Infection due to the SARS-CoV-2 coronavirus, which causes COVID-19, tends to predispose patients to hypercoagulability, with an increased risk of thrombotic disease of a multifactor origin. In view of the need to establish a series of recommendations for the management of coagulation disorders in severe COVID-19 patients, the working groups of the Spanish Society of Anesthesia-Resuscitation and Pain Therapy (Sociedad Española de Anestesiología-Reanimación y Terapéutica del Dolor [SEDAR]) and the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias [SEMICYUC]) decided to join our forces and knowledge and develop a consensus document with the aim of providing guidelines for dealing with these patients. As the result of intense work, with the posterior participation of review committees from both Societies, a manuscript was developed that has just been published by the Revista Española de Anestesiología y Reanimación (REDAR).1 For different reasons unrelated to the authors, joint and simultaneous publication in Medicina Intensiva has not been possible. We believe that the most important aspect of any article – and particularly of a consensus document – is its diffusion for knowledge and subsequent clinical application in those cases where it is indicated. We therefore would like to highlight some essential aspects of the mentioned document (Fig. 1), and invite those readers who are interested to consult the full open-access original on the website of the REDAR.
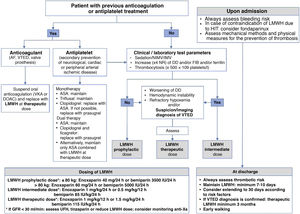
Schematic representation of the recommendations for the management of anticoagulants and antiplatelet drugs in severe COVID-19 patients.
ASA: acetylsalicylic acid; DOAC: direct oral anticoagulant; AVK: anti-vitamin K; DD: D dimer; VTED: venous thromboembolic disease; AF: atrial fibrillation; GFR: glomerular filtration rate; FIB: fibrinogen; LMWH: low molecular weight heparin; UFH: unfractionated heparin; NR: normal range; HIT: heparin-induced thrombocytopenia; IMV: invasive mechanical ventilation; NIMV: noninvasive mechanical ventilation.
Thrombotic risk in COVID-19 patients:
- -
Assessment of thrombotic and bleeding risk is recommended in all COVID-19 patients in which the seriousness of the disease requires admission to hospital.
- -
Thrombophylaxis is recommended in all admitted patients, with low molecular weight heparin (LMWH) being the drug of choice.
- -
In those patients in which a procoagulant profile is confirmed, elevation of the LMWH dose from prophylactic (40-60 mg sc/24 h) to intermediate levels (100 IU/kg/24 h) is suggested, particularly in patients admitted to the Intensive Care Unit (ICU) and subjected to mechanical ventilation.
- -
Elevation of the LMWH dose from intermediate to therapeutic levels (150 IU/kg/24 h or 100 IU/kg/12 h) is suggested in those cases where pulmonary thromboembolism is suspected (e.g., sudden worsening of oxygenation or a sharp and unexplained drop in blood pressure) and no firm diagnosis can be established.
- -
Testing to confirm pulmonary thromboembolism is recommended in suspect cases due to progression of the hemostatic parameters (fundamentally D dimer) or on the basis of the clinical course of the patient, whenever possible. If confirmation is established, anticoagulation with LMWH is recommended as standard treatment.
Adjustment of anticoagulant and antiplatelet medication:
- -
The maintenance of anticoagulation is recommended where required, preferably prescribing LMWH at therapeutic doses.
- -
The maintenance of antiplatelet treatment is recommended, administering acetylsalicylic acid in those patients where needed, and it is advisable to replace clopidogrel with prasugrel in those cases requiring dual therapy.
Interpretation of the hemostasis tests:
- -
It is advisable not to administer hemostatic agents to correct the coagulation test data in the absence of significant bleeding.
- -
In situations of active bleeding, when the administration of hemostatic agents proves necessary, the use of plasma as first choice is suggested versus prothrombin complex concentrates, due to the lack of experience and safety data.
- -
Routine protocols for the management of bleeding are recommended in COVID-19 patients with severe acute hemorrhage.
We would like to end by underscoring the importance of the early detection and optimum management of hemostatic disorders in severe COVID-19 patients. In our opinion, the establishment of consensuses endorsed by scientific societies allows a better approach to patient management, and should be promoted whenever possible.
Please cite this article as: Llau JV, Ferrandis R, Sierra P, Hidalgo F, Cassinello C, Gómez-Luque A, et al. Consenso SEDAR-SEMICYUC sobre el manejo de las alteraciones de la hemostasia en los pacientes COVID-19 graves. Med Intensiva. 2021;45:567–568.