The main, universal problem for transplantation is organ scarcity. The gap between offer and demand grows wider every year and causes many patients in waiting list to die. In Spain, 90% of transplants are done with organs taken from patients deceased in brain death but this has a limited potential. In order to diminish organ shortage, alternative strategies such as donations from living donors, expanded criteria donors or donation after circulatory death, have been developed. Nevertheless, these types of donors also have their limitations and so are not able to satisfy current organ demand. It is necessary to reduce family denial and to raise donation in brain death thus generalizing, among other strategies, non-therapeutic elective ventilation. As intensive care doctors, cornerstone to the national donation program, we must consolidate our commitment with society and organ transplantation. We must contribute with the values proper to our specialization and try to reach self-sufficiency by rising organ obtainment.
De forma universal, el gran problema de los trasplantes es la escasez de órganos. Cada año aumenta la separación entre oferta y demanda, provocando que muchos pacientes fallezcan en lista de espera. En España, el 90% de los trasplantes se realizan con órganos de pacientes fallecidos en muerte encefálica, pero la muerte encefálica tiene un potencial limitado. Para disminuir el déficit de órganos, se han desarrollado estrategias como el trasplante de donante vivo, donantes con criterios expandidos o la donación en asistolia. Este tipo de donantes tiene también su techo y limitaciones, no pudiendo satisfacer la demanda actual. Es necesario disminuir las negativas familiares y aumentar la donación en muerte encefálica generalizando, entre otras estrategias, la ventilación electiva-no terapéutica. Los médicos intensivistas, pieza fundamental en el programa nacional de trasplantes, debemos seguir consolidando nuestro compromiso con la sociedad y los trasplantes, aportando los valores propios de la especialidad y contribuyendo a conseguir la autosuficiencia aumentando la obtención de órganos.
In memoriam of Mr. Luis Gallardo. As homage to all organ donors and their families, who at the most difficult time in life were able to say “yes”.
Organ transplantation is the only treatment option for improving or saving the life of patients with end-stage organ failure. Despite the advances in surgery, postoperative care and immunosuppressor drugs, patients continue to die while on the waiting list because of the scarcity of organs for transplantation. Indeed, such scarcity is a worldwide problem, since the need for organs increases each year – further expanding the gap between offer and demand. Up until 1 January 2014, a total of 57,012 renal transplants, 21,576 liver transplants, .024 heart transplants, 3225 lung transplants, 1517 pancreatic transplants and 105 intestinal transplants had been performed in Spain.1
Although the donation rate in Spain remains the highest in the world, with 35.1 donations per million population (pmp) in 2013 versus 25.8pmp in the United States and 19.2pmp in the European Union, it is estimated that 8–10% of all patients in Spain die while waiting to receive a compatible organ.1 The only three sources of organs for transplantation are: brain dead (BD) organ donors, donors who have died according to circulatory criteria (non-heart beating donors), and live donors. The Spanish National Transplant Organization, in the same way as other similar international organizations, is facing the enormous challenge of achieving self-sufficiency, developing and promoting new strategies aiming to increase the number of available organs through expanded donor criteria, non-standard risk donors, live donors, or donors who have died according to circulatory criteria.2–5
Society and the national health systems are thus facing a worrisome scenario: the shortage of organs, growing waiting lists, and increased patient mortality while in wait of receiving a compatible organ. At the same time, and as an added drama, under-developed countries or countries with low donation rates suffer organ trafficking6–an unfair and ethically unacceptable practice that always benefits patients with greater economical resources.
Donors deceased according to circulatory criteria (non-heart beating donors)Donors who have died according to circulatory criteria (non-heart beating donors) are classified as follows: (1) Maastricht donor classification type II (Madrid modification)7 or uncontrolled asystolia donor: these are patients with unexpected cardiorespiratory arrest in which cardiopulmonary resuscitation maneuvering fails (unsuccessful resuscitation). If cardiac arrest occurs on an out-hospital basis, the donor is classified as corresponding to type IIa, versus type IIb when cardiac arrest occurs in hospital; (2) Maastricht donor classification type III or controlled asystolia donor: these are intubated patients subjected to mechanical ventilation in the Intensive Care Unit (ICU), in whom ventilation is suspended as part of limitation of life support (LLS). In these cases, programmed organ harvesting is carried out after cardiac arrest.
