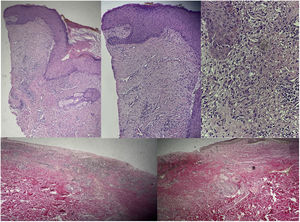
A female patient presented with type AB-B burns caused by fire, affecting 41.5% of the body surface. She suffered chronic wounds in the form of ulcerative blister lesions overlying previously traumatized skin. The lesions proved difficult to heal, were very painful, and an underlying infectious or rheumatological origin was discarded. A skin biopsy showed superficial perivascular and interstitial dermatitis with intraepithelial neutrophils and edema. Pyoderma gangrenosum was suspected based on the evolution of the wounds, with the diagnosis being established through exclusion and supported by the histopathological findings with the granulocytic infiltrate. Treatment was continued with deep subcutaneous betamethasone in donor zones, together with 0.05% clobetasol propionate, with reduction of the damaged areas and clinical improvement with healing of the ulcerations. Enteral cyclosporine was subsequently prescribed, continuing with the intralesional corticosteroid infiltrations, with complete clinical healing in 8 weeks, followed by hospital discharge and follow-up on an outpatient basis (Figure1 Figs. 1 and 2). Skin biopsy with hematoxylin-eosin and Van Gieson staining (Fig. 3): skin fragment with epidermis presenting discrete compact laminar keratosis, with hypergranulation foci and neutrophils within the horny layer. The papillary dermis presents a chronic lymphoplasmacytic inflammatory infiltrate with an interstitial and perivascular distribution. Isolated groups of granulocytes are also observed at the dermo-epidermal interface and at the superficial perivascular level.
Please cite this article as: Matute Miranda JC and Valdés Contreras CB. Pioderma gangrenoso en paciente gran quemado, Med Intensiva. 2023. https://doi.org/10.1016/j.medin.2023.08.004