Prone position ventilation has been shown to improve oxygenation and ventilatory mechanics in patients with acute respiratory distress syndrome. We evaluated whether prone ventilation reduces the risk of mortality in adult patients with acute respiratory distress syndrome versus supine ventilation.
MethodologyA meta-analysis of randomized controlled trials comparing patients in supine versus prone position was performed. A search was conducted of the Pubmed, Embase, Cochrane Library, and LILACS databases. Mortality, hospital length of stay, days of mechanical ventilation and adverse effects were evaluated.
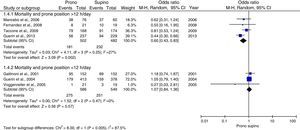
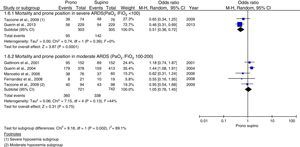
ResultsSeven randomized controlled trials (2119 patients) were included in the analysis. The prone position showed a nonsignificant tendency to reduce mortality (OR: 0.76; 95%CI: 0.54–1.06; p=0.11, I2 63%). When stratified by subgroups, a significant decrease was seen in the risk of mortality in patients ventilated with low tidal volume (OR: 0.58; 95%CI: 0.38–0.87; p=0.009, I2 33%), prolonged pronation (OR: 0.6; 95%CI: 0.43–0.83; p=0.002, I2 27%), start within the first 48h of disease evolution (OR 0.49; 95%CI 0.35–0.68; p=0.0001, I2 0%) and severe hypoxemia (OR: 0.51: 95%CI: 0.36–1.25; p=0.0001, I2 0%). Adverse effects associated with pronation were the development of pressure ulcers and endotracheal tube obstruction.
ConclusionsProne position ventilation is a safe strategy and reduces mortality in patients with severely impaired oxygenation. It should be started early, for prolonged periods, and should be associated to a protective ventilation strategy.
La ventilación en posición prona ha demostrado mejorar la oxigenación y la mecánica pulmonar en pacientes con síndrome de dificultad respiratoria aguda. Nosotros evaluamos si la posición prona disminuye el riesgo de mortalidad en pacientes adultos con síndrome de dificultad respiratoria aguda versus ventilación en posición supina.
MetodologíaSe realizó un metanálisis de ensayos clínicos controlados aleatorizados que compararon pacientes en posición prona versus supina. Se realizó una búsqueda en Pubmed, Embase, Cochrane Library y LILACS. Se evaluó mortalidad, estancia hospitalaria, días de ventilación mecánica y efectos adversos.
ResultadosSiete ensayos clínicos controlados aleatorizados (2.119 pacientes) fueron incluidos en el análisis. La posición prona mostró una tendencia no significativa a disminuir la mortalidad (OR: 0,76; IC 95%: 0,54–1,06; p=0,11; I2 63%). Al estratificar por subgrupos se encontró una disminución significativa en el riesgo de mortalidad en los pacientes ventilados con volumen corriente bajo (OR: 0,58; IC 95%: 0,38–0,87; p=0,009; I2 33%), pronación prolongada (OR: 0,6; IC 95%: 0,43–0,83; p=0,002; I2 27%), instauración antes de 48h de evolución de la enfermedad (OR: 0,49; IC 95%: 0,35–0,68; p=0,0001; I2 0%) e hipoxemia severa (OR: 0,51; IC 95%: 0,36–1,25; p=0,0001; I2 0%). Los efectos adversos relacionados con la pronación fueron el desarrollo de úlceras por presión y obstrucción del tubo orotraqueal.
ConclusionesLa ventilación en posición prona es una estrategia segura y disminuye la mortalidad en los pacientes con compromiso severo de la oxigenación, debe ser instaurada tempranamente, durante periodos prolongados y asociada a una estrategia de ventilación protectora.
Clinical studies have found that patients with acute respiratory distress syndrome (ARDS) account for approximately 5% of all hospitalized patients subjected to mechanical ventilation.1 Most studies have shown that patients with mild ARDS (PaO2/FiO2 200–300) represent only 25% of the cases, while the remaining 75% correspond to patients with moderate or severe ARDS.1,2 Acute respiratory distress syndrome is associated to an in-hospital mortality rate of approximately 40%.2,3 The mortality rate in turn is conditioned to the severity of the oxygenation defect. In the Berlin definition clinical trial, the mortality rate was found to be 27% in patients with mild ARDS, 32% in cases of moderate ARDS, and 45% in those with severe ARDS.4 Although the deterioration of oxygenation is a mortality risk factor in ARDS, patients generally die as a consequence of multiorgan failure, and only a minority (13–19%) die as a result of refractory hypoxemia.3,5 Although the mortality rate has decreased in the last few decades, probably due to the adoption of protective ventilation strategies (low tidal volume, optimum PEEP level, and limitation of plateau pressure), which lessen ventilator-associated lung injury,6,7 the fatality statistics have remained stable in recent years,2,3,5 without additional reductions in patients of this kind. It is therefore essential to establish other strategies or treatments that may result in further significant reductions in patient mortality.7
Mechanical ventilation in the prone position has been used for several decades in patients with ARDS with the purpose of improving oxygenation.8 It is currently well recognized that the prone position is associated to important improvements in the oxygenation indices when compared with the supine position. Furthermore, different studies in animals and humans have found that the prone position can reduce ventilator-associated lung injury.9 A number of clinical trials have been made with the aim of extrapolating these results to the clinical setting,10–15 though none of them have clearly demonstrated a positive impact upon patient survival.16 Likewise, the meta-analyses and systematic reviews published to date only suggest a tendency to reduce mortality in patients with severely impaired oxygenation.5,9,17–23 However, in the time elapsed from the first clinical trial10 to the most recent study,16 there have been important changes in ventilation and pronation strategies, as described in the latest study by Guerin et al.,16 where notorious benefit in terms of survival was documented among patients in the prone position – with an absolute decrease in mortality risk of 37%.
In the light of the fact that few strategies have had an impact upon survival in patients with ARDS, it is important that ventilation in the prone position has reappeared with strong results. However, because of the changes in pronation strategy and in the patient inclusion criteria in the most recent studies, we considered it necessary to determine the true impact of pronation, and to define which patients can benefit from it. A meta-analysis was therefore conducted with the primary objective of determining whether ventilation in the prone position reduces mortality in patients with ARDS compared with traditional ventilation in the supine position. As a secondary objective we described the groups of patients that show a positive impact upon survival and the parameters to be applied during the use of this ventilation strategy (timing of the start, daily duration, associated management strategies, etc.). Lastly, based on the results obtained, we aimed to offer a series of evidence-based recommendations on the use of ventilation in the prone position in patients with ARDS.
Material and methodsTypes of studiesWe included randomized, controlled clinical trials comparing mechanical ventilation in the prone position versus conventional mechanical ventilation in the supine position in adult patients meeting the Berlin criteria for ARDS.4 We also included patients classified as presenting acute lung injury (ALI)(PaO2/FiO2 200–300mmHg) according to the American–European ARDS consensus Conference of 1994.24
Types of patientsWe included studies that evaluated patients over 16 years of age meeting the diagnostic criteria for ARDS, compared results between ventilation in the prone position versus the supine position, and evaluated mortality.
Studies in the pediatric population (under 16 years of age) were excluded, as were studies in animals or which used airway pressure release ventilation (APRV), high-frequency oscillation ventilation (HFOV) or inhaled nitric oxide.
Interventions and outcomesThe interventions evaluated were ventilation in the prone position and conventional ventilation in the supine position.
The following outcomes were assessed:
- 1.
Mortality after maximum follow-up
- 2.
Stay in intensive care (days)
- 3.
Days on mechanical ventilation
- 4.