Non-heart beating donors are generally a minority among the global donors, though with important differences from one country to another.8 In the United Kingdom and the Netherlands, they account for up to 40–50% of all deceased donors, while in other countries such as Germany, Portugal or Sweden there are no such donors.9 In the year 2013, non-heart beating donors represented 8% of all worldwide donors reported to the Global Observatory on Donation and Transplantation, and 10% of the donations in Spain.7 Of the 159 non-heart beating donors in Spain in 2013, 108 (68%) were uncontrolled asystolia donors (a figure that remains stable with a slight decreasing trend), and 51 (32%) were Maastricht type III donors, which show a strong rising trend with a very low number of donors per hospital–with the exception of Puerta de Hierro Hospital in Madrid. At present 32 Spanish hospitals have introduced donations of this kind. The incorporation of non-heart beating donor programs represents an undeniable quantitative benefit, since the total donor pool is expanded as a result. A multicenter study carried out in Catalonia in 3315 patients admitted to the ICU has estimated that 7.7% of all subjects in which ventilatory support was suspended as part of the LLS protocol could have served as controlled asystolia donors.10 The European Achieving Comprehensive Coordination in Organ Donation (ACCORD) study, which analyzes end of life care and the donation potential in critical care units, has documented very important variations in LLS, since such measures are practically inexistent in some countries, while other countries have LLS rates of over 70%.11
Despite its benefits, non-heart beating donation has some limitations: (1) donors must be under 65 years of age; (2) patients who do not suffer asystolia within 60–120min after the start of LLS cannot be used as donors, since such prolonged agonal periods preclude tissue perfusion and thus make organ use unviable. The University of Wisconsin score12 assesses the probability of continued effective breathing after the suspension of ventilation, and thus allows us to predict whether the patient will suffer cardiac arrest within the time window defining acceptance as a donor. Consideration also must be made of the warm ischemia time, defined as the time from functional hypoperfusion with a mean blood pressure (MBP) of <60mmHg to the start of cold perfusion. Warm ischemia times of <30–60min are considered acceptable for liver, lung and pancreas, versus <120min for kidney–though the concrete times depend on the hospital protocol used in each