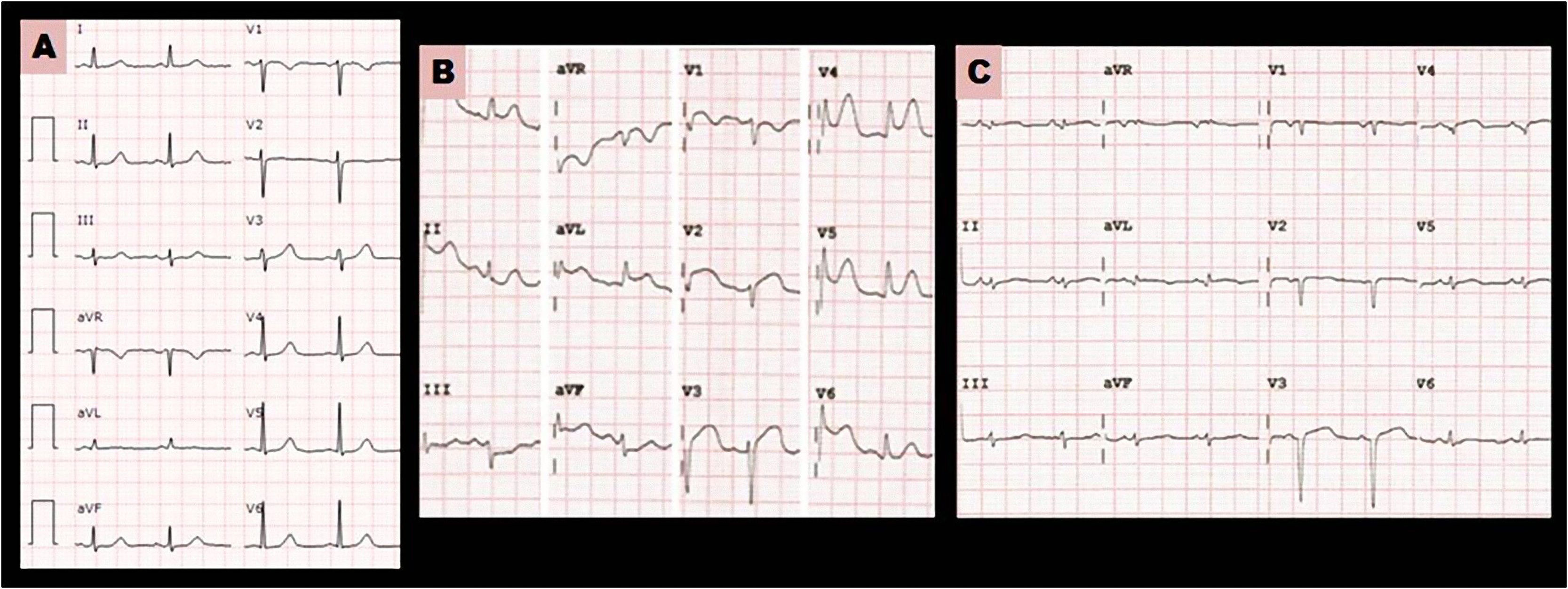
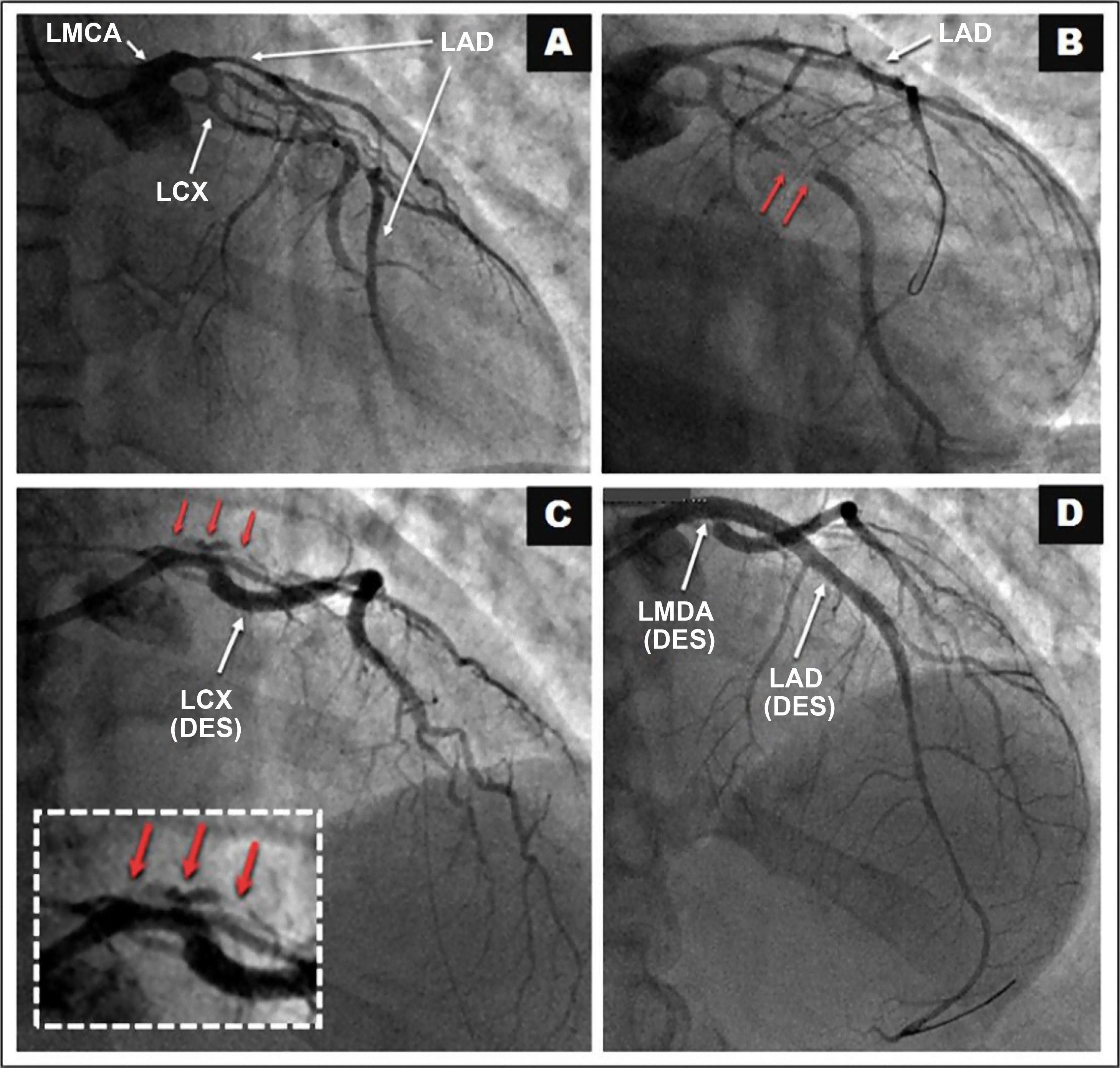
This is the case of a healthy 48-year-old woman who admitted to the intensive care unit with a diagnosis and treatment of NSTEACS following chest pain of coronary origin with a normal EKG reading (Fig. 1A), but with a positive curve of troponin I (0.13–1.15 ng/mL; normal P < 0.04); the early echocardiogram was normal. Within a few hours, the patient showed signs of angina pectoris and extensive anterolateral ST-segment elevation on the EKG (Fig. 1B). The echocardioscopy performed confirmed the presence of severe ventricular systolic dysfunction. An emergency coronary angiography was performed in situation of cardiogenic shock that confirmed the presence of a spontaneous coronary artery dissection in the left main coronary artery (LMCA) (Fig. 2A) spreading towards the middle segment of the left anterior descending coronary artery (LAD) plus the thrombotic subocclusion of the middle and proximal segments of the LAD, and middle segment of the left circumflex artery (LCX) (Fig. 2B). Given the patient’s clinical status, the percutaneous approach was indicated, and 1 drug-eluting stent (DES) was implanted into the LCX proximal-middle segments (Fig. 2C) followed by the implantation of 2 overlapping stents into the LMCA, and LAD proximal-middle segments (Fig. 2D) with good final outcome; Fig. 1C shows the control EKG.
Please cite this article as: Gentille Lorente DI, Faiges Borrás M, Moreno Ambroj C. Disección coronaria espontánea, e idiopática, del tronco coronario izquierdo en mujer joven y sana. Med Intensiva. 2022;46:177–178.