Adverse effects and complications:
- –
Ventilator-associated pneumonia (VAP)
- –
Accidental or non-scheduled extubation
- –
Tube displacement or selective intubation
- –
Tube obstruction
- –
Appearance of pressure ulcers
- –
Pneumothorax during pronation
- –
Venous access loss
- –
The outcomes were stratified by patient subgroups and were predefined taking into account the degree of hypoxemia,4 the use of protective ventilation,6 the duration of ARDS and the daily pronation time.10,20,25 These factors probably have a decisive influence upon the results of ventilation in the prone position.9,17,18,21,22,26–32 The subgroups were stratified as follows:
- 1
Severity of ARDS (Berlin classification)
- –
Mild (PaO2/FiO2 200–300mmHg)
- –
Moderate (PaO2/FiO2 100–200mmHg)
- –
Severe (PaO2/FiO2<100mmHg)
- –
- 2
Daily duration of pronation
- –
Less than 12h/day
- –
More than 12h/day
- –
- 3
Start of pronation and duration of ARDS
- 4
Tidal volume used
- –
Less than 8ml/kg ideal weight
- –
More than 8ml/kg ideal weight
- –
A literature search was made of the PubMed, EMBASE, Cochrane Library and LILACS databases, combining Mesh terms and Keywords: “Prone Position”[Mesh], “Prone Positioning”, “Respiratory Distress Syndrome, Adult”[Mesh], “Acute Respiratory Distress Syndrome”, “ARDS”, “Acute Respiratory Failure”, “Acute Lung Injury”, “Clinical Trial” [Publication Type], “Controlled Clinical Trial” [Publication Type], “Randomized Controlled Trial” [Publication Type], “Clinical Trials as Topic”[Mesh], “Comparative Study” [Publication Type], “Multicenter Study” [Publication Type], “Multicenter Studies as Topic”[Mesh]. The search was limited to the period between 1 January 1974 and 31 December 2013, with no language restrictions.
Data extraction and analysisIdentification of trials and data extractionTwo authors (J. Mora and O. Bernal) independently screened the titles and abstracts identified by the search, selecting those studies that met the established inclusion criteria. Information was extracted regarding the study design, randomization procedure, blinding, patient characteristics, inclusion and exclusion criteria, interventions and results. Any disagreements were resolved through examination of the information by a third reviewer (S. Rodriguez).
Quality assessmentThe assessment tool recommended by the Cochrane Collaboration33 was used to evaluate the risk of bias that referred to:
- 1.
Random sequence generation
- 2.
Allocation concealment
- 3.
Blinding of participants and evaluators
- 4.
Incomplete results
- 5.
Selective reporting of results
- 6.
Other sources of bias
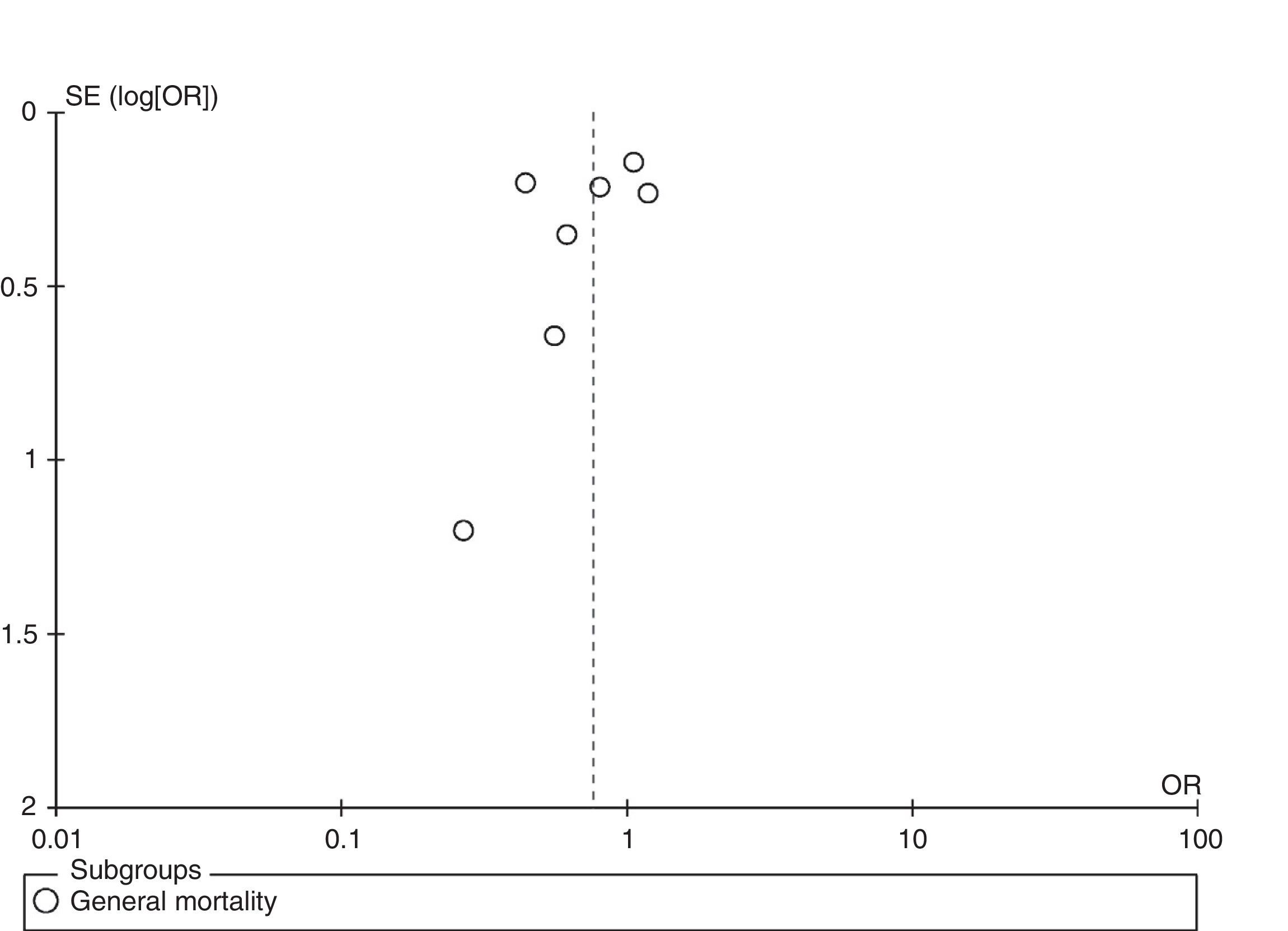
The data from the included studies were qualitatively and quantitatively analyzed per population, intervention and result using the RevMan 5.2 freeware statistical package from the Cochrane Informatics and Knowledge Management Department (http://tech.cochrane.org/). The results were quantified and analyzed on an intention-to-treat (ITT) basis; relative heterogeneity was measured with the I2 statistic; and statistical significance was examined using the chi-squared test. Dichotomic results were assessed based on the odds ratio (OR) with the Mantel–Haenszel test and a random effects model. In the case of continuous variables, we calculated the difference in means based on the inverse variance method with a random effects model. Publication bias in turn was assessed by funnel plot analysis, and a sensitivity analysis was made to assess the certainty of the results.
The study protocol was not registered.