case.4,13 The percentage of patients who do not suffer asystolia within the established time limit, and who therefore cannot be used as donors, is estimated to be 17–36%12,14; and (3) donors of this kind produce fewer organs. In the United Kingdom, a brain dead donor generates 3.9 organs on average, versus 2.5 organs in the case of a non-heart beating donor.15 Due to the characteristics of death, some organs such as the heart are not transplantable, though there are some exceptional cases published in the literature, and there is active research in this field.16–18 Other organs such as the liver show low tolerance of agonal hypoxia, resulting in added post-transplant complications such as ischemic cholangiopathy and poorer survival outcomes.19 Although the new preservation techniques produce a larger number of lungs, these in the best of cases are harvested in fewer than 40% of all non-heart beating donors.20 In Spain the figure is far lower, since in 2013 a total of 19 lungs were harvested from 159 non-heart beating donors (12%), and of these organs only 10 (6%) were actually transplanted.7
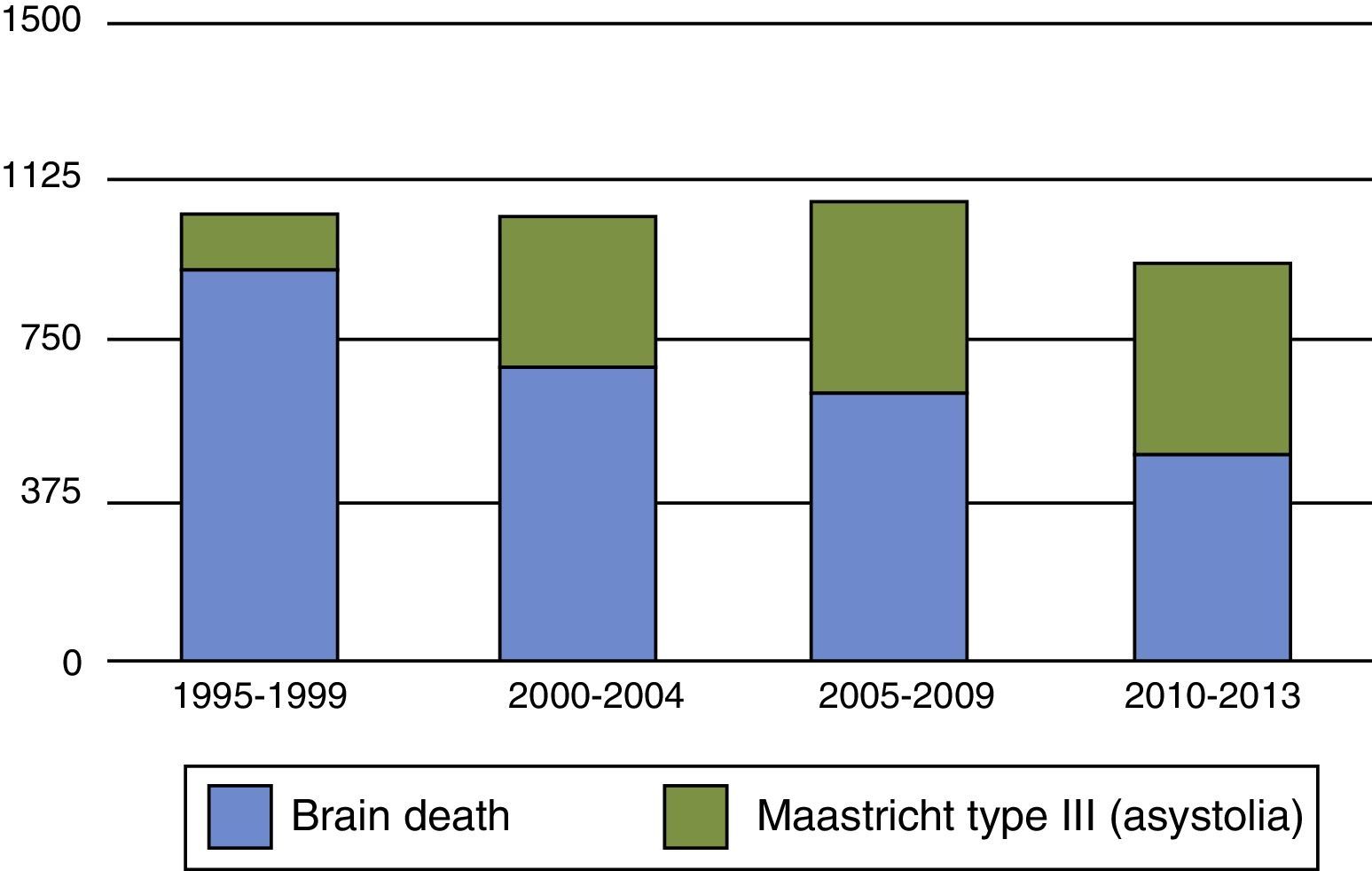
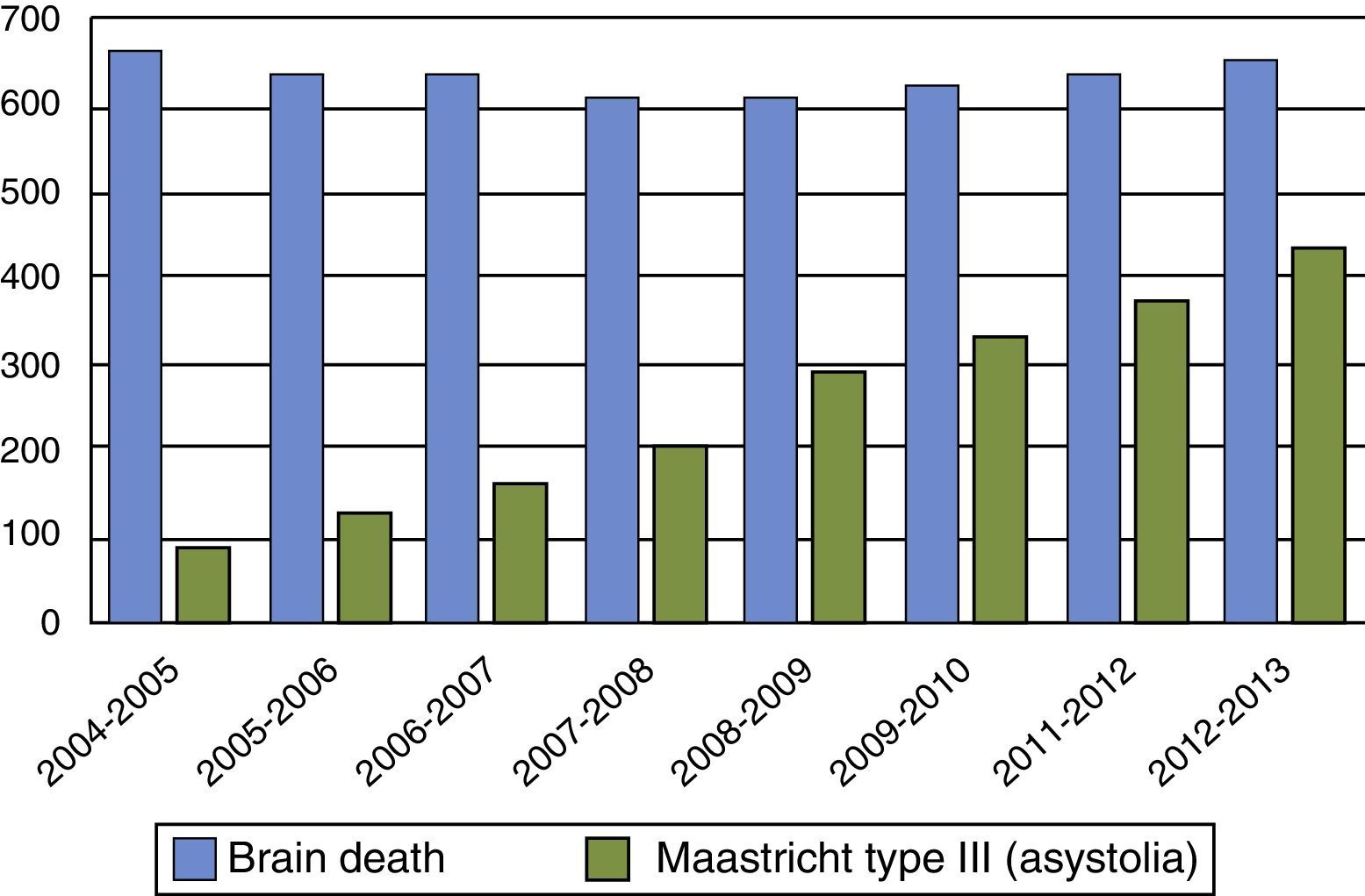
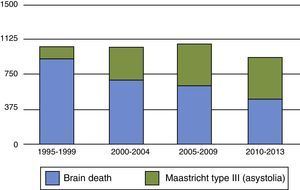
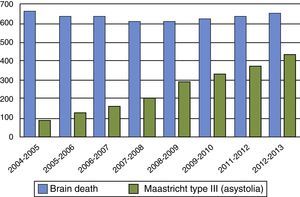
On the other hand, regarding Maastricht type III donors, there is debate as to whether their increase may have conditioned a decrease in brain dead donors, as has been observed in countries such as the United Kingdom and the Netherlands (Figs. 1 and 2).21,22 In order not to reduce total organ generation and avoid the abovementioned conditioning effect, it is essential to stress that the incorporation of Maastricht type III donor programs must seek to obtain organs “in addition to” and not “instead of” those obtained from brain dead donors. If very early LLS is adopted in patients with catastrophic brain damage, we may increase the number of non-heart beating donors but reduce the number of dead brain donors–thereby reducing the total organ pool. Health organizations are very complex structures, and the incorporation of new practices and routines may be difficult to modulate, giving rise to undesired results. We must promote and develop controlled asystolia donation, but also must make sure that this does not occur at the expense of reducing the number of dead brain donors. Delaying LLS as far as possible, with consensus on the part of the family, may be an option for increasing the number of organs. This issue will probably require an in-depth ethical debate if the gap between organ offer and demand continues to grow.
