The SEMICYUC Nutrition and Metabolism Working Group has conducted a national survey with two goals in mind: identify the methods that are used to assess the nutritional status in Spanish intensive care units (ICU) and objectify the incidence of refeeding syndrome.
The assessment of nutritional status could be considered the first step of nutritional therapy. Its main goal is to identify malnourished patients or those at risk of developing malnutrition at their ICU admission and who might benefit from nutritional therapy.1 A correct nutritional assessment requires a complete clinical history to help find the patients at risk: 7–10-day-fasting associated with severe stress, nervous anorexia, chronic alcoholism, postoperative patients of abdominal surgery, marasmus or kwashiorkor type of malnutrition, especially with weight losses>10% in 2 months, prolonged IV fluid therapy, nervous anorexia or oncological patients.2
At the moment, there is no consensus on what the most appropriate method is for the identification of nutritional risk in critically ill patients, although, by definition, critically ill patients are at nutritional risk due to their increased energetic/protein needs in the acute disease and because many cases are consistent with data of previous malnutrition. Recently, a new method has been developed for the assessment of nutritional risk in critically ill patients: the NUTRIC-Score.3 Although it still needs validation as a maker of nutritional risk, it has proved to be a fine prognostic marker, since scores≥5 (when interleukin 6 is not available) are associated with higher mortality rates at 28 days and longer periods of time on mechanical ventilation.
The refeeding syndrome is an underdiagnosed condition in most ICUs. It may be defined as hydroelectrolytic alterations accompanied by retention of sodium and fluids as a result of intensive nutritional support in patients severely malnourished or deprived of food.4,5,6 Refeeding gives rise to hydric overload, introduction of elements such as phosphorus, magnesium, or potassium in the intracellular space and its decline in plasma levels, and to an increased need for vitamins (deficit of thiamine),2,7 which may lead to heart failure, arrhythmias, hyperosmolar coma, epileptic seizures, lactic acidosis, rhabdomyolysis, renal failure, hemolytic anemia, thrombocytopenia and even death.
In critically ill patients, it is essential to detect those at nutritional risk at their ICU admission, and those at risk of developing refeeding syndrome.
The form was designed and distributed and the answers were collected using Google Drive form tool (© 2017 Google) and then distributed to the hospitals included in an already created database8 and through the SEMICYUC distribution list (sent to 3499 Spanish and Latin American members). Answers from 118 hospitals and 157 intensivists were received from the different units of each hospital (some hospitals are divided into several units). Only one answer per unit was considered. The answer sent was based on the experience of the personnel that filled out the survey.
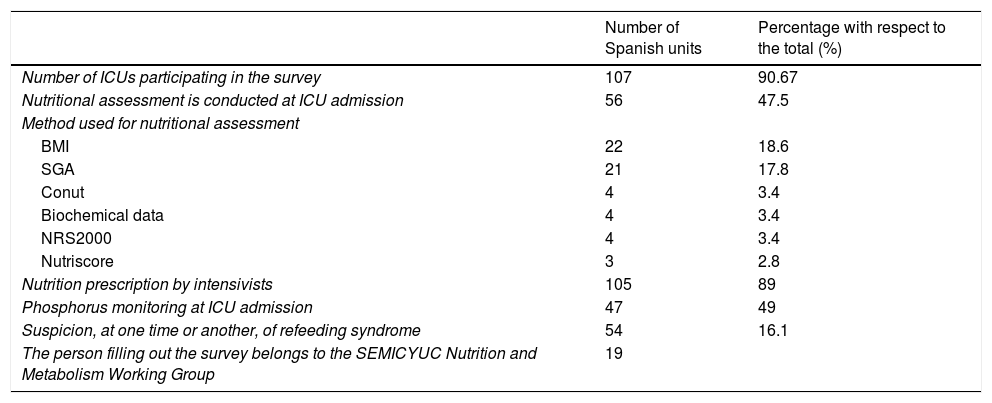
The results from the survey are shown in Table 1; 118 hospitals [107 Spanish (90.7% of the total) and 11 Latin American (9.3%)]. The results from the table include only the results of the participating Spanish hospitals; 107 Spanish hospitals grouped into 38 provinces, with the highest participation rate in Barcelona (14 hospitals) followed by Madrid (11 hospitals), Valencia (8 hospitals), Alicante and Zaragoza (5 hospitals), respectively. The average number of beds from the hospitals that answered the survey is 17.91±12.77 beds per hospital.