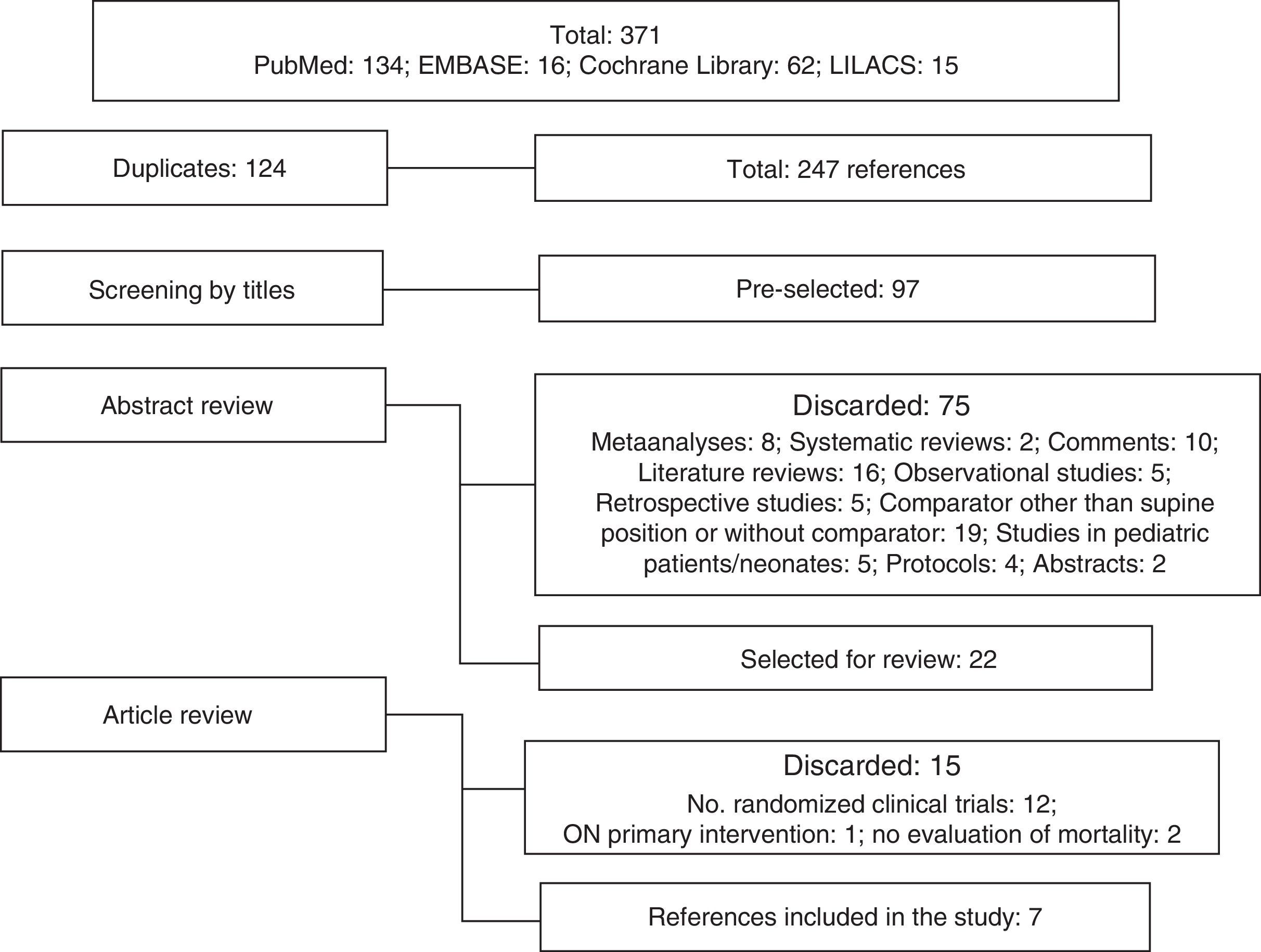
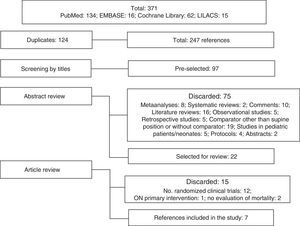
ResultsA total of 371 literature references were identified: PubMed n=134, EMBASE n=160, Cochrane Library n=62 and LILACS n=15. We discarded 124 due to duplication. Twenty-two references were fully reviewed, and of these 7 met the study inclusion criteria (Fig. 1).
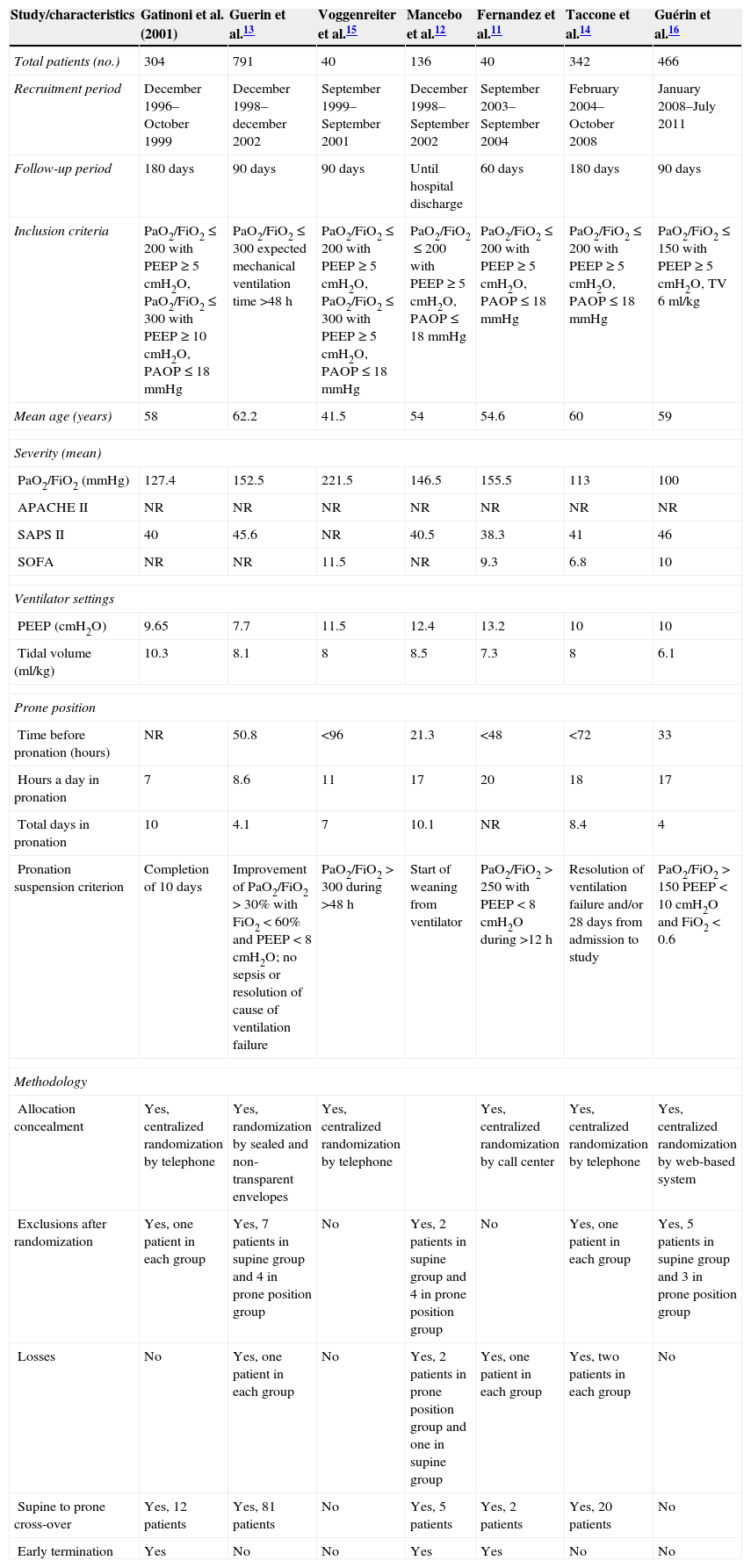
Characteristics of the studiesThe patient population totaled 2119, of which 1088 were ventilated in the prone position and 1031 in the supine position. The recruitment period of four studies10,12,13,15 preceded publication of the results of the ARDS network study6 (which demonstrated a decrease in mortality risk in patients ventilated with low tidal volumes). In general, these studies used tidal volumes greater than those currently recommended.
The severity of the disease and the mortality risk predicted by the SAPS II were similar in all 7 studies. The four most recent studies only included patients with PaO2/FiO2<200, i.e., with more severely impaired oxygenation.11,12,14,16 Likewise, the number of hours a day in the prone position was found to increase (from 7–11 to 17–20h/day). The changes in mechanical ventilation protocol were also seen to be related to the time of publication: the three studies that started the recruitment period after publication of the ARDS network study6 used a tidal volume of 6–8ml/kg.11,14–16 The administered PEEP was generally low. No single protocol for deciding the time of pronation suspension was found. Table 1 shows the general characteristics of the studies.