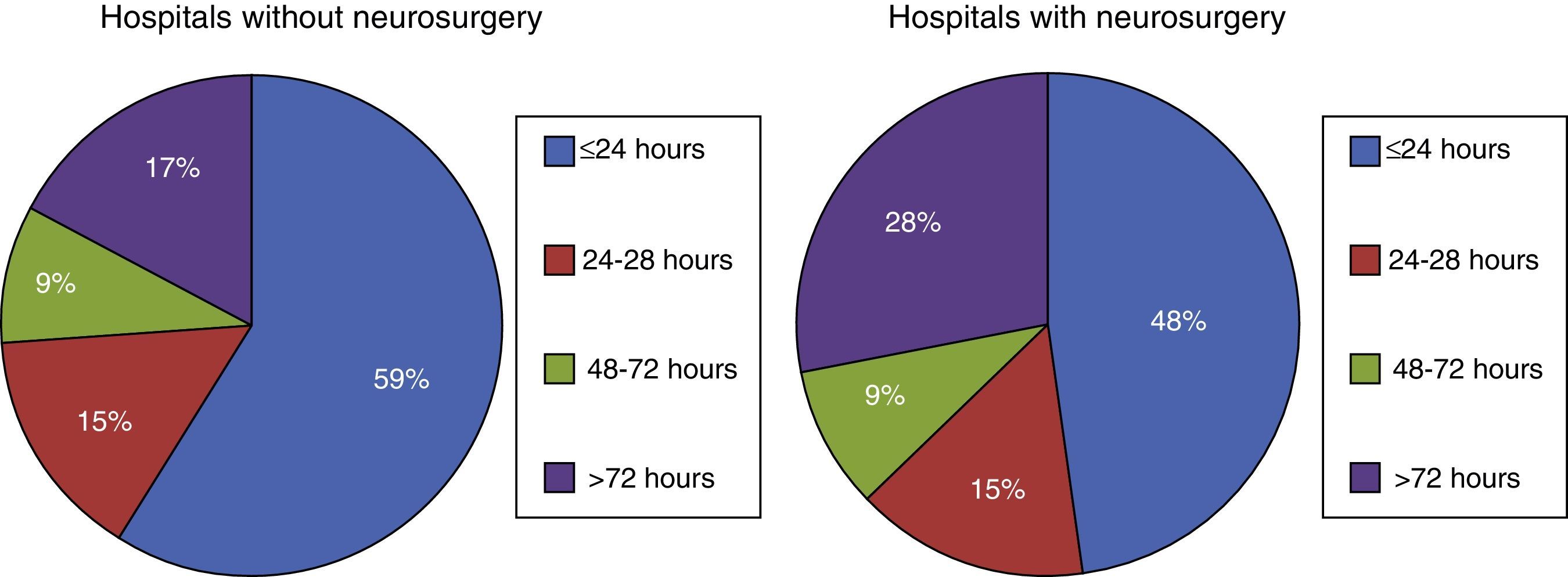
Brain death is of course an undesirable outcome in medical practice, but can have beneficial collateral effects. Donors deceased according to neurological criteria are the most common source of organs, and are therefore central to any national organ transplant program. They are regarded as ideal donors and are the only source of heart grafts. A study conducted in European ICUs, involving 4248 deceased patients, found only 330 to correspond to dead brain cases (7.8%). There are important regional differences in this regard. In the northern European countries, brain death represents 3.2% of the cases, while in southern Europe dead brain cases account for 12.4% of all deaths in the ICU.23 In Spain, brain death represents 2.3% of all in-hospital deaths and 12.4% of the deaths that occur in the ICU (8.3% in hospitals without neurosurgery and 13.4% in those with neurosurgery),24 though in ICUs with a large number of neurocritical cases the percentage corresponding to brain death can reach 33% of all fatalities.25
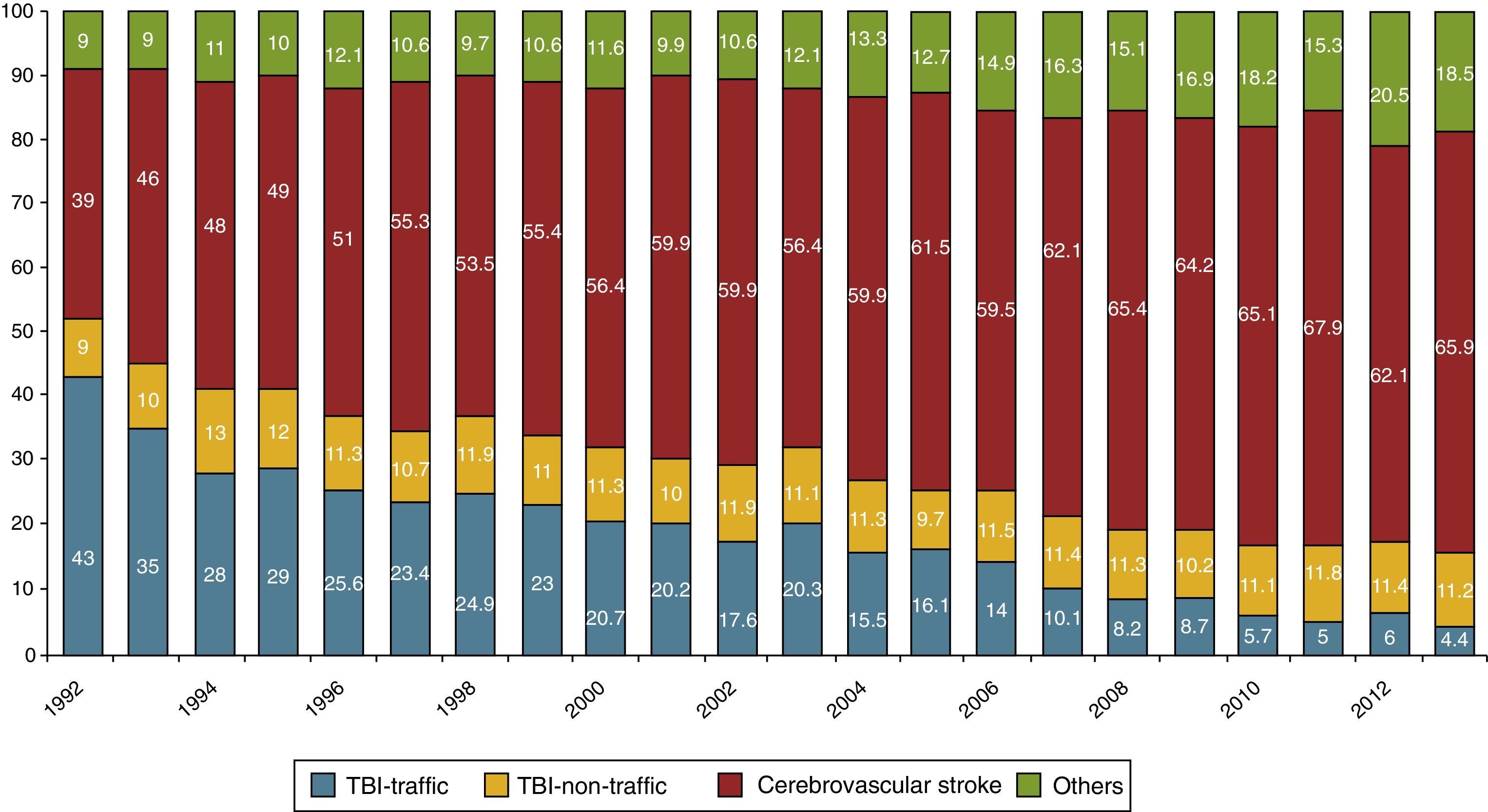
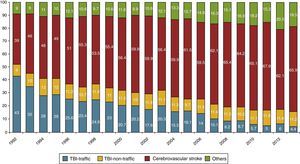
Because of its characteristics and etiology, brain death has limited potential. In recent years a decrease in brain dead donation has been observed worldwide, due to different reasons.21,26–31 One of the most important causes is the reduction in traffic accidents in most western countries, which has resulted in a significant decrease in traumatic brain injuries (TBIs). Important improvements in vehicle safety and roads, prevention campaigns, and strict regulation of traffic safety explain the decrease in traffic accidents in both North America and Europe. In effect, in the year 2009, the United States recorded its lowest number of traffic accident