To investigate the relationship between the age of an urgently hospitalized patient and his or her probability of admission to an intensive care unit (ICU).
DesignObservational, retrospective, multicenter study.
Setting42 Emergency Departments from Spain.
Time-periodApril 1–7, 2019.
PatientsPatients aged ≥65 years hospitalized from Spanish emergency departments.
InterventionsNone.
Main variables of interestICU admission, age sex, comorbidity, functional dependence and cognitive impairment.
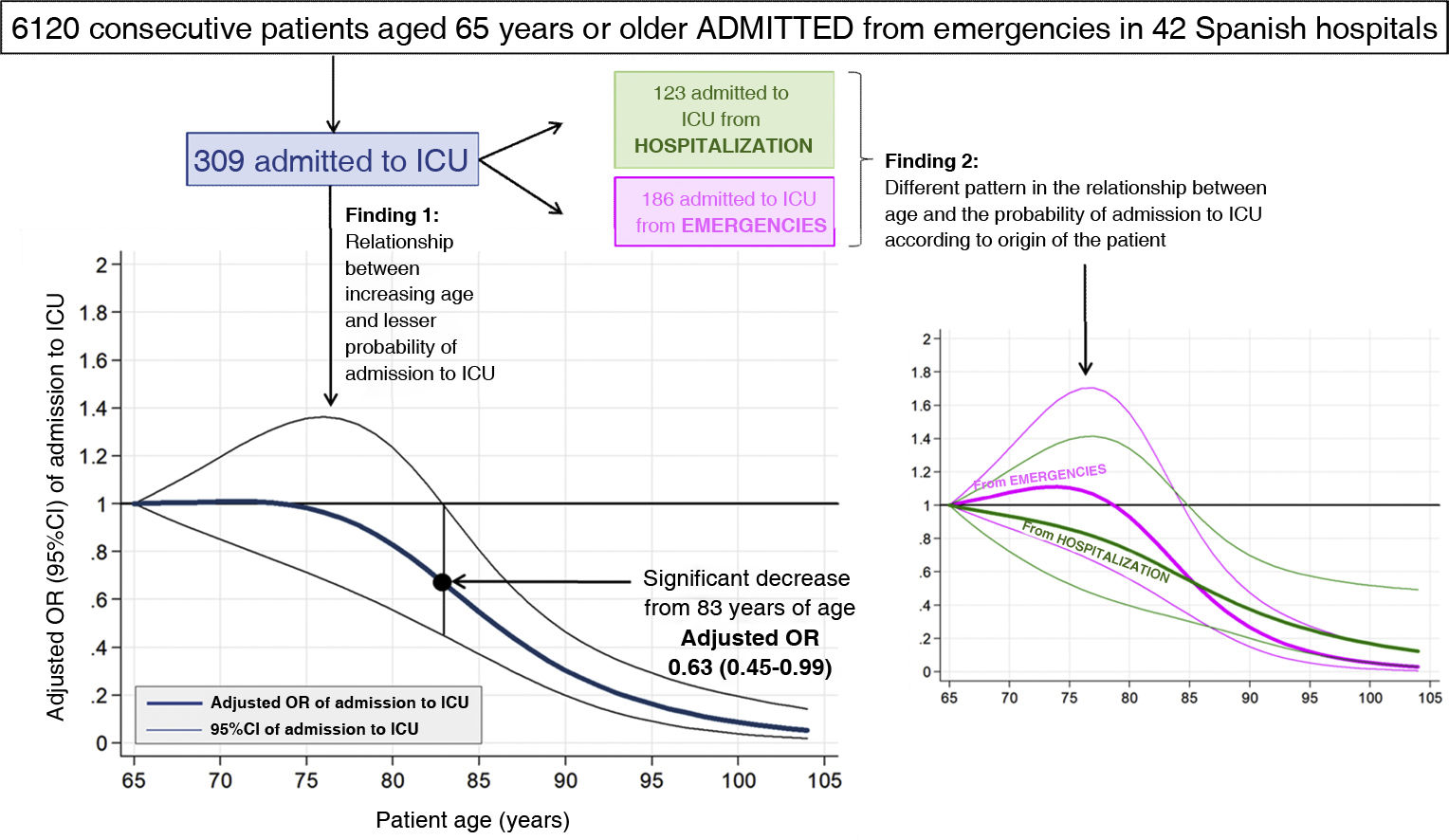
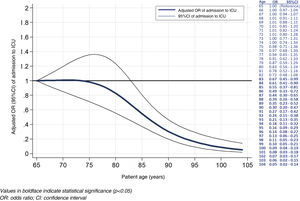
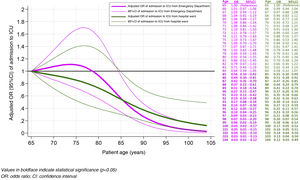
Results6120 patients were analyzed (median age: 76 years; males: 52%. 309 (5%) were admitted to ICU (186 from ED, 123 from hospitalization). Patients admitted to the ICU were younger, male, and with less comorbidity, dependence and cognitive impairment, but there were no differences between those admitted from the ED and from hospitalization. The OR for ICU-admission adjusted by sex, comorbidity, dependence and dementia reached statistical significance >83 years (OR: 0.67; 95%CI: 0.45−0.49). In patients admitted to the ICU from ED, the OR did not begin to decrease until 79 years, and was significant >85 years (OR: 0.56, 95%CI: 0.34−0.92); while in those admitted to ICU from hospitalization, the decrease began 65 years of age, and were significant from 85 years (OR: 0.55, 95%CI: 0.30−0.99). Sex, comorbidity, dependency and cognitive deterioration of the patient did not modify the association between age and ICU-admission (overall, from the ED or hospitalization).
ConclusionsAfter taking into account other factors that influence admission to the ICU (comorbidity, dependence, dementia), the chances of admission to the ICU of older patients hospitalized on an emergency basis begin to decrease significantly after 83 years of age. There may be differences in the probability of admission to the ICU from the ED or from hospitalization according to age.
Investigar la relación entre la edad del paciente urgente y la probabilidad de ingresar en la unidad cuidados intensivos (UCI).
DiseñoEstudio observacional retrospectivo multicéntrico.
ÁmbitoUn total de 42 servicios de urgencias españoles.