Summarized characteristics of the studies.
| Study/characteristics | Gatinoni et al. (2001) | Guerin et al.13 | Voggenreiter et al.15 | Mancebo et al.12 | Fernandez et al.11 | Taccone et al.14 | Guérin et al.16 |
|---|---|---|---|---|---|---|---|
| Total patients (no.) | 304 | 791 | 40 | 136 | 40 | 342 | 466 |
| Recruitment period | December 1996–October 1999 | December 1998–december 2002 | September 1999–September 2001 | December 1998–September 2002 | September 2003–September 2004 | February 2004–October 2008 | January 2008–July 2011 |
| Follow-up period | 180 days | 90 days | 90 days | Until hospital discharge | 60 days | 180 days | 90 days |
| Inclusion criteria | PaO2/FiO2≤200 with PEEP≥5cmH2O, PaO2/FiO2≤300 with PEEP≥10cmH2O, PAOP≤18mmHg | PaO2/FiO2≤300 expected mechanical ventilation time >48h | PaO2/FiO2≤200 with PEEP≥5cmH2O, PaO2/FiO2≤300 with PEEP≥5cmH2O, PAOP≤18mmHg | PaO2/FiO2≤200 with PEEP≥5cmH2O, PAOP≤18mmHg | PaO2/FiO2≤200 with PEEP≥5cmH2O, PAOP≤18mmHg | PaO2/FiO2≤200 with PEEP≥5cmH2O, PAOP≤18mmHg | PaO2/FiO2≤150 with PEEP≥5cmH2O, TV 6ml/kg |
| Mean age (years) | 58 | 62.2 | 41.5 | 54 | 54.6 | 60 | 59 |
| Severity (mean) | |||||||
| PaO2/FiO2 (mmHg) | 127.4 | 152.5 | 221.5 | 146.5 | 155.5 | 113 | 100 |
| APACHE II | NR | NR | NR | NR | NR | NR | NR |
| SAPS II | 40 | 45.6 | NR | 40.5 | 38.3 | 41 | 46 |
| SOFA | NR | NR | 11.5 | NR | 9.3 | 6.8 | 10 |
| Ventilator settings | |||||||
| PEEP (cmH2O) | 9.65 | 7.7 | 11.5 | 12.4 | 13.2 | 10 | 10 |
| Tidal volume (ml/kg) | 10.3 | 8.1 | 8 | 8.5 | 7.3 | 8 | 6.1 |
| Prone position | |||||||
| Time before pronation (hours) | NR | 50.8 | <96 | 21.3 | <48 | <72 | 33 |
| Hours a day in pronation | 7 | 8.6 | 11 | 17 | 20 | 18 | 17 |
| Total days in pronation | 10 | 4.1 | 7 | 10.1 | NR | 8.4 | 4 |
| Pronation suspension criterion | Completion of 10 days | Improvement of PaO2/FiO2>30% with FiO2<60% and PEEP<8 cmH2O; no sepsis or resolution of cause of ventilation failure | PaO2/FiO2>300 during >48h | Start of weaning from ventilator | PaO2/FiO2>250 with PEEP<8cmH2O during >12h | Resolution of ventilation failure and/or 28 days from admission to study | PaO2/FiO2>150 PEEP<10cmH2O and FiO2<0.6 |
| Methodology | |||||||
| Allocation concealment | Yes, centralized randomization by telephone | Yes, randomization by sealed and non-transparent envelopes | Yes, centralized randomization by telephone | Yes, centralized randomization by call center | Yes, centralized randomization by telephone | Yes, centralized randomization by web-based system | |
| Exclusions after randomization | Yes, one patient in each group | Yes, 7 patients in supine group and 4 in prone position group | No | Yes, 2 patients in supine group and 4 in prone position group | No | Yes, one patient in each group | Yes, 5 patients in supine group and 3 in prone position group |
| Losses | No | Yes, one patient in each group | No | Yes, 2 patients in prone position group and one in supine group | Yes, one patient in each group | Yes, two patients in each group | No |
| Supine to prone cross-over | Yes, 12 patients | Yes, 81 patients | No | Yes, 5 patients | Yes, 2 patients | Yes, 20 patients | No |
| Early termination | Yes | No | No | Yes | Yes | No | No |
NR: not reported; PAOP: pulmonary artery occlusion pressure; PaO2/FiO2: ratio between partial pressure of oxygen in arterial blood and fraction of inspired oxygen; PEEP: positive end-expiratory pressure; TV: tidal volume.
All the included studies were randomized, controlled clinical trials. Randomization was carried out on a centralized basis by telephone or sealed and non-transparent envelopes. Given the nature of the intervention subjected to evaluation, it was not possible to blind the patients or the treating medical team–though we consider that this had no effect upon the results. Furthermore, with the exception of a single study,13 the group handling the information of the patients and the results of the analyses was independent and blinded to the treatment groups. No significant losses were reported in the studies, and exclusions after randomization were also few (being mainly due to secondary withdrawal of consent and inclusion error). Three studies ended prematurely. 10–12We therefore could not obtain an adequate sample for identifying probable differences with optimum statistical power.
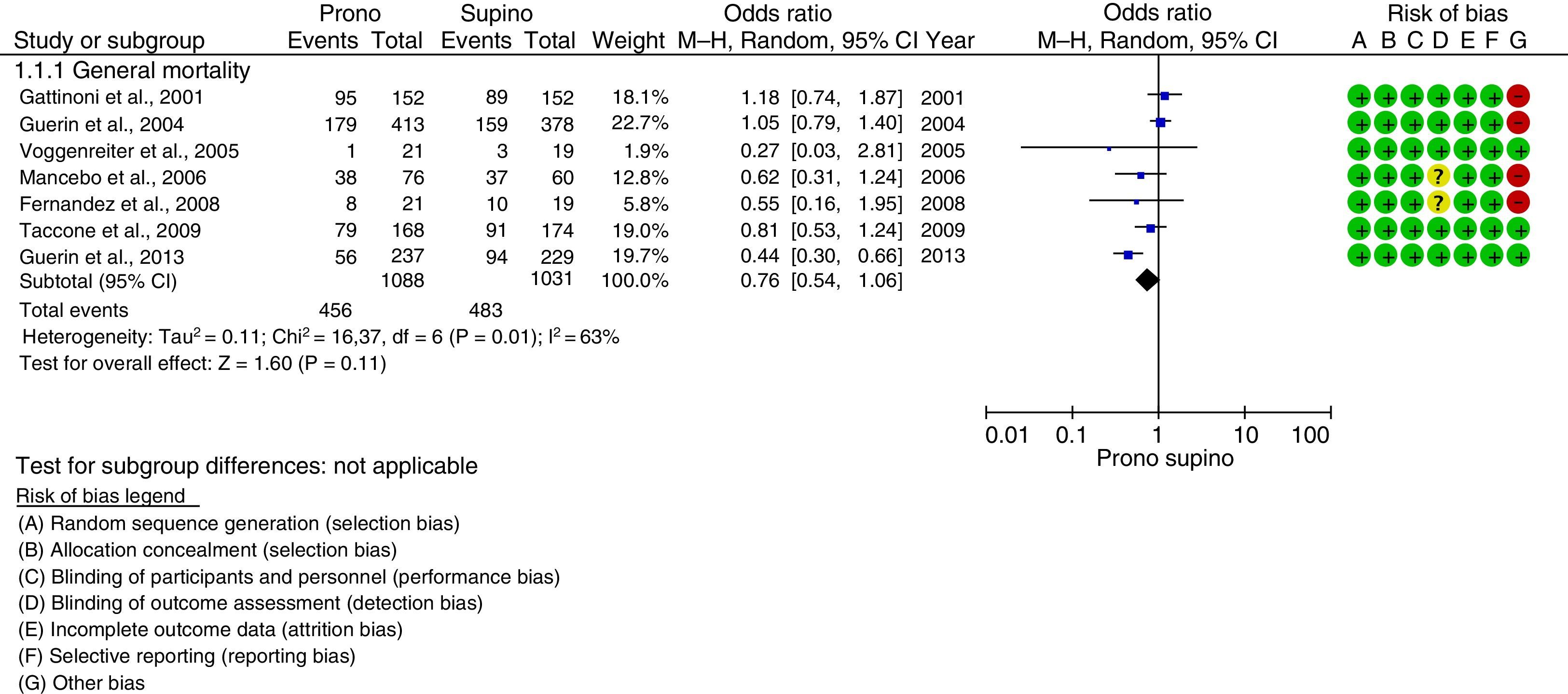
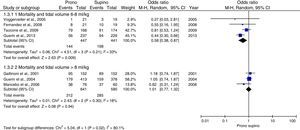
Prone position and mortalityGlobal mortalityA total of 456 events were recorded in the prone position group (41.9%), versus 483 in the supine position group (46.8%), with an OR of 0.76 (95%CI: 0.54–1.06; p=0.11; I2 63%) showing a tendency in favor of the prone position group–though statistical significance was not reached (Fig. 2). Since the studies had different follow-up periods, and we used the final report on events at the end of this period for the global result, the findings were stratified and evaluated in different time periods: after 28 days (OR: 0.73; 95%CI: 0.41–1.32; p=0.3; I2 85%), after 90 days (OR: 0.64; 95%CI: 0.29–1.40; p=0.26; I2 84%) and after 180 days (OR: 0.97; 95%CI: 0.67–1.40; p=0.26; I2 28%), together with mortality in intensive care (OR: 0.86; 95%CI: 0.61–1.22; p=0.4; I2 31%)–no significant differences being found in each of the groups.