deaths since 1954.29 In Spain, traffic accidents caused 1680 fatalities in 2013, with a mortality rate per million inhabitants of 36, which is far below the European average of 52. This classifies Spain as the country with the fifth lowest number of traffic accident deaths in the European Union.32 As a result of the above, TBI-traffic accident donors have decreased from 43% of the total in 1992 to only 4.4% in 2013 (Fig. 3).33 In relation to this observation (among others), the mean adult donor age has increased from 38 years in 1992 to 60.7 years in 2013.34 On the other hand, as a result of improved general neurocritical patient care, a global decrease in brain dead donation of non-traumatic origin has also been observed. One of the underlying causes is the better and earlier management of subarachnoid bleeding, due to a greater availability of endovascular treatment.35
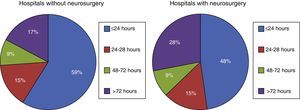
In Spain, the leading cause of brain death in donors is intracerebral hemorrhage (42%), followed by TBI (19%)–fundamentally in relation to “non-traffic TBI” (11.5%)–and subarachnoid bleeding (14%).36 A Spanish multicenter study of 1844 brain death patients admitted to the ICU found that patients who evolve toward brain death do so very early: 59% of the patients died in the first 24h of admission to hospitals without neurosurgery, versus 48% in those with neurosurgery (Fig 4).36 The decrease in brain death is also seen in Spain, where the donors deceased according to neurological criteria dropped from 32pmp in 2001 to 29.2pmp in 2010.24 In this country, approximately 90% of all transplanted organs come from dead brain donors34; as a result, the decrease in number of brain deaths will limit the availability of organs for transplantation, particularly heart grafts.
