Little is known about the evolution and long-term neurological status of pediatric patients who survive out-of-hospital cardiac arrest. Our aim is to describe long-term survival and neurological status.
DesignRetrospective observational study, based on the Andalusian Register of out-of-hospital Cardiac Arrest.
SettingPre-hospital Care.
PatientsThe study included patients aged 0–15 years between January 2008 and December 2012.
InterventionsPatients follow up.
VariablesPrehospital and hospital care variables were analyzed and one-year follow-up was performed, along with a specific follow-up of survivors in June 2014.
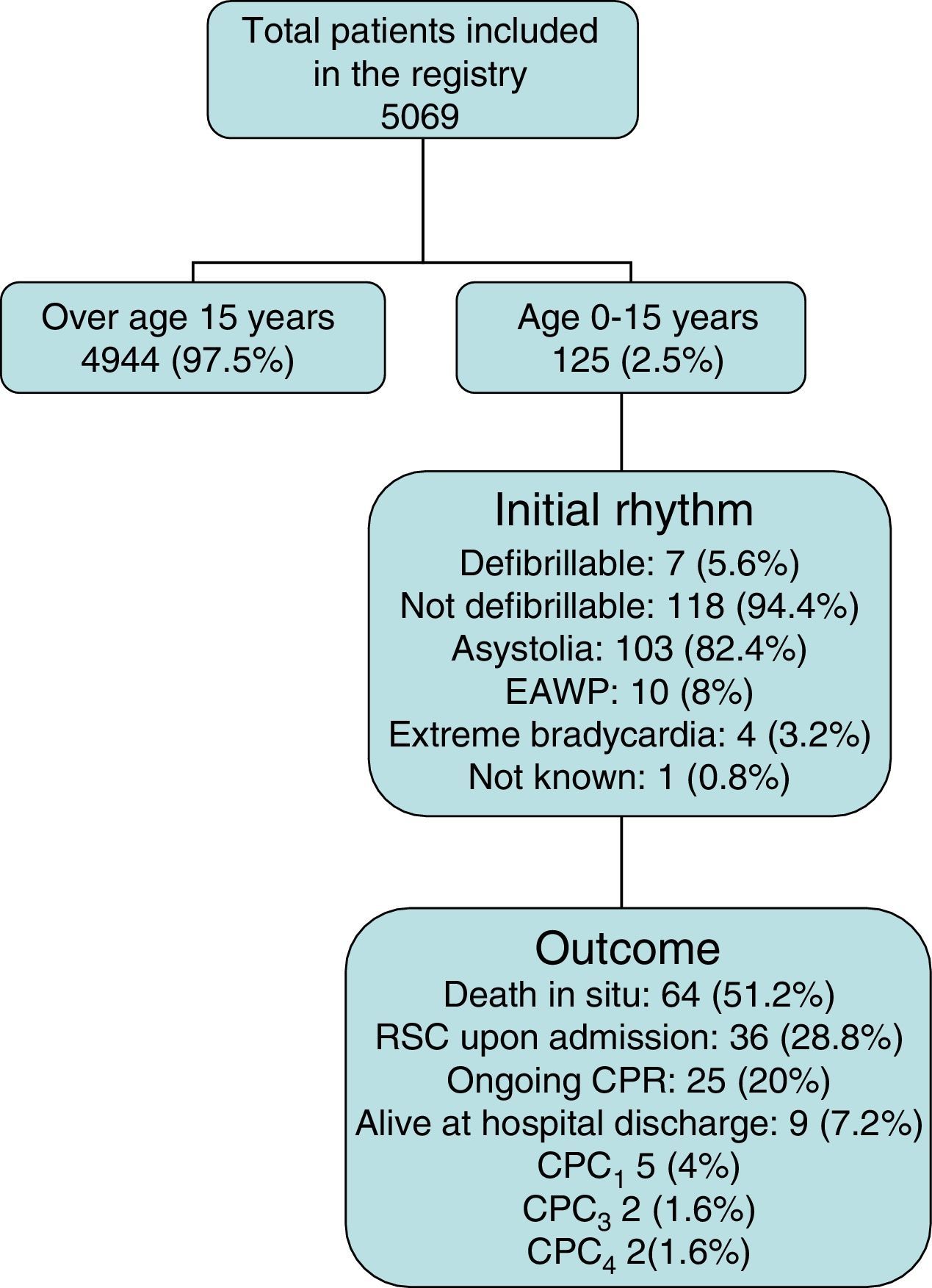
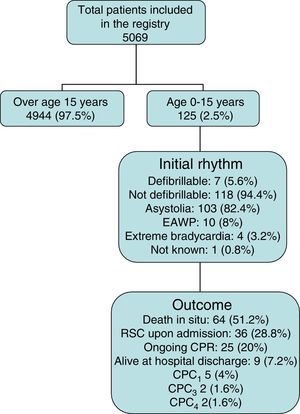
ResultsOf 5069 patients included in the register, 125 (2.5%) were aged ≤15 years. Cardiac arrest was witnessed in 52.8% of cases and resuscitation was performed in 65.6%. The initial rhythm was shockable in 7 (5.2%) cases. Nearly half (48.8%) the patients reached the hospital alive, of whom 20% did so while receiving resuscitation maneuvers. Only 9 (7.2%) patients survived to hospital discharge; 5 showed ad integrum recovery and 4 showed significant neurological impairment. The 5 patients with complete recovery continued their long-term situation. The remaining 4 patients, although slight improvement, were maintained in situation of neurological disability.