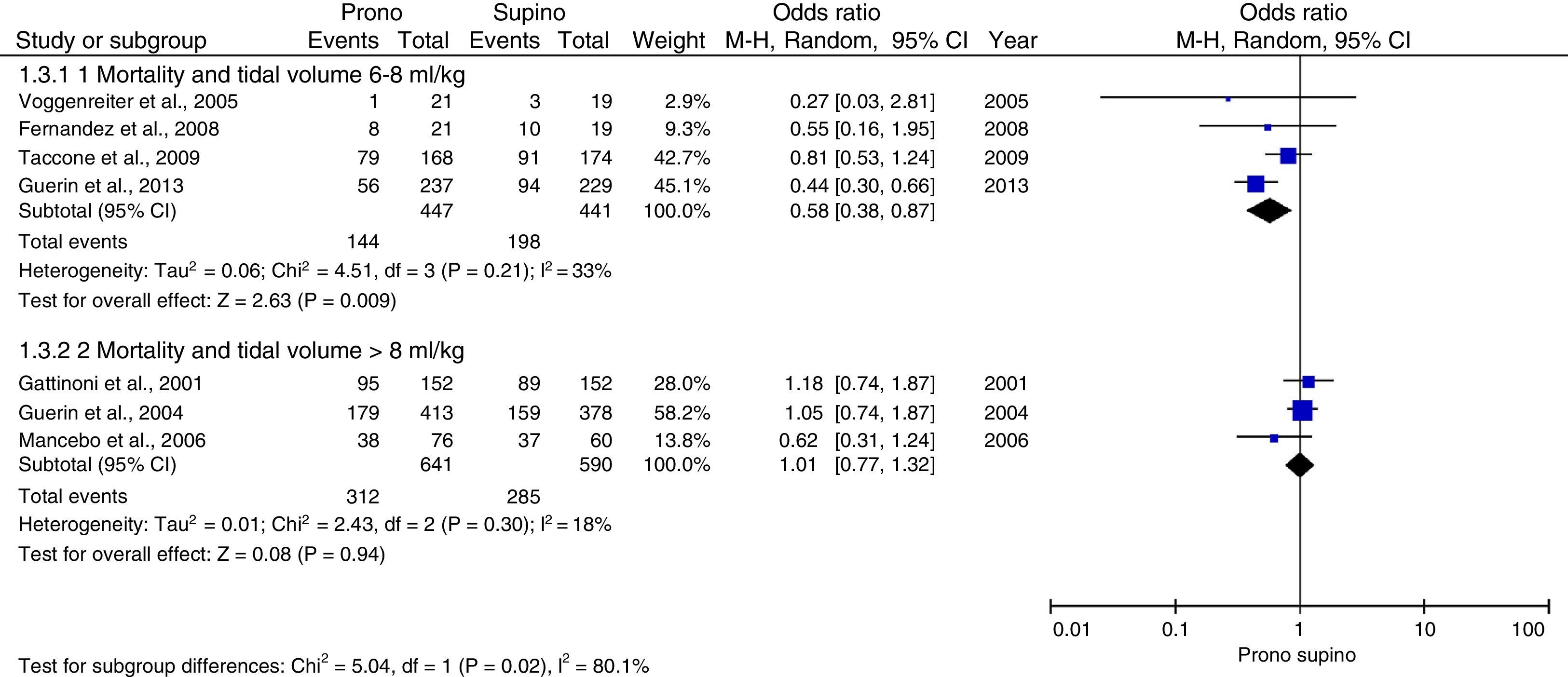
Mortality and protective ventilationOn examining the association between mortality and the administered tidal volume, stratification into two groups was made according to whether a low tidal volume was used as part of a protective ventilation strategy, or a high tidal volume was administered (the latter appearing to be related to the development of ventilator-associated lung injury). Four studies11,14–16 used a tidal volume 8ml/kg ideal weight, showing a decrease in mortality risk of 36% (OR: 0.58; 95%CI: 0.38–0.87; p=0.009; I2 33%). This finding was not obtained when using a tidal volume >8ml/kg ideal weight (OR: 1.01; 95%CI: 0.77–1.32; p=0.94; I2 18%) (Fig. 3).
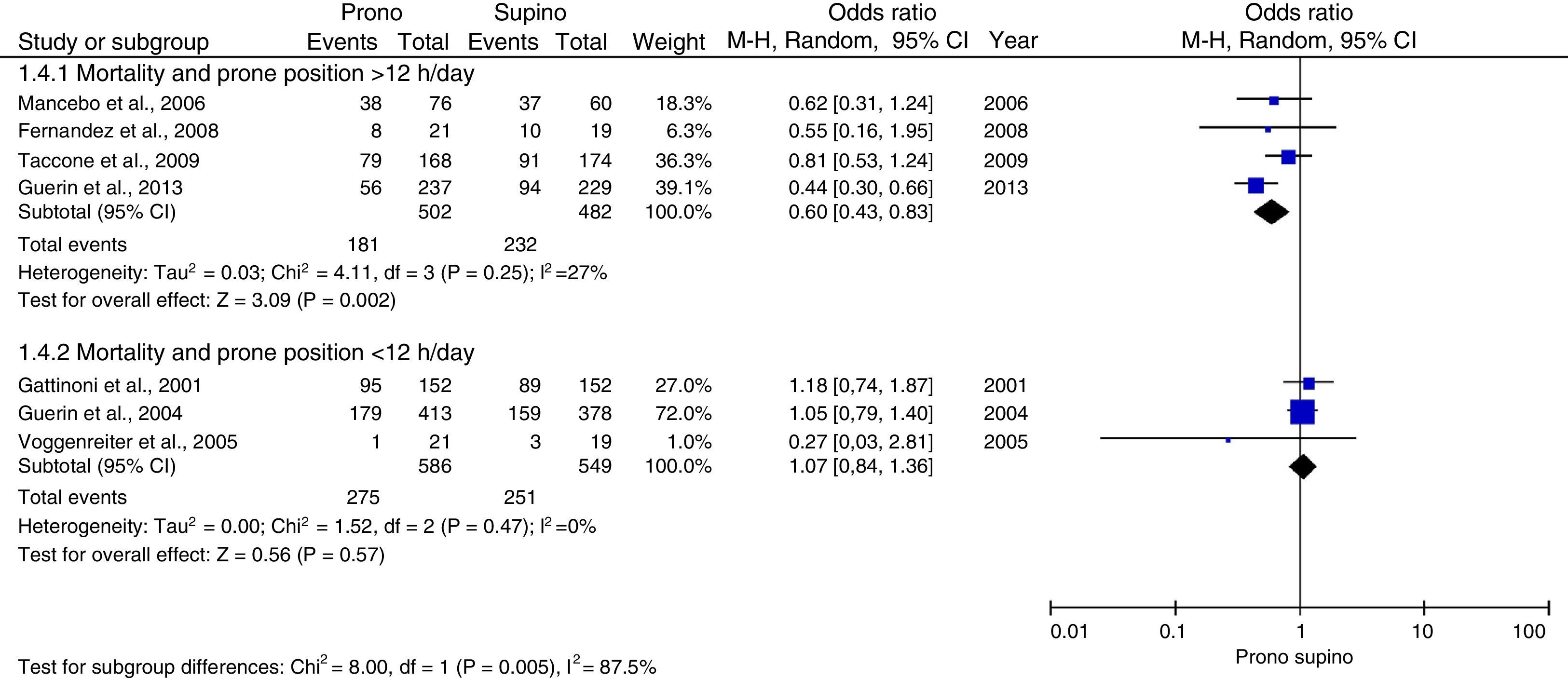
Mortality and number of hours a day in the prone positionAll the studies reported and analyzed data regarding the duration of pronation. In the four most recent publications11,12,14,16 the number of daily hours was increased (18h on average)–this resulting in a significant decrease in event risk in favor of the group of patients placed in the prone position for more than 12h (OR: 0.6; 95%CI: 0.43–0.83; p=0.002; I2 27%) (Fig. 4).
