been shown that this frequency of use persists independently of the disease of the patient (in both patients with chronic obstructive pulmonary disease (COPD) exacerbation and in acute respiratory distress syndrome (ARDS)).14
However, the current recommendations for optimum mechanical ventilation include a lung protecting strategy limiting Vt to below 10ml/kg ideal body weight, transpulmonary pressure to 35 cmH2O and lung distension pressure to under 20 cmH2O, and contemplates the application of early and aggressive PEEP to maintain lung volume at the end of expiration.15 The aim of this strategy is to ensure adequate (not necessarily normal) gas exchange, minimize barotrauma and volutrauma of the lungs, avoid hemodynamic deterioration and protect right ventricle function, prevent biotrauma and expansion of the lung injury, and at the same time contribute to minimize the patient sedation needs.16,17 These objectives are possibly easier to reach with pressure-controlled methods, or at least with the use of decelerated and variable flow patterns.
The beneficial effects of PCV include the lowering of peak inspiratory pressure (PIP) associated with overdistension phenomena of the ventral and apical regions of the lungs. In addition, oxygenation is improved–this being particularly useful in situations of severe hypoxemia. Such improvement in oxygenation is a consequence of improved gas distribution within the alveolar spaces.18,19
Many clinicians are unwilling to accept variable Vt in PCV despite the benefits referred to oxygenation and lung mechanics. However, randomized studies in patients with acute respiratory distress syndrome (ARDS) have shown control of plateau pressure and Vt to be similar, independently of whether volume- or pressure-controlled modes are used. This has led to the development of dual ventilation modes designed to obtain a given Vt and at the same time limit the pressure. These modes have been publicized as an innovation, but in fact they offer clinicians the option of administering VCV with a descending ramp flow.
Inadequate programming of inspiratory flow during VCV can impose great work of breathing (WOB) upon patients. It is very important for the inspiratory flow of the ventilator to equal or at least come close to the flow demanded by the patient. Since patient inspiratory demand can vary from breath to breath, any predetermined inspiratory flow (referred to both waveform and peak flow) can substantially affect patient WOB. During PCV the flow is decelerated and fundamentally variable; thus, if patient demand increases at any point during inspiration, the measured pressure drops to below the programmed pressure, and instructs the ventilator to increase flow with the purpose of maintaining the programmed pressure. This autoregulatory nature of the inspiratory flow administered by the ventilator during PCV can offer advantages in patients with variable respiratory demands.
Another form of patient WOB which is sometimes overlooked refers to expiratory muscle activation. Expiration should be passive even under mechanical ventilation. Active expiration can be caused by inadequate programming of Ti and PEEP, or by the use of an inspiratory pause. The original PCV modes required the expiratory valve to be closed throughout Ti. If the patient wished to cough or exhale, the airway pressure increased to the maximum pressure alarm level, thereby ending inspiration before completing the stipulated Ti. The new ventilator designs incorporate a “floating valve” allowing the patient to exhale within Ti. The pressure objective and programmed inspiratory pressure are maintained through manipulation of the inspiratory and expiratory valves.
Improving the tolerance of mechanical ventilation through modes that control or limit pressure can contribute to lessen the need for sedation and neuromuscular blockers, thereby facilitating earlier spontaneous ventilation on the part of the patient and ultimately shortening the number of days on mechanical ventilation and the duration of stay in the Intensive Care Unit (ICU).
The only randomized study20 in patients with ARDS comparing VCV and PCV within the context of a lung-protecting ventilation strategy showed pressure control to afford safe maintenance of the ventilation parameters and pH levels. This same study also recorded a decrease in the incidence of multiorgan failure over time. Unfortunately, failure in randomization of the study, affecting the results of its multivariate analysis, precludes generalization of the results–though possibly a similar study ought to be repeated at the present time.
In conclusion, both types of ventilation control offer some advantages fundamentally derived from improved control of the parameters in the volume-controlled modes and improved adaptability to the patient in the case of the pressure-controlled modes. However, the efficacy of the latter has not been demonstrated to date in clinical studies, which on the other hand are difficult to carry out at the present time. In any case, the current recommendation possibly should be to use the ventilation mode that allows us to reach the objectives individually adapted to the clinical condition of the patient and to the existing lung mechanics in the most effective way possible.21–23 The mode of control of the parameters is not as important as their true control, possibly even in future when new monitoring modes have become introduced.24
Conflicts of interestDr. H. Abbona is the Manager of Development and Clinical Research of TECME.
Please cite this article as: Garnero AJ, et al. Modos controlados por presión versus volumen en la ventilación mecánica invasiva. Med Intensiva. 2013;37:292-8.