ConclusionsSurvival after out-of-hospital cardiac arrest in pediatric patients was low. The long-term prognosis of survivors with good neurological recovery remains, although improvement in the rest was minimal.
No existe demasiada información sobre la evolución y estado neurológico a largo plazo de los pacientes en edad pediátrica que sobreviven a una parada cardiaca extrahospitalaria. Nuestro objetivo es describir la supervivencia y estado neurológico de estos pacientes a largo plazo.
DiseñoEstudio observacional retrospectivo. Basado en el Registro Andaluz de Parada Cardiaca Extrahospitalaria.
ÁmbitoAtención Prehospitalaria.
PacientesEntre 0 y 15 años atendidos entre enero de 2008 y diciembre de 2012 por Parada Cardiaca Extrahospitalaria.
IntervencionesSeguimiento de pacientes.
VariablesSe incluyen variables de la atención prehospitalaria, hospitalaria y del seguimiento al año y un seguimiento específico de los supervivientes en junio de 2014.
ResultadosSe incluyeron en el registro un total de 5069 pacientes de los que 125(2.5%) tenían 15 o menos años. La parada fue presenciada en el 52.8% de los casos y hubo reanimación previa en 65.6%. El ritmo inicial fue desfibrilable en 7 (5.2%) casos. Un 48.8% de los pacientes llegó al hospital aunque un 20% lo hizo en situación de reanimación en curso. De los 9 (7.2%) pacientes que sobrevivieron al alta hospitalaria, 5 de ellos lo hicieron con recuperación ad integrum y 4 con grave deterioro neurológico. Los 5 pacientes con recuperación completa mantuvieron su situación a largo plazo. Los 4 pacientes restantes, aunque con discreta mejoría, se mantuvieron en situación de discapacidad neurológica.
ConclusionesLa supervivencia de la parada cardiaca extrahospitalaria en edad pediátrica es baja. El pronóstico a largo plazo de los pacientes con buena recuperación neurológica desde el inicio se mantiene, aunque la mejoría en el resto es mínima.
While once considered a rare event,1 out-of-hospital cardiac arrest (CA) in the pediatric population currently holds a relevant place in this type of disease.2,3 Nevertheless, in comparison with CA in the adult population, the available information referred to pediatric patients is scarce. Some series have presented a significant number of patients, analyzing the incidence of the disease at population level and the outcomes referred to survival and neurological status at hospital discharge.4 However, there is controversy regarding the long-term outcomes in terms of pediatric patient recovery. This situation is due to the few data available on neurological recovery in periods late after discharge from hospital. The most important series do not explore beyond neurological status one month after the event.5,6 On the other hand, pediatric age has not been clearly defined in the literature on CA, and in this regard the incidence and final outcomes vary greatly according to the different age intervals considered. The age range involved therefore needs to be specified.5,7
The present study describes the long-term outcomes in terms of survival and neurological status in patients between 0 and 15 years who suffer out-of-hospital CA.
Patients and methodsA retrospective observational study was made between January 2008 and December 2012, based on data obtained from the Andalusian Out-of-Hospital Cardiac Arrest Registry (Registro Andaluz de Parada Cardíaca Extrahospitalaria), the protocols of which have been described elsewhere.8 In brief, this is a continuous registry of cases of out-of-hospital CA assisted by the emergency care teams (ECTs) of the Public Company of Healthcare Emergencies of Andalusia (Spain)(Empresa Pública de Emergencias Sanitarias de Andalucía, EPES).