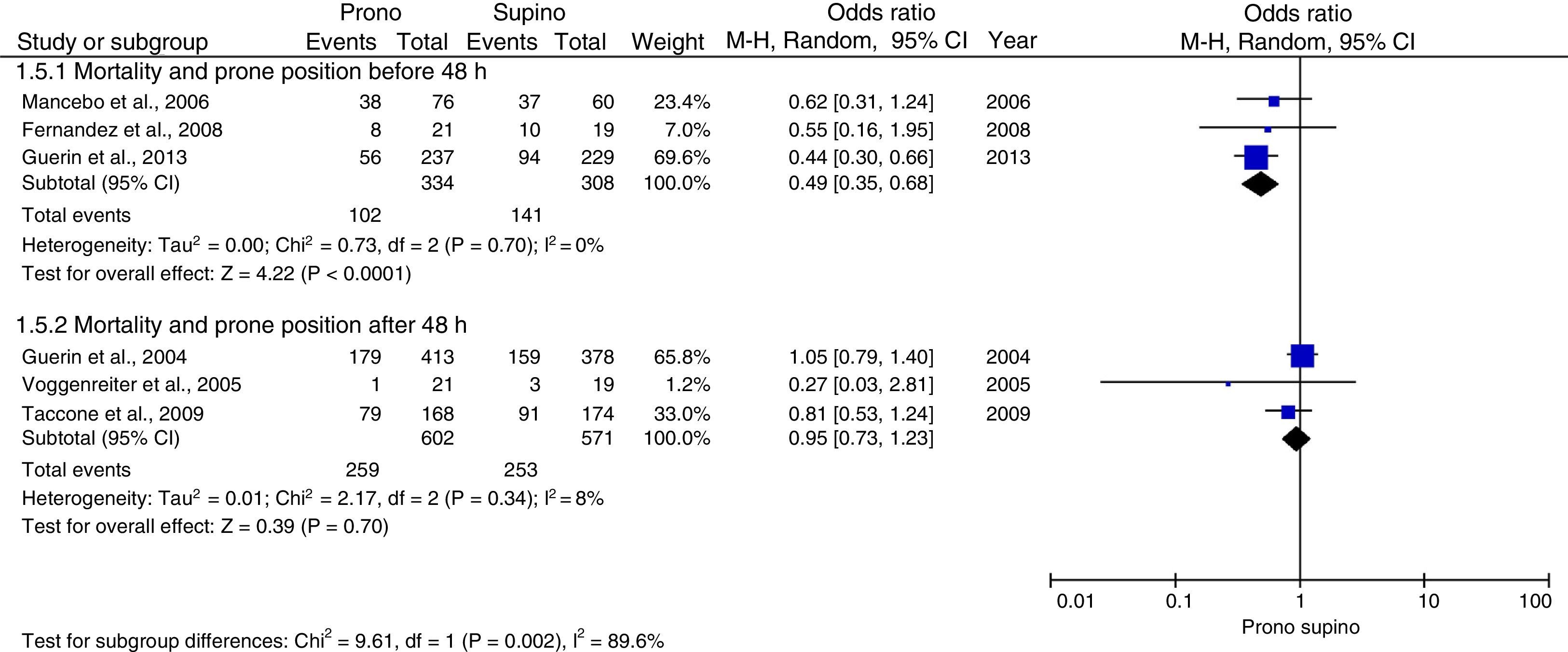
Mortality and start of pronationIn the same way that the number of hours in the prone position appears to be important, so does the timing of the start of patient placement in the prone position. In effect, greater benefit was observed when the patients were placed in the prone position within the first 48h after the start of mechanical ventilation, with an OR of 0.49 (95%CI: 0.35–0.68, p=0.0001; I2 0%) (Fig. 5).
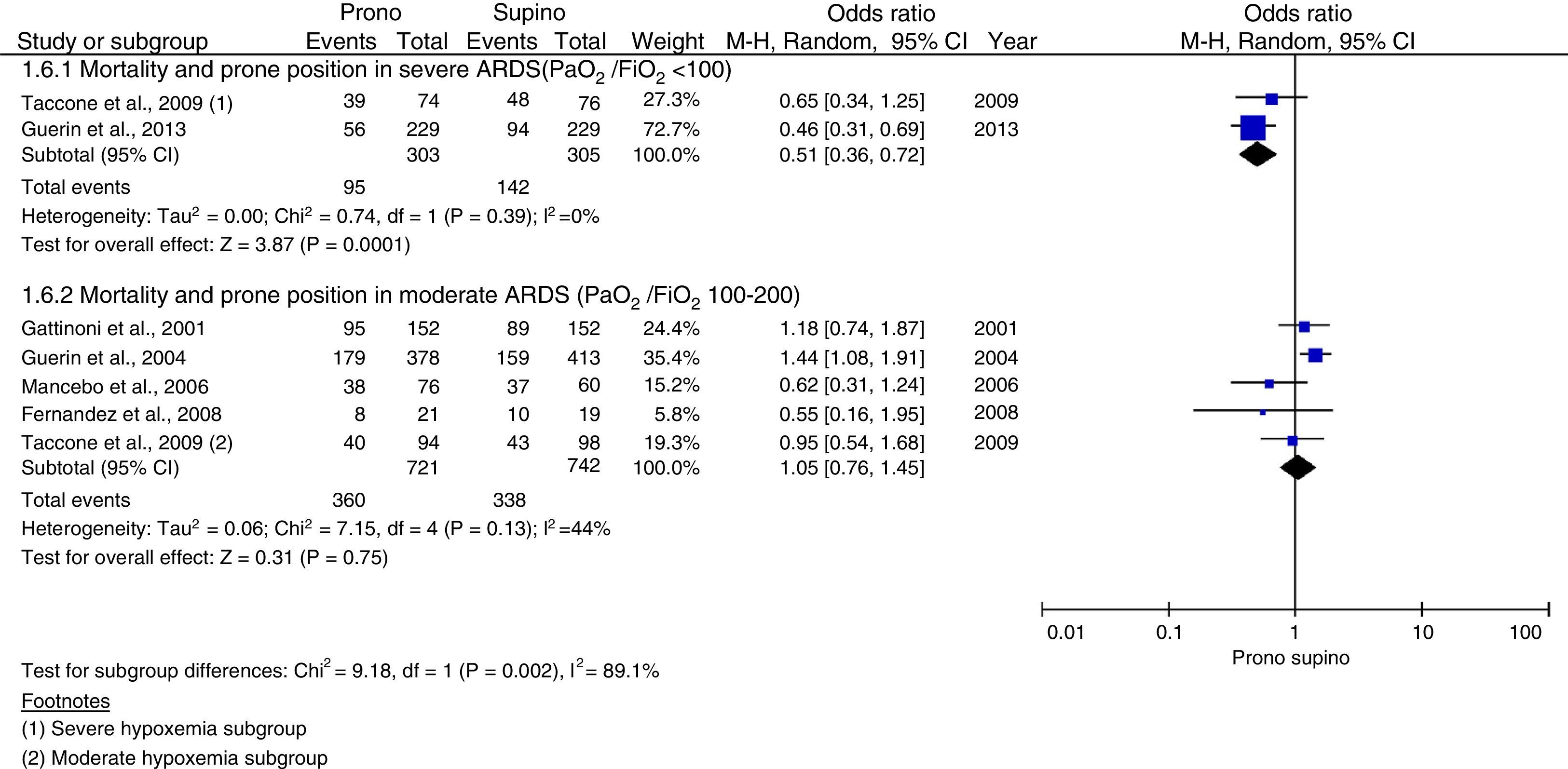
Mortality and severity of hypoxemiaThe studies were stratified according to the severity of hypoxemia: moderate (PaO2/FiO2 100–200) or severe (PaO2/FiO2<100). Taccone et al. stratified the population into these two groups; their data were therefore taken separately for analysis. The study published by Voggenreiter et al. reported patients with PaO2/FiO2>200. Five studies10–14 documented patients with moderate hypoxemia, while two studies14,16 reported patients with severe hypoxemia. On performing the meta-analysis, the group with severely impaired oxygenation showed clear benefit with the prone position (OR: 0.51; 95%CI: 0.36–1.25; p=0.0001; I2 0%) (Fig. 6).