Periodo de estudioDel 1 al 7 de abril de 2019.
PacientesMayores de 65 años hospitalizados desde urgencias.
IntervencionesNinguna.
Variables de interés principalesIngreso en UCI, edad, sexo, comorbilidad, dependencia funcional y deterioro cognitivo.
ResultadosSe analizaron 6.120 pacientes (mediana 76 años; varones 52%; comorbilidad grave 23%; dependencia funcional 16%; deterioro cognitivo 19%); 309 (5%) ingresaron en UCI (186 desde urgencias, 123 desde hospitalización). Los ingresados en UCI fueron más jóvenes, varones y con menor comorbilidad, dependencia y deterioro cognitivo, sin diferencias entre ingresos de urgencias/hospitalización. Las odds ratio (OR) de ingreso ajustadas por sexo, comorbilidad, dependencia y demencia fueron constantes entre 65–75 años, con significación tras los 83 años (OR: 0,67; IC 95%: 0,45–0,49). Desde urgencias, las OR no descendieron hasta los 79 años, y fueron significativas en>85 años (OR: 0,56, IC 95%: 0,34–0,92). Desde la hospitalización el descenso fue a los 65 años, y significativos en>85 años (OR: 0,55, IC 95%: 0,30–0,99). El sexo, comorbilidad, dependencia y deterioro cognitivo no modificaron la asociación edad/ingreso en UCI (global, desde urgencias o desde hospitalización).
ConclusionesTras tener en cuenta otros factores que influyen en el ingreso en UCI (comorbilidad, dependencia, demencia), las posibilidades de este ingreso de pacientes mayores hospitalizados de forma urgente empiezan a descender significativamente a partir de los 83 años. Pudieran existir diferencias en la probabilidad de ingreso en UCI desde urgencias o desde hospitalización en función de la edad.
The percentage need for hospital admission among patients seen in the hospital Emergency Departments (EDs) of the Spanish public healthcare system was 10.3% in 2019, and this percentage may triple in the more elderly population.1,2 With some frequency, intensive care may prove necessary at some moment during hospital admission, particularly in patients with more serious disease conditions and with lesser functional reserves. Admission to the intensive care unit (ICU) may occur immediately after arrival in the ED, or may be decided after some days of hospital stay in a conventional ward, due to a poor patient course.
Admission to the ICU is not applied on a universal basis, and it is widely recognized that such admission must be based on criteria of severity or clinical instability, reversibility of the clinical process, the need for monitoring and intensive treatment, the patient preferences, or immediate interventions that cannot be carried outside such units.3–5 The recent COVID-19 pandemic evidenced the need to establish prioritization in accessing ICU beds, based on aspects of beneficence and nonmaleficence, as well as principles of social justice and equality.6,7 In this regard, patient age is one of the most important factors in the decision-making process, though its assessment is controversial. On one hand, advanced age is associated with a poorer prognosis, particularly in very elderly patients, while on the other hand if admission is indicated due to the rest of the patient’s circumstances, failure to admit such patients to the ICU is associated with an even poorer prognosis.8,9 Despite this, few studies have specifically analyzed the association between age and admission to the ICU when other circumstances that also intervene decisively in the decision-making process are taken into account. The present study was carried out to investigate the relationship between a patient age of ≥65 years in individuals hospitalized on an emergency basis and their probability of being admitted to the ICU, taking into account other factors of potential relevance in decision-making.10
MethodDescription of the SIESTA network and the EDEN projectThe SIESTA (Spanish Investigators in Emergency Situations TeAm) network is composed of ED professionals and seeks to address multidisciplinary research challenges in real-life clinical practice that affect Emergency Care Medicine from a multicenter perspective, and with a broad representation of Spanish EDs. The SIESTA network was created in 2020.11 Its first research challenge was represented by the COVID-19 pandemic, with the participation of 62 EDs (approximately 20% of all Spanish public EDs), and its results have recently been presented.12
The EDEN (Emergency Department and Elder Needs) challenge arises from the SIESTA network, and its primary aim is to expand knowledge about the sociodemographic, organizational, basal condition, clinical, care and evolutive aspects among the population aged 65 years or older, seen in the Spanish EDs. With this in mind, a multipurpose registry was created to include all patients seen in the emergency care setting, independently of the reason for consultation. The EDEN cohort, established for this purpose, comprises all the patients seen in 52 Spanish EDs from 14 regions (Autonomous Communities) between 1–7 April 2019. There were no exclusion criteria, and the EDs included all the patients assisted during the study period.13
EDEN-12 study designThe EDEN-12 study was specifically designed to analyze the association between the age of elderly patients requiring urgent hospitalization and the need for admission to the ICU in Spain.14
The mentioned study included all the patients of the EDEN registry requiring hospitalization and who had been assisted in hospitals with an ICU (42 of the 52 hospitals participating in the EDEN registry). In this respect, it was investigated whether there had been admission to the ICU during this index process (urgent hospitalization), directly after patient assistance in the ED or from conventional hospital wards. Patient stays in ED or other areas with intensive treatment or management resources, but without admission at any time to the ICU, were not regarded as stays in the ICU.
Apart from the variables selected for the evaluation of associations (age and admission to the ICU), we included four independent variables which a priori would be used to model the aforementioned association, and which were the gender of the patient and three variables known to influence the decision to admit a given patient to the ICU: comorbidity (assessed by the Charlson comorbidity index [CCI]),15 functional status (assessed by the Barthel index [BI]),16 and the presence of cognitive impairment. Severe comorbidity was defined by CCI≥5 points, and severe functional dependence was defined by BI<60 points. These scores were calculated from the data of the ED report and review of the clinical documents contained in the patient’s electronic health records. The diagnosis of cognitive impairment was accepted if it was explicitly mentioned in the indicated reports, though no specific scale was used to quantify the disorder.
Statistical analysisQualitative variables were reported as frequencies and percentages, while continuous variables were reported as the median and interquartile range (IQR). The chi-squared test for qualitative variables (or the Fisher exact test) and the nonparametric Mann–Whitney U-test for quantitative variables were used to detect differences in the characteristics of the patients with and without admission to the ICU, and between the patients admitted to the ICU from ED or the hospital ward.