SettingAs a public service, the EPES manages out-of-hospital healthcare emergencies throughout Andalusia. However, due to its socio-geographic structure, the resources and care dedicated to out-of-hospital emergencies by the EPES result in overland coverage of 67% of the population, and mixed air and overland coverage of 100%.9,10
Patients studiedWhen dealing with ventricular fibrillation or when performing resuscitation maneuvers, the ECTs use codes 427.41 (ventricular fibrillation) and 427.5 (CA) to typify the care provided. All cases with these codes are automatically entered in the registry. The pre-hospital care parameters are documented in each case: patient information (gender, age), the context of CA (place where CA occurs, whether the event was witnessed or not, prior life support measures with or without defibrillation, time intervals from event to call/arrival of the ECT), ECT interventions (airway maintenance, defibrillation, drugs, condition at end of resuscitation, estimated cause of arrest), hospital evolutive parameters (coronary intervention, hypothermia, survival and neurological status at discharge), and follow-up data at discharge (survival and neurological status at discharge). The hospital data were consulted from the single (unified) patient case history. Follow-up after discharge, at one month and one year, is made by means of a standardized telephone survey, centralized for all Andalusia, and carried out from an EPES coordination center. Consent is requested from the patient (or relatives – in this case always the parents) for both the interview and for statistical use of the data. Evaluation of neurological status was based on the pediatric Cerebral Performance Category (CPC) scale.11 In order to limit the loss of information and loss of number of cases, an annual request is made for access to the National Mortality Statistics Institute of the Spanish Ministry of Health. Lastly, for the present analysis, special follow-up was conducted during the month of May 2014. This follow-up determined the maximum evolution time of each patient. The definition of the selected variables (Table 1) follows the Utstein recommendations.12
General characteristics of the 125 pediatric patients.
| Variables | Distribution |
|---|---|
| Age in years (mean±SD) | 5.3±5 |
| Median (IQR) in years | 4 (1–9.5) |
| Males, n (%) | 77 (61.6) |
| Place of arrest, n (%) | |
| Home | 36 (29.2) |
| Public place | 31 (24.8) |
| Street | 23 (18.4) |
| Non-hospital medical center | 23 (18.4) |
| Others | 10 (8) |
| Ambulance of the ECT | 2 (1.6) |
| Witnessed arrest, n (%) | 66 (52.8) |
| Witnesses | 38 (30.4) |
| Other healthcare personnel | 16 (12.8) |
| ECT | 12 (9.6) |
| Life support measures before arrival of the ECT | 82 (65.6) |
| Healthcare personnel | 64 (51.2) |
| Witnesses | 14 (11.2) |
| Non-healthcare public service personnel | 2 (1.6) |
| Witnesses with telephone CPR support | 2 (1.6) |
| Defibrillations before arrival of the ECT | 1 |
| Cause of CA, n (%) | |
| Traumatic | 23 (18.4) |
| Respiratory | 22 (17.6) |
| Not known | 37 (29.6) |
| Cardiac | 20 (16) |
| Others | 13 (10.4) |
| Drowning | 5 (4) |
| Toxic-metabolic | 4 (3.2) |
| Neurological | 1 (0.8) |
| Interval collapse-arrival ECT, median (IQR) in minutes | 14 (9–24) |
| Interval call-arrival ECT, median (IQR) in minutes | 8 (12–18) |
SD: standard deviation; ECT: emergency care team; CA: cardiac arrest; CPR: cardiopulmonary resuscitation; IQR: interquartile range.
The present study considered the pediatric patients included in the registry and aged between 0 and 15 years (both included). Futile resuscitation cases were excluded to the effects of analysis.
Statistical analysisA descriptive analysis was made of the general characteristics, the pre-hospital care provided, and the characteristics of the survivors. The results are expressed as the mean±standard deviation, median and interquartile range, or as the number and percentage, as applicable.
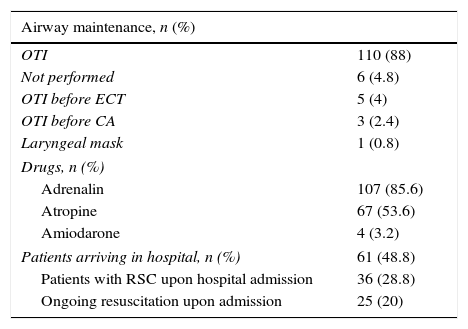
ResultsThe registry comprised a total of 5069 patients subjected to advanced life support care. Of these individuals, 125 (2.5%) were 15 years old or younger (Fig. 1). A total of 113 CA events (90.4%) occurred before arrival of the ECT. The exact timing of the event could not be established in 50 cases (44.2%), i.e., the interval could only be calculated in 63 (55.8%). The general characteristics of the patients are reported in Table 1. The details referred to pre-hospital care and the outcomes following such care are described in Table 2. None of the patients admitted to hospital received treatment involving hypothermia.