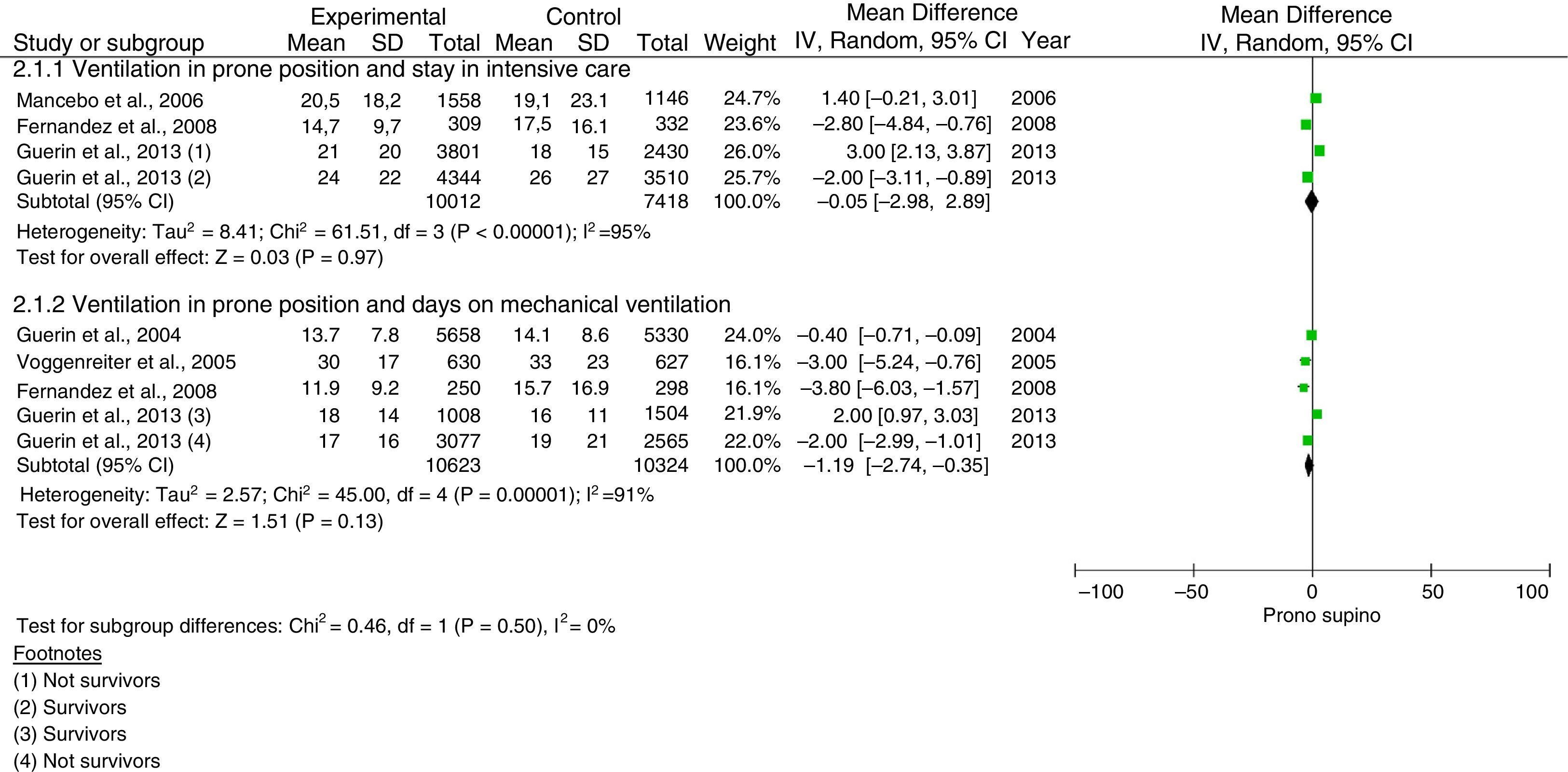
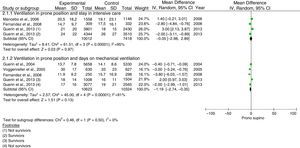
Prone position, stay in intensive care and days on mechanical ventilationFour studies reported the stay in intensive care,11,12,14,16 and 5 studies11,13–16 recorded the days on mechanical ventilation. Analysis was discarded in both cases,14 since different measurement units were used. The study published by Guerin et al.16 reported the results in subgroups of survivors and non-survivors. No differences were found in the results between the two studied groups (stay in intensive care: difference of means −0.05; 95%CI: −2.98–2.89; p=0.00001; I2 95%, and days on mechanical ventilation: difference of means −1.19; 95%CI: −2.74–0.35; p=0.00001; I2 91%) (Fig. 7).
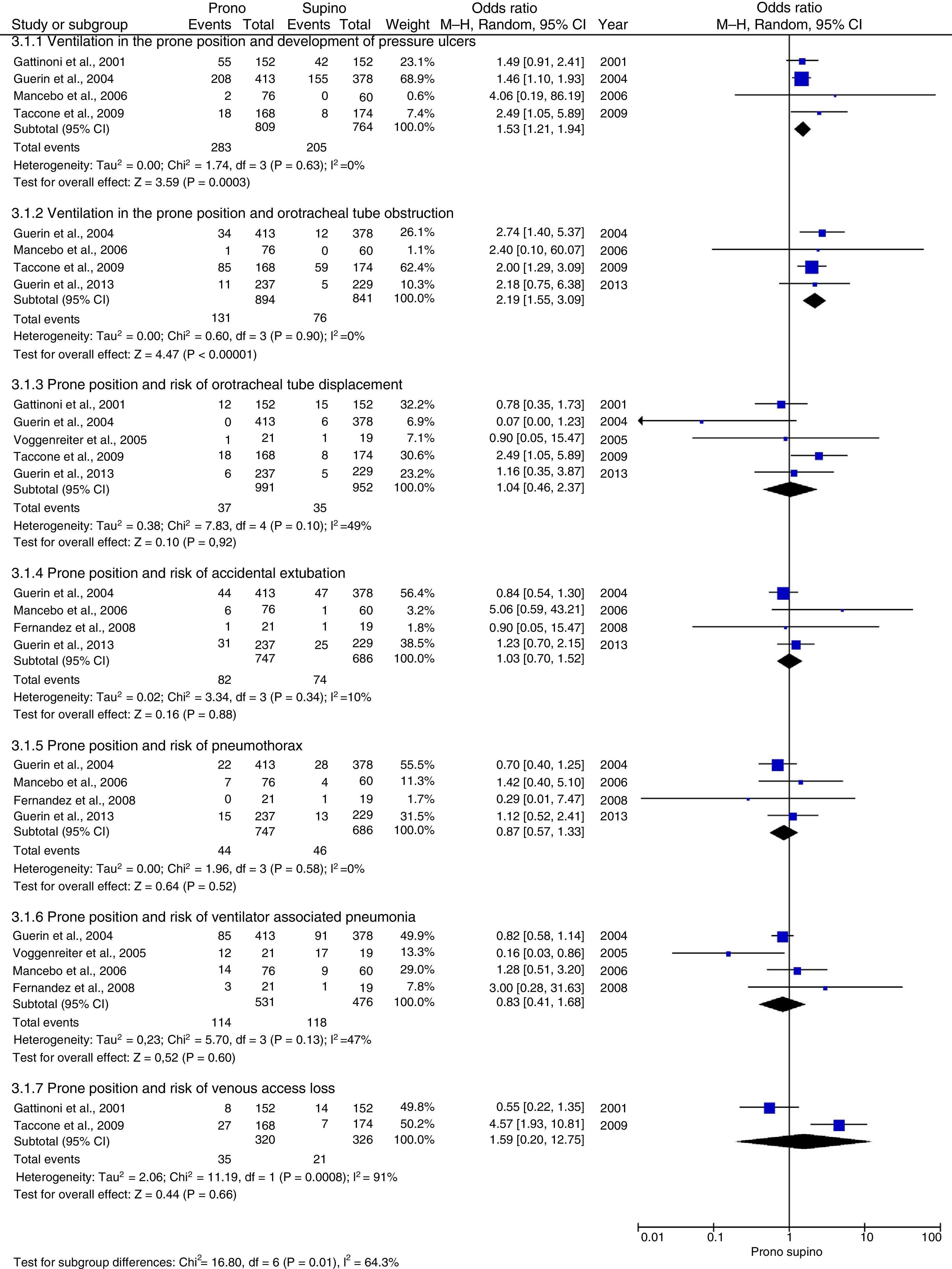
Prone position and adverse effectsPressure ulcers were the most frequent adverse events (34%), followed by ventilator-associated pneumonia (21.4%), orotracheal tube obstruction (14.6%), accidental extubation (10.9%), venous access loss (10.9%), pneumothorax (5.8%), and displacement of the orotracheal tube (3.7%).