The association between age and admission to the ICU was modeled based on logistic regression using a restricted cubic spline (RCS) to avoid imposing lineality upon the association. Three spline knots were placed in deciles 10, 50 and 90 of the marginal distribution of age, following the recommendations of Harrel.17 The magnitude of the effect of each unit change in age upon the probability of admission to the ICU was graphically displayed in the form of dose-response curves, and the association was estimated based on the odds ratio (OR) with the corresponding 95% confidence interval (CI), adjusted for gender, comorbidity (CCI), dependence (BI) and cognitive impairment. Missing values were not replaced. The age of 65 years (minimum value) was chosen as a reference for the ORs of the elderly patients in the dose-response plots. We explored whether the covariables included in the fit modified the association between age and admission to the ICU based on a first-order interaction analysis. All these analyses were repeated two more times: once only taking into account the patients admitted to the ICU from ED, and again only for patients admitted to the ICU from the hospital ward.
All hypothesis tests were two-tailed, and statistical significance was considered for p<0.05, or the 95%CIs of the ORs that excluded the value 1. Data analysis was performed using the Statistical Package for Social Sciences (SPSS) version 23.0 (IBM, Armonk, NY, USA) and Stata version 16.1 (Stata Corp., College Station, TX, USA). Some plots were generated with Microsoft Office PowerPoint version 2019 (Microsoft Corporate Office, Redmond, Washington, USA).
Ethical particularsThe EDEN project was approved by the Clinical Research Ethics Committee of Hospital Clínico San Carlos (Madrid, Spain) (protocol HCSC/22/005-E). The obtainment of informed consent was not considered necessary, given the descriptive observational nature of the study, involving no interventions of any kind. At all times, the creation of the EDEN cohort and the works generated from it have complied with the ethical principles of the Declaration of Helsinki.
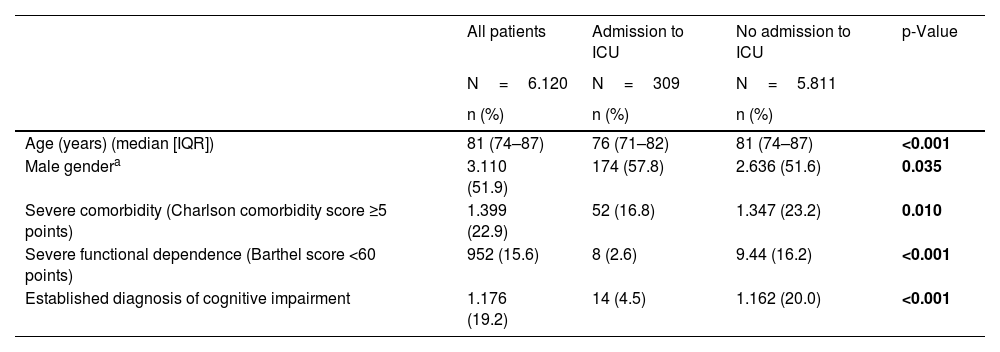
ResultsOf the 24,128 patients aged 65 years or older in the EDEN cohort from hospitals with an ICU, we analyzed a total of 6120 individuals requiring hospitalization from the ED. The median age was 81 years (IQR: 74–87), and 52% were males. Severe comorbidity was present in 23% of the cases, severe functional dependence in 16%, and 19% of the patients had a prior diagnosis of cognitive impairment (Table 1). The most frequent comorbidities were arterial hypertension (75%), dyslipidemia (52%), diabetes mellitus (35%), chronic obstructive pulmonary disease (26%), heart failure (25%), neoplasms (24%) and ischemic heart disease (21%). The median duration of hospitalization was 7 days (IQR: 4–11), and 652 patients died during this index episode (in-hospital mortality rate 10.7%).
Characteristics of the patients of the EDEN cohort included in the EDEN-12 study and comparison according to whether they were admitted to an intensive care unit or not.
| All patients | Admission to ICU | No admission to ICU | p-Value | |
|---|---|---|---|---|
| N=6.120 | N=309 | N=5.811 | ||
| n (%) | n (%) | n (%) | ||
| Age (years) (median [IQR]) | 81 (74–87) | 76 (71–82) | 81 (74–87) | <0.001 |
| Male gendera | 3.110 (51.9) | 174 (57.8) | 2.636 (51.6) | 0.035 |
| Severe comorbidity (Charlson comorbidity score ≥5 points) | 1.399 (22.9) | 52 (16.8) | 1.347 (23.2) | 0.010 |
| Severe functional dependence (Barthel score <60 points) | 952 (15.6) | 8 (2.6) | 9.44 (16.2) | <0.001 |
| Established diagnosis of cognitive impairment | 1.176 (19.2) | 14 (4.5) | 1.162 (20.0) | <0.001 |
Values in boldface indicate statistical significance (p<0.05).
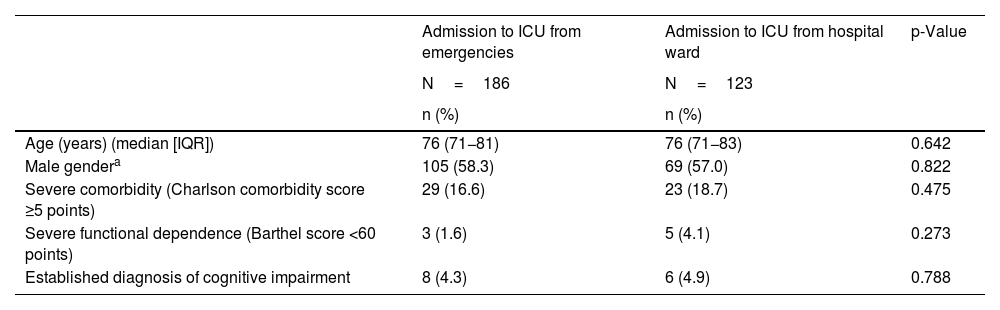
Of the 6120 patients included in the analysis, 309 were admitted to the ICU (5%): 186 were admitted after being seen in the ED and 123 required admission to the ICU during their stay in a conventional hospital ward. The patients admitted to the ICU were significantly younger and male, and with less comorbidity, dependence and cognitive impairment (Table 1). However, there were no differences in these characteristics in comparing the patients admitted from the ED versus those admitted from the hospital ward (Table 2).