Neurocritical patients with catastrophic injuries, subjected to extensive decompressing craniectomy, sometimes do not evolve toward brain death and remain in a vegetative state or die as a result of secondary complications. In such cases decompressive craniectomy may be a futile measure, preventing natural evolution toward brain death. New approaches to LLS have been suggested in order to avoid this situation and the associated decrease in number of brain dead donors, such as cranioplasty with bandaging, which has been regarded as an ethically acceptable form of LLS similar to other commonly used procedures. In cases of irreversible brain damage in which LLS involving cranioplasty with bandaging is decided, we must know the prior instructions of the patient, and if this is not possible, we must obtain permission from the family after providing detailed information on the procedure.37 However, while these measures can rescue a considerable number of donors each year, their impact is limited and their use has not become generalized.
Despite the observed tendency toward fewer brain death cases, this situation must be analyzed in full, since there is a very high growth potential for donors defined according to neurological criteria–as has been evidenced in some Spanish autonomous Communities with brain dead donor rates of over 55pmp versus others in which the figure does not exceed 25pmp.33 One of the differences in the epidemiology of brain death is that its leading cause in Spain is intracerebral hemorrhage36 versus subarachnoid bleeding in other countries.22 Intracerebral hemorrhage is of a vascular origin and is associated to population aging factors such as arteriosclerosis or hypertension. Consequently, it has an important growth potential as a source of organ donors.
Organ donation and end of life care. Ethical considerationsOrgan donation is a right that forms part of our living will, and therefore should be considered within the end of life care setting.38 It is necessary to examine the last will records or ask the family about the opinion of the deceased person, respecting the principle of patient autonomy and proactively contributing to fulfill his or her wishes regarding the donation of organs for other people. This will allow posthumous application of the will of the patient, ennobling the individual, and contributing added value to death.
Organ donation is not only a task of the transplant coordinator: it should implicate all intensivists and health professionals, since it respects the principle of autonomy, promotes values such as generosity and solidarity, constitutes a treatment with excellent clinical outcomes, and is moreover very efficient in terms of resource utilization. Organ donation is good for patients and good for the healthcare system, since it is a cost-effective procedure. Some authors have estimated that a single multiorgan donation of 6 organs can generate up to 55.8 life years for the recipients of such organs.39 The World Health Organization (WHO),40 the Medical Ethics and Deontology Code of the Spanish National Medical Organization,41 and the Ethical Code of the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias, SEMICYUC) consider it an obligation of all health professionals to promote organ donation,42 based on the patient needs and good clinical outcomes.
Elective–non-therapeutic ventilationIn 1990, the Royal Devon and Exeter Hospital in the United Kingdom was the first center to publish a protocol referred to the intensive care admission of patients at risk of imminent death due to catastrophic brain damage, with the exclusive purpose of organ donation.43 These patients were subjected to tracheal intubation, mechanical ventilation and general supportive measures until organ harvesting. This is what is known as elective-non-therapeutic ventilation. The authors concluded that this strategy could significantly increase the donor rate of 14.6 donors pmp found at that time in the country. Although the idea initially generated controversy,44 subsequent debate, reflections and conclusions upon the subject have evolved favorably (provided there is no prior patient wish against the initiative), and many bioethical studies support elective-non-therapeutic ventilation at both international level and in Spain.45–51
The ethical arguments in favor are clear, and admission to an ICU with mechanical ventilation does not violate the principle of beneficence. In a study on the subject, de Lora and Pérez-Blanco45 considered that admission to an ICU is intrinsically good, since the ICU is the best place for assessing the patient condition and affording the best medical care. In effect, the ICU offers the greatest guarantees of optimum care, including end of life care. The authors underscored that the systems inherent to the ICU include bispectral index scale (BIS) monitoring, which ensures optimum sedation, and that elective ventilation may be considered a good thing, since it can facilitate death with dignity and the absence of pain. The will of patients who have previously expressed their wish not to be intubated or admitted to an ICU must be strictly observed. However, in the absence of prior instructions, admission to the ICU may be ethically justified. The principle of non-maleficence is also observed, since if the patient does not evolve toward brain death within a time period agreed with the family (usually ≤72h), the medical team would suspend all life support measures in order to avoid a vegetative state. The principle of fairness also would be supported by the fact that organ donation contributes to give life or improve quality of life. Moreover, patients of this kind quickly evolve toward brain death with scant resource utilization–this being an important consideration for the responsible management of available resources. In cases of elective ventilation and admission to the ICU of a potential organ donor, a prior interview is needed to truthfully inform the family about the clinical situation, and to ask whether there are any prior instructions either in favor or against organ donation. In clinical practice there may be a state of psychological block or emotional shock in the first few hours after admission preventing the family from adequately assimilating the information. In such cases the matter may be dealt with on a delayed basis, offering the family a minimum period to adapt to their personal tragedy. Once the family is able to make adequately reasoned decisions, the steps to be taken should be examined–assessing possible maintenance in wait of brain death, or organ and/or tissue donation under conditions of asystolia if the family is considering immediate LLS.