Pre-hospital treatment measures.
| Airway maintenance, n (%) | |
|---|---|
| OTI | 110 (88) |
| Not performed | 6 (4.8) |
| OTI before ECT | 5 (4) |
| OTI before CA | 3 (2.4) |
| Laryngeal mask | 1 (0.8) |
| Drugs, n (%) | |
| Adrenalin | 107 (85.6) |
| Atropine | 67 (53.6) |
| Amiodarone | 4 (3.2) |
| Patients arriving in hospital, n (%) | 61 (48.8) |
| Patients with RSC upon hospital admission | 36 (28.8) |
| Ongoing resuscitation upon admission | 25 (20) |
ECT: emergency care team; OTI: orotracheal intubation; CA: cardiac arrest; RSC: recovery of spontaneous circulation.
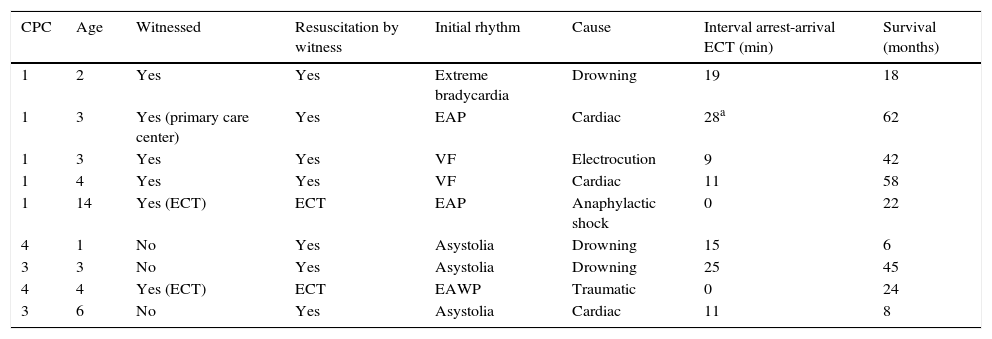
Of the 9 patients (7.2%) alive at hospital discharge, 5 experienced full recovery (CPC1), while four suffered severe neurological sequelae (CPC3–4).
The following results were recorded over follow-up: the 5 patients with CPC1 maintained this status 18, 22, 42, 58 and 62 months after the event, respectively. The four patients with CPC3–4 neurological impairment were alive and presented discrete improvement of their neurological status (all four corresponded to CPC3) after a period of 6, 8, 24 and 45 months, respectively. The characteristics of these patients are described in Table 3.
Characteristics of the survivors at hospital discharge.
| CPC | Age | Witnessed | Resuscitation by witness | Initial rhythm | Cause | Interval arrest-arrival ECT (min) | Survival (months) |
|---|---|---|---|---|---|---|---|
| 1 | 2 | Yes | Yes | Extreme bradycardia | Drowning | 19 | 18 |
| 1 | 3 | Yes (primary care center) | Yes | EAP | Cardiac | 28a | 62 |
| 1 | 3 | Yes | Yes | VF | Electrocution | 9 | 42 |
| 1 | 4 | Yes | Yes | VF | Cardiac | 11 | 58 |
| 1 | 14 | Yes (ECT) | ECT | EAP | Anaphylactic shock | 0 | 22 |
| 4 | 1 | No | Yes | Asystolia | Drowning | 15 | 6 |
| 3 | 3 | No | Yes | Asystolia | Drowning | 25 | 45 |
| 4 | 4 | Yes (ECT) | ECT | EAWP | Traumatic | 0 | 24 |
| 3 | 6 | No | Yes | Asystolia | Cardiac | 11 | 8 |
EAP: electrical activity with pulse; EAWP: electrical activity without pulse; CPC: Cerebral Performance Category; ECT: emergency care team; VF: ventricular fibrillation.
The present study describes the results of the largest series of out-of-hospital CA episodes in the pediatric population in Spain. The proportion of pediatric/adult CA in our series is similar to that published by other registries, taking into account the differences in defining the age groups.3,6 Likewise, overall survival was consistent with the data from other similar series,13 and lower than in our adult population.8 Most of the CA episodes occurred outside the home, though close to 50% were not witnessed. Despite these data, resuscitation maneuvers were started in two-thirds of the cases before the arrival of the ECT–probably because a proportion of arrests occurred in primary care centers and others were directly referred to these centers before the ECT arrived. One-half of the patient reached the hospital, though one out of every 5 of these individuals did so without a spontaneous pulse and under conditions of ongoing resuscitation maneuvering–this being known to imply a poor prognosis.14,15 This circumstance, which greatly exceeds what is seen in adults, is probably related to the known difficulty of deciding resuscitation cessation in children.16 Although the time of death cannot be established, the fact is that none of the patients with ongoing resuscitation maneuvering received hospital discharge.