Comparison of the patients admitted to the intensive care unit according to whether admission took place from the Emergency Department or from hospital wards.
| Admission to ICU from emergencies | Admission to ICU from hospital ward | p-Value | |
|---|---|---|---|
| N=186 | N=123 | ||
| n (%) | n (%) | ||
| Age (years) (median [IQR]) | 76 (71−81) | 76 (71−83) | 0.642 |
| Male gendera | 105 (58.3) | 69 (57.0) | 0.822 |
| Severe comorbidity (Charlson comorbidity score ≥5 points) | 29 (16.6) | 23 (18.7) | 0.475 |
| Severe functional dependence (Barthel score <60 points) | 3 (1.6) | 5 (4.1) | 0.273 |
| Established diagnosis of cognitive impairment | 8 (4.3) | 6 (4.9) | 0.788 |
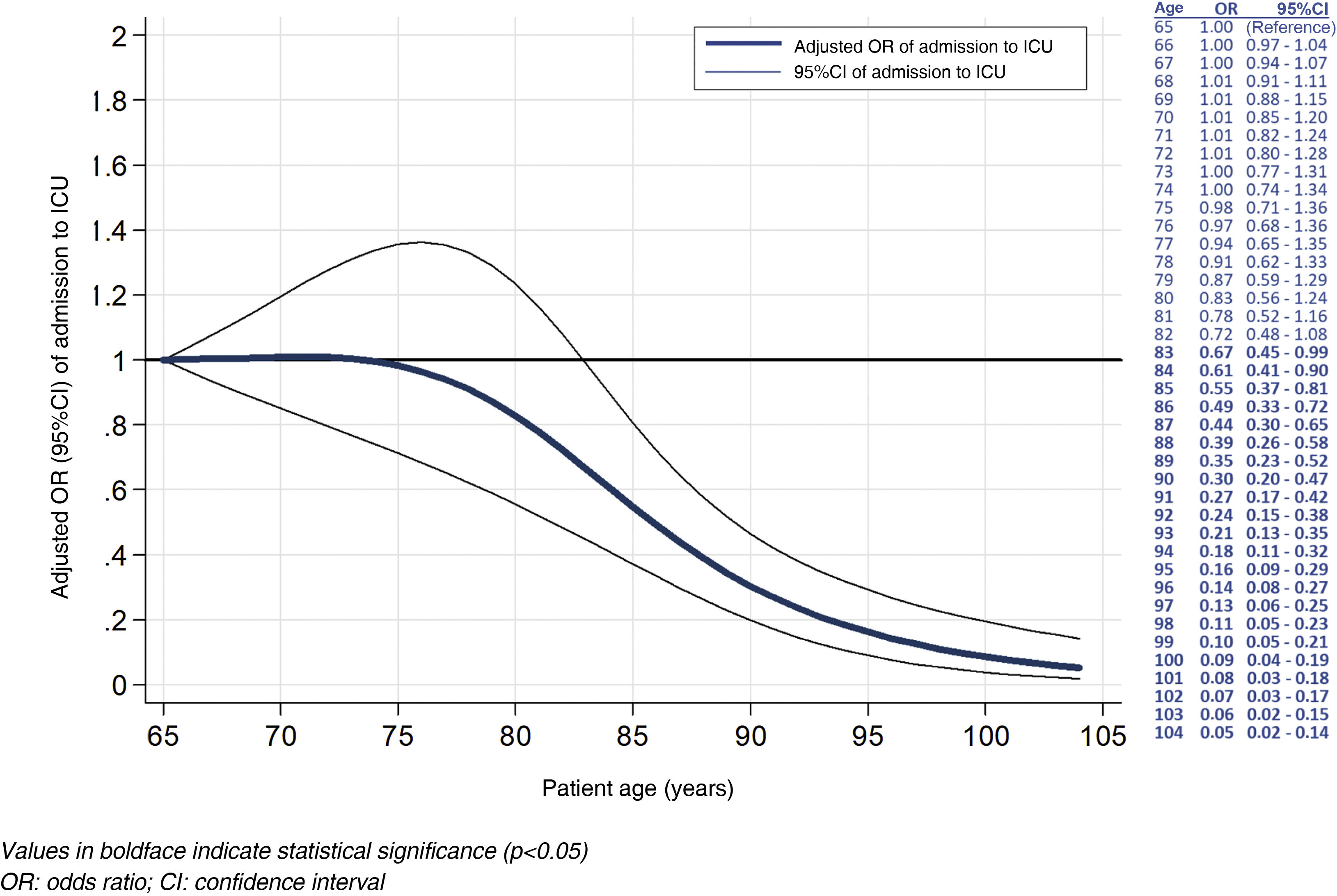
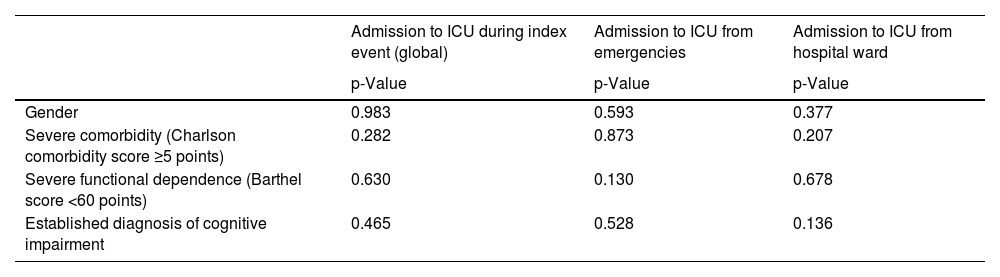
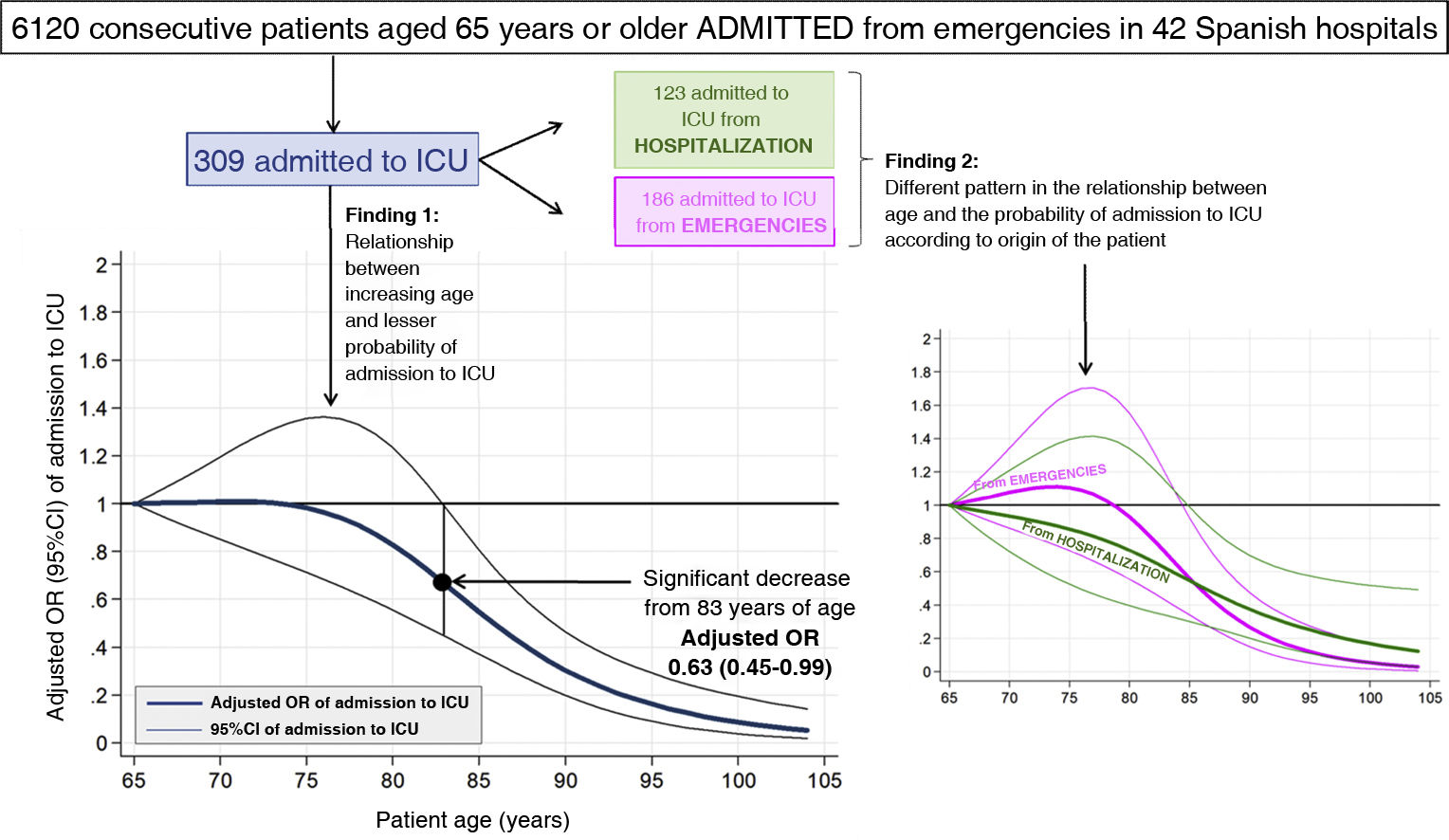
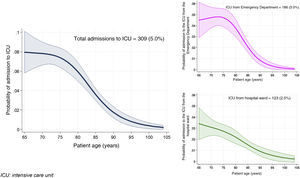
The probability of admission to the ICU was about 8% among those between 65–75 years of age, and subsequently decreased constantly until reaching close to 0% from the age of 95 years (Fig. 1). On analyzing the OR of admission to the ICU adjusted for gender, comorbidity, dependence and cognitive impairment, a similar curve was obtained, with ORs that remained practically constant between 65–75 years of age, followed by a progressive decrease that reached statistical significance from the age of 83 years (OR: 0.67; 95%CI: 0.45–0.49) onwards. In the case of patients aged 95 years, this OR was 0.16 (95%CI: 0.09–0.29) (Fig. 2). This dose-response curve of the relationship between age and admission to the ICU was not significantly modified by patient gender, comorbidity, dependence or cognitive impairment (interaction p>0.05 in all cases) (Table 3).
Analysis of interaction in the adjusted model of the association between patient age and admission to the intensive care unit for the variables gender, comorbidity, functional dependence and cognitive impairment.