In the year 2003, with the approval of the Care Ethics Committee, Gregorio Marañón Hospital in Madrid became a pioneer in this field, with protocolization of the admission of patients to the ICU with the purpose of serving as organ donors. This activity represented 30% of all its donors in the period 2003–2005, with a mean time between admission to the ICU and brain death of 15h (range 2–24) (Braulio de la Calle, non-published observations). In other centers such as Virgen de las Nieves Hospital in Granada, admission to the ICU for this same purpose now accounts for 11% of all the donors in that center (José M. Pérez-Villares, non-published observations).
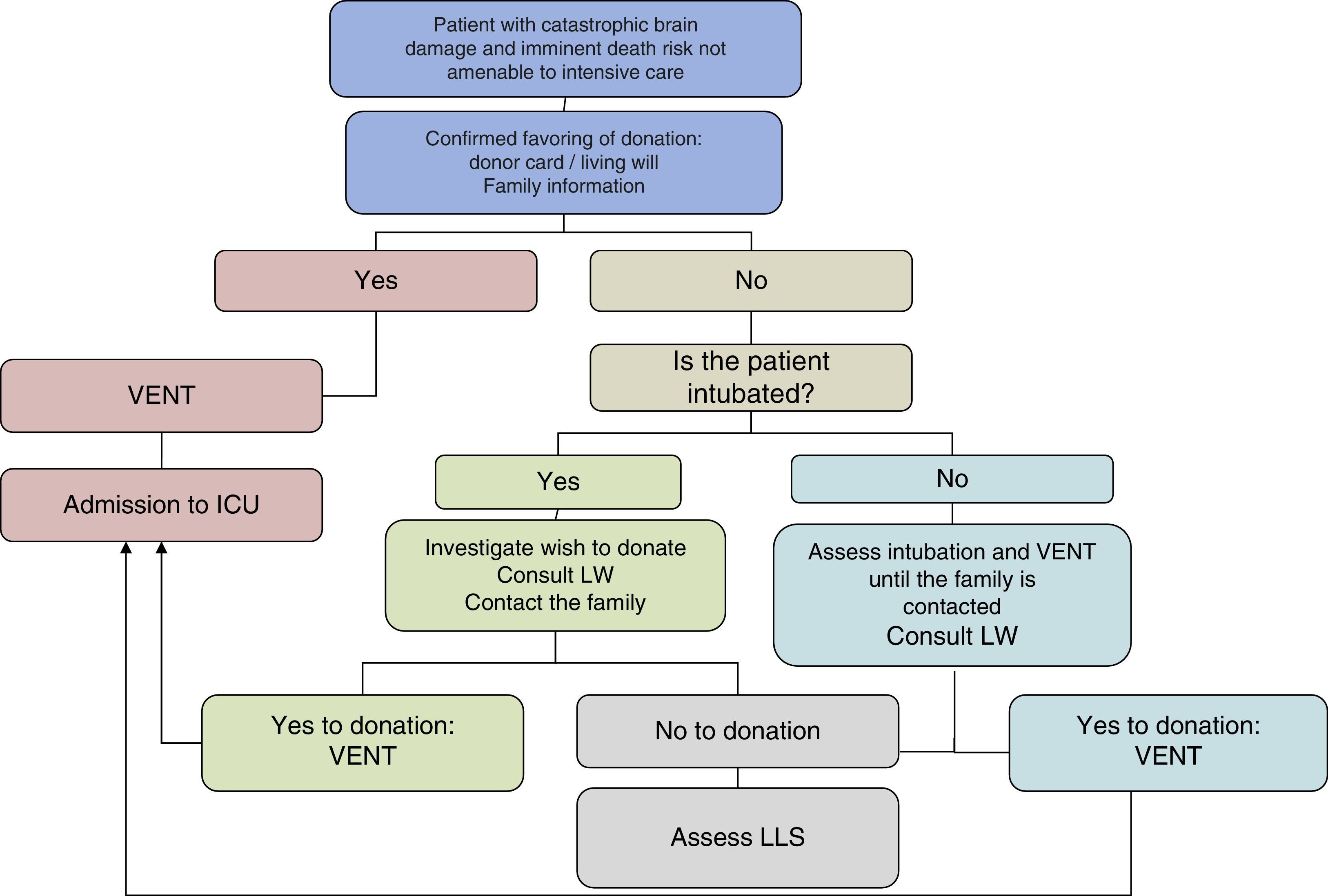
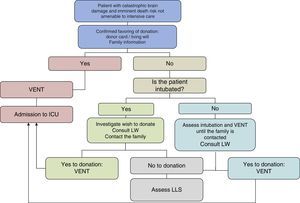
The main sources of potential donors according to neurological criteria are the Departments of Emergency Care, Neurology and Neurosurgery. In this context, elective-non-therapeutic ventilation protocols would have to be implemented and generalized. The strategy of admitting patients to intensive care for organ donation based on the prior interview and elective-non-therapeutic ventilation would allow a very notorious increase in the number of organs obtained from brain dead patients. Many of the patients reaching the emergency room have already been intubated by the out-hospital emergency service. It is therefore not always necessary to urgently decide the start of elective ventilation–a fact that facilitates decision making and clinical intervention until the express wish of the patient and/or family becomes known (Fig. 5).