In the same way as in other series from different countries, an initial defibrillable rhythm is infrequent,5,17,18 and this undoubtedly exerts an influence upon the low general survival rates observed at this age. In fact, asystolia was not the initial condition in any of the cases with a favorable neurological outcome.
All the survivors underwent life support maneuvering before arrival of the ECT, and CA was witnessed in the 5 cases resulting in full recuperation. One arrest of traumatic origin was also witnessed by the ECT. Although this patient survived, long-term sequelae resulted (CPC3)–this being expected, considering the poor general prognosis of CA of this kind.19
An important number of cases were classified as being of unknown cause, and although in adults CA is usually attributed to cardiac causes, the same does not apply to pediatric patients, where a low diagnostic correlation has been evidenced in the absence of an apparent cause of CA.20 There was moreover important uncertainty in estimating the time of arrest – this reflecting the difficulty of establishing the time of the event when CA is not witnessed.
Survival among out-of-hospital CA victims is low. Although a significant percentage of patients reach hospital, the long-term outcome is disappointing, independently of adherence of the pre-hospital basic, airway and drug measures (Table 2) to the international recommendations.21 The results are probably influenced by the difficulty of treating the cause of CA, e.g., percutaneous coronary intervention in the case of CA of cardiac origin in adults,22 and uncertainty regarding the efficacy of therapeutic hypothermia in pediatric CA.23,24 In fact, in none of the patients in our series was hypothermia used, despite the fact that during the first years of this type of practice there were fewer negative data to feed such controversy.24
A very notorious observation is the marked difference in outcome between pediatric out-of-hospital CA and CA occurring in hospital,25 with percentage results that currently give the impression of being beyond reach. Nevertheless, considering that the data are referred to a single emergency care service (albeit assisting the most populated region in Spain), there might be some variability, as occurs with other general series published in this country.26
A key issue in intervention would be not only to increase the percentage of prior resuscitation maneuvering but also its quality – specifically, performing chest compression with ventilation versus compression alone. This aspect should be stressed when telephone recommendations and instructions are provided from the coordination centers.27,28
Despite the abovementioned data, the neurological status of the pediatric patients that survived out-of-hospital CA was maintained over the long term. The patients discharged from hospital with full recovery maintained that condition. In comparison, although the patients with neurological sequelae showed discrete improvement, they all remained dependent for daily life activities.
Our study has a number of limitations. Although patients are entered prospectively in the registry, in chronological order, the data were analyzed on a retrospective basis. Certain variables with missing information in turn can condition the results. In this regard, missing information referred to the time of arrest limits analysis of the influence of the time interval between collapse and the start of resuscitation. Although this is a common limitation in most registries, it constitutes a key variable in relation to the outcome of CA. On the other hand, the registry is characterized by an automatic case inclusion system, and although quality control measures have been implemented, it is not possible to discard errors attributable to defective case coding, which would result in the non-inclusion of some patients.
Although the study series was very large considering the age group involved, the small number of patients who finally survived did not advise any correlating analysis between variables and outcome. Lastly, this is a general CA registry, not a specific registry of pediatric CA, and is moreover confined to a regional setting. The results obtained therefore might not be extendable to the rest of Spain.
Our results demonstrate the need to maintain follow-up and to analyze the evolution of pediatric patients with out-of-hospital CA, in order to incorporate improvements in their integral care. Research focusing on measures capable of guaranteeing previous resuscitation of better quality could increase the chances for success of a series of hospital care measures which, at least for the time being, lack protocols specifically targeted to patients of this age.
Financial supportThe Andalusian Out-of-Hospital Cardiac Arrest Registry (Registro Andaluz de Parada Cardíaca Extrahospitalaria) was implemented through a research grant from the Fondo de Investigaciones Sanitarias, Instituto Carlos III, and is maintained through proprietary funding from the EPES.
Conflict of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Rosell-Ortiz F, Mellado-Vergel FJ, López-Messa JB, Fernández-Valle P, Ruiz-Montero MM, González-Lobato I, et al. Supervivencia y estado neurológico de la parada cardiaca extrahospitalaria en edad pediátrica en Andalucía. Med Intensiva. 2016;40:163–167.