| Admission to ICU during index event (global) | Admission to ICU from emergencies | Admission to ICU from hospital ward | |
|---|---|---|---|
| p-Value | p-Value | p-Value | |
| Gender | 0.983 | 0.593 | 0.377 |
| Severe comorbidity (Charlson comorbidity score ≥5 points) | 0.282 | 0.873 | 0.207 |
| Severe functional dependence (Barthel score <60 points) | 0.630 | 0.130 | 0.678 |
| Established diagnosis of cognitive impairment | 0.465 | 0.528 | 0.136 |
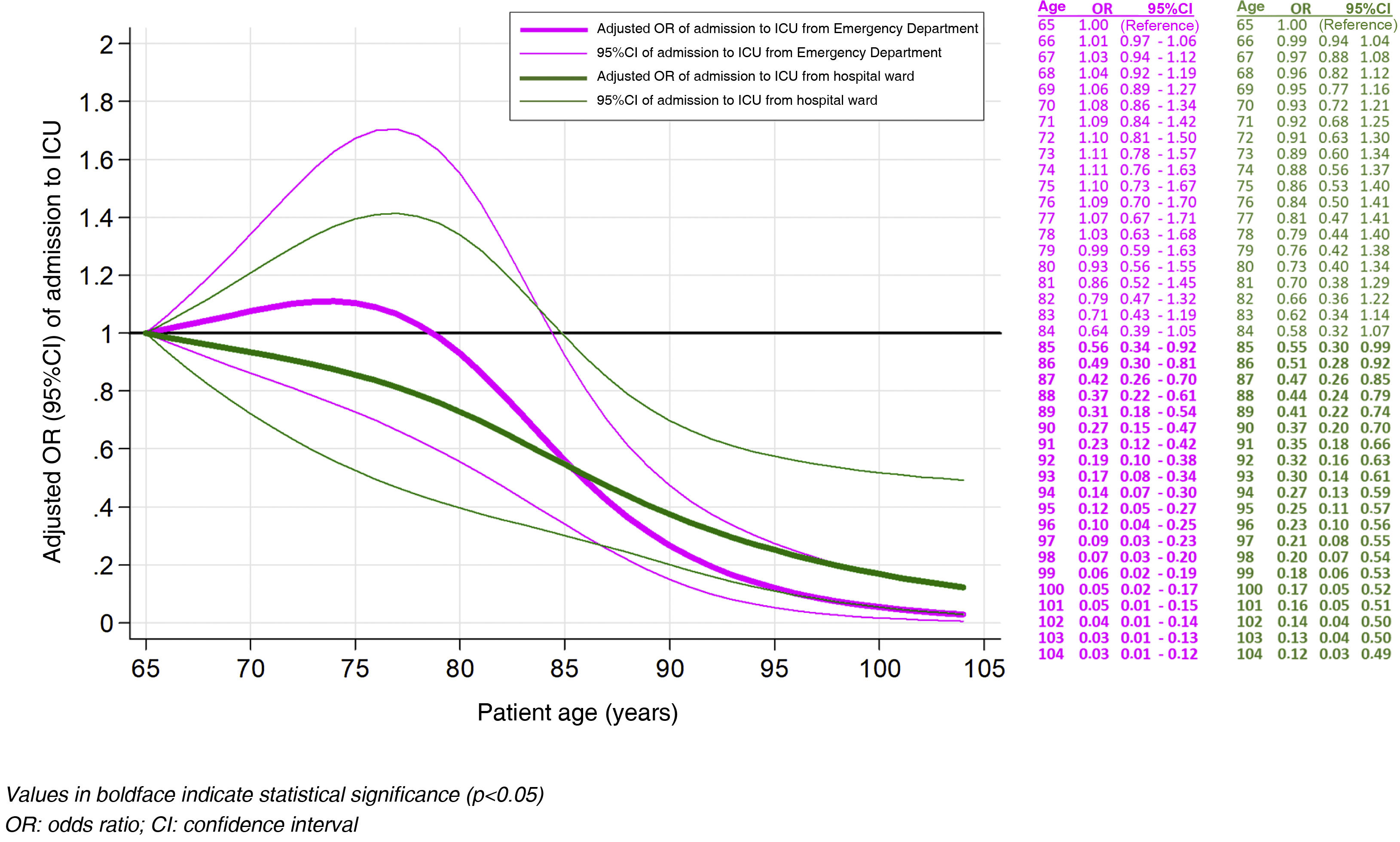
The probability of admission to the ICU from the ED was between 4% and 5% in the 65–75 years of age range, followed by a sharp and progressive decrease to close to 0% from the age of 95 years onwards. Similarly, the adjusted ORs of admission to the ICU from the ED were not <1 until the age of 79 years, and proved statistically significant from the age of 85 years (OR: 0.56, 95%CI: 0.34–0.92). In the case of patients aged 95 years, the OR was 0.16 (95%CI: 0.09–0.29). In contrast, the probability of admission to the ICU from the hospital ward was about 3.5% at 65 years of age, and subsequently decreased slowly and progressively in a quite linear manner until reaching close to 0% towards the age of 100 years (Fig. 1). The adjusted ORs likewise decreased slowly and progressively from the age of 65 years; where always <1 beyond that age; and proved statistically significant from the age of 85 years (OR: 0.55, 95%CI: 0.30–0.99) onwards. In the case of patients aged 95 years, the OR was 0.25 (95%CI: 0.11–0.57) (Fig. 3). Patient gender, comorbidity, dependence and cognitive impairment did not modify the association between age and admission to the UCI from the ED or the hospital ward (Table 3).
DiscussionThe present study offers three novel conclusions that should be highlighted. Firstly, it shows that the probability of admission to the ICU decreases significantly from the age of 83 years onwards. Secondly, this decrease in relation to age persists even after taking into account other factors that intervene in the decision of whether to admit a patient to the ICU or not, such as comorbidity, functional dependence and cognitive impairment. Lastly, the individualized analysis of admissions to the ICU from the ED or from hospital wards revealed a correlation to patient age that could differ in these two circumstances: the probability of admission from the ED remains unaltered until more advanced patient ages than when admission is from the hospital ward, and then decreases faster and more intensely, reaching lesser probabilities of admission in the more elderly patients that are admitted from the ED.
Overall, age is a limiting factor for admission to the ICU in that it is the main parameter limiting the chances of survival among individuals with acute or chronic disease. However, the decision not to admit a patient to the ICU may affect relatively young individuals if added survival-limiting factors are present. In this sense, the ADENI-UCI study, carried out over a consecutive 13-month period (2018–2019) in 62 Spanish Departments of Intensive Care Medicine, reviewed 2284 decisions against admission to the ICU. The mean age of the patients in which admission to the ICU was discarded was 75 years. However, age was precisely the factor less often linked to the decision against admission (only 31% of the cases), and in those cases where age was the cited reason for non-admission, the mean age of the affected patients was 88 years.14 Although chronological age in itself is not the only element taken into account by intensivists in deciding against admission to the ICU in Spain, there are clear data indicating that elderly critical patients are less often admitted to the ICU.18 The ethical debate on this issue has intensified in recent months due to the COVID-19 pandemic and the application of age as an ICU admission criterion in the peak moments of the first wave.19,20 However, it should be underscored that triage decisions, with prioritization in the face of limited resources, is completely different in ethical and care terms from the limitation of life support decisions that can include patient admission to the ICU as a therapeutic ceiling. We believe that the present study, carried out in the year before the COVID-19 outbreak, offers objective data in Spain on routine clinical practice in a non-selected elderly population, and shows that at the time of the study the age of 75 years begins to indicate a decrease in the chances of admission to the ICU, and that from the age of 83 years onwards this decrease becomes statistically significant.