The prone position was associated to a significantly increased risk of orotracheal tube obstruction (OR: 2.19; 95%CI: 1.55–3.09; p<0.0001; I2 0%) and the development of pressure ulcers (OR: 1.53; 95%CI: 1.21–1.94; p=0.0003; I2 0%). No differences were observed in relation to the rest of the described events (Fig. 8).
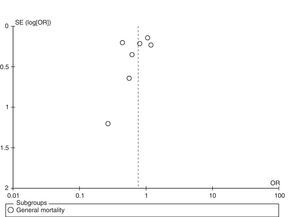
Assessment of publication biasVisual inspection of the funnel plots revealed no evidence of publication bias (Fig. 9).
DiscussionThe primary objective of our study was to examine the impact of mechanical ventilation in the prone position upon mortality in patients with ARDS. Global assessment of the results revealed a nonsignificant tendency to reduce mortality risk in favor of the prone position group. However, on individually analyzing the studies, we found that the most recent trials11,12,14,16 incorporated a number of changes in both the inclusion criteria and in the prone position protocol, based on the analysis of the probable causes underlying the discouraging results recorded in the earlier studies.10,13,15 A first change was the inclusion of more severely compromised patients, with PaO2/FiO2<200, while a second change was the prolongation of pronation time to over 16 consecutive hours a day. A third change was the utilization of protective ventilation strategies with a tidal volume of <8ml/kg ideal weight, the maintenance of a plateau pressure of <30cmH2O, and titration of the optimum PEEP level according to the recommendations of the ARDS network. On examining the studies linearly over time, we observed a tendency to gradually favor the prone position, culminating in the study published by Guerin et al.,16 where a strong reduction in mortality risk was recorded in favor of pronation (HR 0.44; 95%CI: 0.29–0.67; p=0.001 after 90 days). These findings are consistent with those of two recent meta-analyses. The first study was carried out by Beitler et al.,34 who conducted a meta-analysis of individual patient data, including the PROSEVA study,16 assessing mortality after 60 days, with the identification of a nonsignificant tendency in favor of pronation (RR: 0.83; 95%CI: 0.68–1.02; p=0.073). The second study was published by Lee et al.,35 based on broader inclusion criteria and a larger number of studies, and identified a global decrease in mortality risk, though with a confidence interval very close to one (OR: 0.77; 95%CI: 0.59–0.99; p=0.039).
However, interesting data were obtained on stratifying the results by subgroups, supporting our theory regarding the evolution and optimization of the prone position ventilation strategy based on plausible physiology and clear clinical characteristics. Firstly, the utilization of a low tidal volume (<8ml/kg ideal weight) in patients with ARDS became generalized after publication of the ARDS network study6, which revealed a decrease in mortality risk probably related to the generation of lesser mechanical stress upon the alveolar membrane by preventing overdistension and improving alveolar stability.36 This, being associated to recruitment capacity and homogenization of the distribution of ventilation, flow and airway pressures attributed to pronation,37 probably also produce an additive effect in the prevention and reduction of ventilator-associated lung injury. Thus, on evaluating the subgroup of patients in which a tidal volume of <8ml/kg ideal weight was used,11,14–16 a significant decrease in mortality risk was noted in comparison with the group receiving a greater tidal volume10,13,15–these findings possibly being attributable to the decrease in ventilator-associated lung injury. Beitler et al.34 and Lee et al.35 also recorded a significant decrease in mortality risk in those studies that used low tidal volumes (RR: 0.66; 95%CI: 0.5–0.86; p=0.002 and OR: 0.62; 95%CI: 0.48–0.69; p=0.015, respectively). Beitler et al.34 in turn performed a metaregression analysis that revealed a dose–response relationship between the mean basal tidal volume and the relative risk of death after 60 days during pronation. Specifically, a decrease in mean basal tidal volume of 1ml/kg ideal weight was seen to be associated to a 16.7% mortality risk.34
The degree of alveolar recruitment in the prone position also requires consideration. Acute respiratory distress syndrome is characterized by disruption of the alveolar-capillary barrier, with increased permeability of the latter and the production of flooding and alveolar edema furthermore associated to the depletion of surfactant–thus giving rise to alveolar instability and collapse.38 Pulmonary involvement is heterogeneous, with well aerated lung regions that participate in gas exchange, and other regions that have collapsed as a result of the overpressure exerted by the interstitial edema and alveolar flooding39,40–these mechanisms explaining the decrease in lung volume in these patients.40 Pronation makes it possible to recruit these affected zones,37 redistributing and homogenizing ventilation,30 reducing the intrapulmonary shunt effect and improving oxygenation, ventilation and lung mechanics.41 However, the degree of recruitment depends on factors such as the severity of lung involvement,25 the pronation time39 and the time elapsed from lung injury to patient placement in the prone position.19
Although the prone position can effectively increase oxygenation when used several days after onset of the disease,10 its application during the early stages was found to offer betters results. During these early stages, all the conditions favoring the effectiveness of pronation are present, such as alveolar edema, reversible collapse and the absence of pulmonary structural alterations.37 In these stages, the reduction in ventilator-associated lung injury risk probably exceeds that obtained when pronation is used in later stages of ARDS, when the damage has already been caused.42 This has been clearly demonstrated in our study, where the patients placed in the prone position within the first 48h of the evolution of the disease showed a clear protective effect referred to mortality risk.
In clinical practice, the severity of ARDS has been rated according to the PaO2/FiO2 ratio,4 though in disorders as complex as this syndrome, the PaO2/FiO2 ratio depends on the PEEP level and FiO2 administered, as well as on the prescribed treatments and/or interventions, the comorbidities, and the innate compensatory mechanisms of the disease.43 Despite the presence of these variables, the results obtained allow us to clearly establish that the prone position is indicated in patients with severely impaired oxygenation, as has already been demonstrated in other studies.5,17–19,21–23 Furthermore, prolongation of the prone position to over 12 consecutive hours a day (18h on average) in patients with severe ARDS is a highly recommended strategy.11,12,14,16 It is important to note that in patients with mild ARDS, pronation has not been found to offer clinical advantages and is therefore not advised.15 In cases of moderate ARDS, the clinical recommendation is likewise not clear, though the results of the post hoc analysis of a meta-analysis9 revealed a certain tendency to benefit patients with PaO2/FiO2<140. Consequently, when taken in combination with the results of the PROSEVA study,16 these data allow us to consider the use of this strategy in this patient subgroup.37,44
Adverse eventsIn general, ventilation in the prone position is safe, and its complications are infrequent. The most common adverse effects are pressure ulcers and orotracheal tube obstruction. Accidental extubation, displacement of the orotracheal tube, the risk of pneumothorax, and venous access loss exhibited a similar distribution between the two groups. The development of ventilator-associated pneumonia (VAP) was not related to pronation, and its frequency was similar to that reported in previous reviews.45 Although the incidence of adverse events is low, we think that it is largely conditioned by treating team experience with the prone position, and the existence of guides and protocols with the indications, contraindications and safety measures to be adopted during the procedure.
ConclusionsThe prone position offers clinical benefits such as improved oxygenation, by optimizing lung recruitment and the ventilation–perfusion ratio, and probably also prevents and reduces ventilator-associated lung injury by homogenizing the stress and strain upon the lung parenchyma, resulting in a decrease in mortality risk.
Based on the results obtained, the prone position can be recommended in patients with severe hypoxemia (PaO2/FiO2<100), associated to a low tidal volume (<8ml/kg ideal weight), during a period of over 16h a day, and starting early during the course of the disease (<48h). These consequently would be the indications and associated strategies to be included in pronation protocols.
Pronation requires no special equipment, but should be carried out by trained personnel and adopting the required safety measures in order to avoid associated complications.
Financial supportThe authors declare that no financial support has been received for this study from any government or private organism.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Mora-Arteaga JA, Bernal-Ramírez OJ, Rodríguez SJ. Efecto de la ventilación mecánica en posición prona en pacientes con síndrome de dificultad respiratoria aguda. Una revisión sistemática y metanálisis. Med Intensiva. 2015;39:359–372.