Primary angioplasty is the reperfusion treatment of choice for the management of acute myocardial infarction (AMI) when performed at the right time (<120min since diagnosis) and in highly experienced centers. In multiple clinical trials, the percutaneous coronary intervention (PCI) has proven superior to fibrinolysis reducing mortality, reinfarction, and intracranial bleeding.1
Fibrinolysis is spared for cases that for whatever reason are not eligible to undergo a primary PCI. It should be performed as early as possible with fibrin-specific fibrinolytic agents2 and with immediate referral to a PCI capable center. It can be a rescue or a late (2–24h) PCI depending on whether fibrinolysis failed or not.3,4 Although primary angioplasty is successful in most cases, higher Killip-Kimbal indices at admission, multivessel disease, clinical history of AMI, and longer disease progression times are some of the main causes for a failed PCI, which is associated with a very high in-hospital mortality rate.5,6 Occasionally, specific anatomical problems can also result in failed primary PCIs.7,8 «Rescue or bailout fibrinolysis» is the treatment of choice in these patients, although medical literature says nothing on this regard.
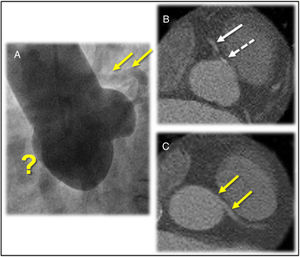
This is the case of a 55-year-old male. The patient was a former smoker but did not have any relevant personal or familial medical history. The patient experienced a sudden 1-h duration oppressive centrothoracic pain radiating to his jaw and to the interscapular region followed by cardiogenic shock with spontaneous recovery. Upon arrival to the ER, the patient was still complaining of chest pain, but he was hemodynamically stable (Killip I). The electrocardiogram (EKG) showed second-degree Mobitz I atrioventricular block (AVB), ST-segment elevation in the inferior and right precordial leads, and ST-segment depression on LI and aVL. A loading dose with adiro 300mg and clopidogrel 600mg was administered, the Infarction Code was activated, and the patient was eventually transferred to our center. An emergency coronary angiography via right radial access was performed that confirmed the presence of a left coronary tree without injuries and the anomalous origin of the left main coronary artery (LMCA), slightly above the sinotubular juncture (STJ). Yet despite the multiple attempts made with different catheters and the performance of 2 aortograms (Fig. 1) the right coronary artery (RCA) could never be seen. Considering the possibility of an anomalous origin from the left Valsalva sinus, the guidewire crossed to the left anterior descending coronary artery followed by injections of the catheter tip with different angulations. Still, the anomalous origin of this artery could not be seen, and the procedure was terminated.
A) Aortogram in the left anterior oblique projection showing the 3 Valsalva sinuses and apparent absence (?) of right coronary artery. The left main coronary artery originated above the sinotubular junction is partially filled non-selectively (arrows). B) Axial CT scan showing a calcified plaque (dashed arrow) inside the right coronary artery ostium that has already recovered the antegrade flow (arrow). C) Left coronary artery outflow tract with intra-arterial trajectory (yellow arrows).
The patient was admitted to the coronary unit and remained hemodynamically stable, yet symptoms remained as well as changes on the ECG. The emergency transthoracic echocardiogram performed showed moderate left ventricular dysfunction (left ventricular ejection fraction of 40%) with inferior septal akinesis and significant dyskinesia, right ventricular (RD) dilatation, and severe dysfunction. Three and a half hours after the onset of pain, an IV «bailout» fibrinolysis was performed with alteplase 100mg (the only fibrinolytic agent available at the hospital). During the infusion of the first bolus, the patient showed transient, asymptomatic, and advanced second-degree AVB with successful electrical pacing reperfusion data (complete normalization of the ST-segment elevation), and a significant improvement of the RV and septum contractility.
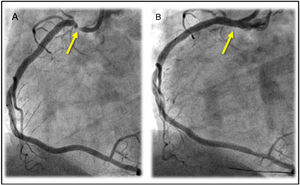
The axial cardiac CT scan performed within the first 24h revealed a serious injury in the ostial RCA slightly exiting right above the STJ. The anomalous origin of the LMCA with inter-arterial trajectory was also confirmed (Fig. 1). Then, in an elective coronary angiography performed the RCA—that was patent at that time—was selectively probed revealing the presence of a critical ostial injury where a drug-eluting stent was implanted with a positive outcome (Fig. 2). After complete revascularization, biventricular function went back to normal, and the patient was discharged from the hospital without further complications.
Although primary PCI is a very effective therapy for most patients with AMI, the possible complications and limitations should be studied carefully because, though rare, have higher morbidity and mortality rates.5,6 Exceptionally, the culprit vessel cannot be identified. This can happen when the occlusion of a coronary branch does not clearly show a stump9 or in ostial occlusions like the case presented here. Coronary abnormalities can also pose a significant challenge in this setting where selectively probing and the recanalization of the culprit artery should be performed urgently.10 Fibrinolysis is a fast, easy, and effective therapy that is undoubtfully beneficial if performed early.1 Although the «bailout PCI» strategy has been extensively described in the medical literature for cases of failed fibrinolysis,3 as far as we know, there are no accurate descriptions for the use of the «rescue or bailout fibrinolysis» after a first failed PCI. In our patient, the bailout or rescue fibrinolysis achieved the immediate vessel reperfusion with obvious clinical, ECG, and echocardiography improvements. Therefore, it is important to remember that even highly experienced hospitals that also have the necessary infrastructure to perform primary PCIs should always have fibrinolytic drugs of choice available for the management of AMI.
Conflicts of interestNone reported.
Please cite this article as: Alvarado Casas T, Diego Nieto G, Rojas González AM, Antuña Álvarez P, Rivero Crespo F, Alfonso F. «Fibrinólisis de rescate» tras angioplastia primaria fallida. Med Intensiva. 2021;45:187–189.