Beyond the age factor, assessment of the social circumstances and of the basal situation of the patient is increasingly carried out among patients seen in hospital EDs, as these are risk factors for a poor patient outcome.21 In this respect, their correct evaluation allows us to establish a prognosis more coherent with the real-life situation,22 being moreover needed to assess the intensity of the treatment required.14,23–25 In the abovementioned ADENI-UCI study, comorbidity, prior functional limitation, poor expectable quality of life, and futility were the most frequent reasons for non-admission to the ICU, being present in between 51%–62% of the cases.14 Thus, although these factors were related to the probability of admission to the ICU in the present study, it is notorious that their presence did not exert a differential effect in terms of the decrease in chances for admission to the ICU seen for advancing patient age, since no interaction was observed between them and the association between age and admission to the ICU.
An interesting aspect of this study is that the analysis of the results suggests a different behavior of age as a determinant of admission to the ICU depending on whether the patient comes from the ED or from the hospital ward. In this sense, and possibly related to suboptimal assessment by the ED physician (who is not the usual physician of the patient), with partial unawareness of the personal, social, functional and chronicity circumstances of the patient, and the need for rapid decision making, the present study identified a more conservative attitude in the assessment made in the ED (i.e., more inclined towards admission) when the patients are in a younger age range (65–75 years). In contrast, this trend was inverted in older individuals (i.e., showing a lesser tendency to admit patients over 85 years of age). It must be acknowledged that combined assessment of the situations that limit therapeutic intensity is easier to make during hospitalization; probably as a result of this, the decrease in the probability of patient admission to the ICU decreased more gradually and constantly and linearly in the case of patients coming from the hospital ward. Furthermore, the preferences of the patients and relatives are easier to take into account, influencing decision-making in the case of hospitalized patients versus patients coming from emergency care. The ADENI-UCI study found the mortality rate among patients in the ED in whom admission to the ICU was discarded to be lower than in hospitalized patients against whom admission was decided against.14 This would speak in favor of the existence of different conditioning factors in deciding ICU admission between patients in the ED and patients who have already been admitted to the hospital.
LimitationsThe present study has several limitations. First, the 42 EDs that contributed patients to the EDEN registry were not randomly selected but showed their willingness to participate. Nevertheless, the broad territorial representation (12 out of the 17 Autonomous Communities in Spain were included) and their profiles (university hospitals, high-technology centers and district hospitals) probably imply that this bias is small. Second, the analysis was not made by disease groups but on a global basis. This may imply that the findings obtained are conditioned by certain specific processes that have not been analyzed. Nevertheless, we believe that the global view of the needs of the elderly population during care in the ED is better represented in this way, as we included all patients seen in the ED, independently of the reason for consultation. Furthermore, the severity of the acute condition does not usually imply a limitation to admission to the ICU in itself, and it would have little impact on the results. Third, this is a secondary analysis of a multipurpose cohort; the associations found therefore may be influenced by factors not contemplated in the design of the cohort. In this regard, the model of the relationship between age and admission to the ICU was only adjusted to four variables (gender, comorbidity, functional condition and cognitive status), and other factors not analyzed might have modified the observed relationship in part. Thus, the findings must be seen as generators of hypotheses to be specifically confirmed by further studies. In this sense, other very important variables, such as the APACHE or SAPS scores, or frailty measures,26,27 could have allowed for a more in-depth and complete analysis. However, review of the patient histories was limited to the stay in the ED, and these data were not collected. Fourth, the existence of living will documents of the patients was not recorded; although these documents are still infrequent in Spain, they could have influenced the decision of admission in concrete cases. Fifth, patient inclusion was limited to a short period of the year (the first week of April) when still under the influence of the usual flu and viral pandemics of winter and spring. However, this circumstance should not have influenced the assessment of patients requiring admission to the ICU.
ConclusionsThe present study evidences that the probability of admission to the ICU among patients requiring urgent hospitalization decreases significantly from the age of 83 years onwards. Although admission to the ICU is also initially influenced by patient gender, comorbidity, functional dependence and cognitive impairment, these factors do not affect the relationship between age and the chances for admission to the ICU. The analysis made allows us to postulate the existence of a difference in behavior of the mentioned relationship between age and admission to the ICU depending on whether the patient comes from the ED or the hospital ward.
Author’s contributionGuillermo Burillo-Putze, Patricia Parra-Esquivel, Sira Aguiló, Sònia Jiménez, Javier Jacob, Pascual Piñera Salmerón, Pere Llorens, Eric Jorge García-Lamberechts, Francisco Javier Montero Pérez, Adriana Gil- Rodrigo, Cesáreo Fernández, Aitor Alquezar-Arbé, Juan González del Castillo and Òscar Miró participated in the study design, case report form validation, case registry, analysis of results, and writing of the manuscript.
Esperanza Muñoz-Triano, Manuel Salido Mota, Rodrigo Javier Gil Hernández, Jorge Pedraza García, Angela Cobos Requena, Esther Gargallo Garcia, Monica de Diego Arnaiz, Marta Iglesias Vela, Rafael Antonio Pérez-Costa, Sara del Mar Pérez Peñalva, Beatriz Valle Borrego, Eva Quero Motto, Belén Morales Franco and Maria Adroher Muñoz are investigators of the EDEN challenge, and have been the principal investigators at their respective centers, performing data collection, analysis of results and writing of the manuscript.
Conflicts of interestThe authors declare that they have no conflicts of interest with respect to this study.