Results from the survey on nutritional assessment conducted from the SEMICYUC Nutrition and Metabolism Working Group among Spanish intensive care units.
| Number of Spanish units | Percentage with respect to the total (%) | |
|---|---|---|
| Number of ICUs participating in the survey | 107 | 90.67 |
| Nutritional assessment is conducted at ICU admission | 56 | 47.5 |
| Method used for nutritional assessment | ||
| BMI | 22 | 18.6 |
| SGA | 21 | 17.8 |
| Conut | 4 | 3.4 |
| Biochemical data | 4 | 3.4 |
| NRS2000 | 4 | 3.4 |
| Nutriscore | 3 | 2.8 |
| Nutrition prescription by intensivists | 105 | 89 |
| Phosphorus monitoring at ICU admission | 47 | 49 |
| Suspicion, at one time or another, of refeeding syndrome | 54 | 16.1 |
| The person filling out the survey belongs to the SEMICYUC Nutrition and Metabolism Working Group | 19 | |
BMI, body mass index; NRS2000, nutritional risk screening; SEMICYUC, Spanish Society of Intensive and Critical Care Medicine and Coronary Units; ICU, intensive care unit; SGA, subjective global assessment.
When it comes to the method used by every unit to conduct nutritional assessments, based on our survey, the most commonly used methods were the body mass index and the subjective global assessment followed by Conut, biochemical data, NRS 2000 and finally the NUTRIC Score. In 81.6% of the units (96 units), the phosphorus levels at ICU admission were monitored. In 47 of these 96 units (49%), all patients were monitored at ICU admission, in 27 units (28.1%) the phosphorus levels were measured only in those patients who were going to go on artificial nutrition. In 22 units (22.9%), these levels were only measured in patients with diseases suspicious of hyper/hypophosphatemia. At one time or another, in 54 units there was suspicion of refeeding syndrome in the last 5 years and eventually refeeding syndrome was diagnosed once in 10 units (18.5%), twice in 9 units (16.7%), 3 times in 3 units (5.65%), 4 times in 1 unit (1.9%), 5 times in 2 units (3.7%), 10 times in 1 unit (1.9%) and 25 times in 1 unit (1.9%).
The results from this survey tell us that in most units, it is the intensivists who prescribe nutrition. In less than half the ICUs, the nutritional status is assessed, and the phosphorus levels are measured at admission. The methods most commonly used for nutritional assessment are the body mass index and the subjective global assessment (no specific method in critically ill patients) and in less than half the ICUs the refeeding syndrome has been suspected at one time or another.
From the SEMICYUC Nutrition and Metabolism Working Group, we wish to emphasize the importance of protocolizing nutritional assessment during the patients’ admission at the ICU. Also, it is essential to find those patients at risk of developing refeeding syndrome which, as we have been able to see in the results coming from the survey, is still an underdiagnosed syndrome. This will allow us to establish adequate measures to prevent its development (hydroelectrolytic and vitamin repositioning prior to nutritional support that will be initiated more slowly).9
We wish to thank the SEMICYUC Nutrition and Metabolism Working Group for their decisive collaboration conducing the survey and elaborating this manuscript.
Please cite this article as: Zamora Elson M, Trujillano Cabello J, González Iglesias C, Bordejé Laguna ML, Fernández Ortega JF, Vaquerizo Alonso C. Encuesta sobre valoración del estado nutricional y síndrome de realimentación en las unidades de cuidados intensivos en España. Med Intens. 2018;42:511–512.