Hospital Clínico San Carlos, Madrid: Juan González del Castillo, Cesáreo Fernández Alonso, Jorge García Lamberechts, Paula Queizán García, Andrea B Bravo Periago, Blanca Andrea Gallardo Sánchez, Alejandro Melcon Villalibre, Sara Vargas Lobé, Laura Fernández García, Beatriz Escudero Blázquez, Estrella Serrano Molina, Julia Barrado Cuchillo, Leire Paramas López, Ana Chacón García. Hospital Universitario Infanta Cristina, Parla: Ángel Iván Diaz Salado, Beatriz Honrado Galán, Sandra Moreno Ruíz. Hospital Santa Tecla, Tarragona: Enrique Martín Mojarro, Lidia Cuevas Jiménez. Hospital Universitario de Canarias, Tenerife: Guillermo Burillo Putze, Aarati Vaswani- Bulchand, Patricia Eiroa-Hernández. Hospital Norte Tenerife: Patricia Parra-Esquivel, Montserrat Rodríguez-Cabrera. Hospital General Universitario Reina Sofía, Murcia: Pascual Piñera Salmerón, José Andrés Sánchez Nicolás, Yurena Reverte Pagán, Lorena Bernabé Vera, Juan José López Pérez. Hospital Universitario del Henares, Madrid: Martín Ruiz Grinspan, Cristóbal Rodríguez Leal, Rocío Martínez Avilés, María Luisa Pérez Díaz-Guerra. Hospital Clínic, Barcelona: Òscar Mir, Sònia Jiménez, Sira Aguiló Mir, Francesc Xavier Alemany González, María Florencia Poblete Palacios, Claudia Lorena Amarilla Molinas, Ivet Gina Osorio Quispe, Sandra Cuerpo Cardeñosa. Hospital Universitario y Politécnico La Fe, Valencia: Leticia Serrano Lázaro, Javier Millán Soria, Jésica Mansilla Collado, María Bóveda García. Hospital Universitario Dr. Balmis, Alicante: Pere Llorens Soriano, Adriana Gil Rodrigo, Begoña Espinosa Fernández, Mónica Veguillas Benito, Sergio Guzmán Martínez, Gema Jara Torres, María Caballero Martínez. Hospital Universitario de Bellvitge, L'Hospitalet de Llobregat, Barcelona: Javier Jacob Rodríguez, Ferran Llopis, Elena Fuentes, Lidia Fuentes, Francisco Chamorro, Lara Guillen, Nieves López. Hospital de Axiarquia, Málaga: Coral Suero Méndez, Lucía Zambrano Serrano, Rocío Lorenzo Álvarez. Hospital Regional Universitario de Málaga: Manuel Salido Mota, Valle Toro Gallardo, Antonio Real López, Lucía Ocaña Martínez, Esther Muñoz Soler, Mario Lozano Sánchez. Hospital Santa Barbara, Soria: Fahd Beddar Chaib, Rodrigo Javier Gil Hernández Hospital Valle de los Pedroches, Pozoblanco, Córdoba: Jorge Pedraza García, Paula Pedraza Ramírez. Hospital Universitario Reina Sofía. Córdoba: F. Javier Montero-Pérez, Carmen Lucena Aguilera, F. de Borja Quero Espinosa, Ángela Cobos Requena, Esperanza Muñoz Triano, Inmaculada Bajo Fernández, María Calderón Caro, Sierra Bretones Baena. Hospital Universitario Gregorio Marañón, Madrid: Esther Gargallo Garc, Leonor Andrés Berián, María Esther Martínez Larrull, Susana Gordo Remartínez, Ana Isabel Castuera Gil, Laura Martín González, Melisa San Julián Romero, Montserrat Jiménez Lucena, María Dolores Pulfer. Hospital Universitario de Burgos: Pilar López Diez, Mónica de Diego Arnaiz, Verónica Castro Jiménez, Lucía González Ferreira, Rocío Hernando González, María Eugenia Rodríguez Palma. Complejo Asistencial Universitario de León: Marta Iglesias Vela, Rudiger Carlos Chávez Flores, Alberto Álvarez Madrigal, Albert Carbó Jordá, Enrique González Revuelta, Héctor Lago Gancedo, Miguel Moreno Martín, M. Isabel Fernández González. Hospital Universitario Morales Meseguer, Murcia: Rafael Antonio Pérez-Costa, María Rodríguez Romero, Esperanza Marín Arranz, Sara Barnes Parra. Hospital Francesc de Borja de Gandía, Valencia: María José Fortuny Bayarri, Elena Quesada Rodríguez, Lorena Hernández Taboas, Alicia Sara Knabe. Hospital Universitario Severo Ochoa, Leganés. Madrid: Beatriz Valle Borrego, Julia Martínez-Ibarreta Zorita, Irene Cabrera Rodrigo, Beatriz Mañero Criado, Raquel Torres Gárate, Rebeca González González. Hospital Clínico Universitario Virgen Arrixaca, Murcia: Eva Quero Motto, Nuria Tomas García, Lilia Amer Al Arud, Miguel Parra Morata. Hospital Universitario Lorenzo Guirao, Cieza, Murcia: Carmen Escudero Sánchez, Belén Morales Franco, José Joaquín Giménez Belló. Hospital Universitario Dr. Josep Trueta, Girona: María Adroher Muñoz, Ester Soy Ferrer, Eduard Anton Poch Ferrer. Hospital de Mendaro, Guipuzkoa: Jeong-Uh Hong Cho. Hospital Universitario Miguel Servet, Zaragoza: Rafael Marrón, Cristina Martín Durán, Fernando López López, Alberto Guillen Bove, Violeta González Guillén, María Diamanti, Beatriz Casado Ramón, Ana Herrer Castejón. Hospital Comarcal El Escorial, Madrid: Sara Gayoso Martín. Hospital Do Salnes, Villagarcia de Arosa, Pontevedra: María Goretti Sánchez Sindín. Hospital de Barbanza, Ribeira, A Coruña: Azucena Prieto Zapico, María Esther Fernández Álvarez. Hospital del Mar, Barcelona: Isabel Cirera, Bárbara Gómez y Gómez, Carmen Petrus Rivas. Hospital Santa Creu y Sant Pau, Barcelona: Aitor Alquezar Arbé, Miguel Rizzi, Marta Blázquez Andion, Carlos Romero Carret, Sergio Pérez Baena, Laura Lozano Polo, Roser Arenos Sambro, José María Guardiola Tey, Carme Beltrán Vilagrasa. Hospital de Vic, Barcelona: Lluís Llauger. Hospital Valle del Nalón, Langreo, Asturias: Ana Murcia Olagüenaga, Celia Rodríguez Valles, Verónica Vázquez Rey. Hospital Altagracia, Manzanares, Cuidad Real: Elena Carrasco Fernández, Sara Calle Fernández. Hospital Nuestra Señora del Prado de Talavera de la Reina, Toledo: Ricardo Juárez González, Mar Sousa, Laura Molina, Mónica Cañete. Hospital Universitario Vinalopó, Elche, Alicante: Esther Ruescas, María Martínez Juan, Pedro Ruiz Asensio, María José Blanco Hoffman. Hospital de Móstoles, Madrid: Fátima Fernández Salgado, Eva de las Nieves Rodríguez, Gema Gómez García, Beatriz Paderne Díaz.