As physicians, we also must take purely emotional aspects into account. In this regard, families that have suffered the tragedy of a death and have agreed to organ donation may find emotional relief in knowing that they are making a gift of life to others who are in need.
On the other hand, surgeons and clinicians working in the field of organ transplantation are fully aware of the imperious need for organs in order to improve patient health, and have first hand knowledge of the suffering experienced by patients on the waiting list. They are consequently leading role players and must become actively involved in the donation process. The clinical characteristics of current donors referred to age, expanded criteria or non-standard risk donation, which in the year 2013 accounted for 5.4% of all deceased donors (Beatriz Mahillo, non-published observations), are not those of an “ideal donor”–a fact that often generates some rejection on the part of the transplant teams. In this respect, in the course of 2013, a total of 1132 solid organs were rejected for transplantation.33 This circumstance deserves profound reflection in the light of the existing shortage of organs. As we have seen, the prevalence, etiology and characteristics of the donors have changed, and this trend can be expected to continue in the coming years. We therefore have to work with these organs. This in effect is the great challenge facing transplantation: to continue to achieve the best outcomes with the organs that are available. Effort therefore must be intensified to optimize those factors which exert a positive influence upon favorable graft progression, such as shortened cold ischemia times, improved organ preservation with the use of ex vivo perfusion systems, and improvement in surgical times and techniques.
Although there is a presumed consent law in Spain, explicitly stating that organ harvesting from deceased individuals can be made for therapeutic or scientific purposes provided there are no express prior instructions against donation,52 this regulation is not put into practice, and the Spanish National Transplant Organization and Transplant Coordination Boards of the different Autonomous Communities have established policies that are maximally respectful of the different social sensitivities. If the express wish of the deceased person is not known, the national system continues to consider the obtainment of family consent an obligate condition–a fact that has contributed to make Spanish donation programs known for their guarantees and rigor. Family rejection of donation has decreased in recent years, from 27.6% in 1992 to 15.9% in 2013. Despite the significant decrease in rejections, these figures represent an important loss of donors (1606 in the period 2009–2013).33 We therefore have to continue our efforts to make society aware of the need for donation and of the values it represents.
Intensive care medicine and organ donationIn Spain, 85% of all transplant coordinators are intensivists.53 The ICU is central to organ donation, and in most cases intensivists are collaborators and/or are directly responsible for identifying potential donors, diagnosing brain death and Maastricht type II and III donation in asystolia, and for maintaining the multiorgan donor. In some hospitals they are also in charge of the postoperative care of transplant recipients. The first course in transplantation and donation in intensive care for residents in training was imparted in the year 2006, on the initiative of the Andalusian Autonomous Community transplant coordinator, Dr. Manuel Alonso, and with support of the project by Dr. Rafael Matesanz, Director of the Spanish National Transplant Organization, which supplied the necessary funding. Since then, and with the scientific backing of the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias, SEMICYUC), four courses a year are organized throughout Spain, with the training of at least 120 residents a year. Furthermore, other many specific training courses in the field have been organized for over 20 years. The offer in training courses in donation, donor management and transplant coordination is extensive and is well considered.54 The transplant coordinators, along with the rest of the intensivists, form a team network that intervenes in the entire organ donation process, contributing to place Spain at the top of the list of organ donations in the world. This active and direct participation of our specialists and of the ICU (the place where donors are found) is partially responsible for the internationally acknowledged success of the so-called Spanish model.
ConclusionsThe imbalance between the offer and demand for organs for transplantation is a dramatic situation affecting society as a whole. Further efforts are needed to promote donation and reduce family rejection–enhancing global awareness of the scarcity of organs. From the technical perspective, new frontiers must be explored in order to maintain a degree of self-sufficiency, such as the acceptance of new donation criteria, continued support of live donor transplants, increased donation in asystolia, and the generalization of practices such as elective–non-therapeutic ventilation, with a view to increasing dead brain donation. All these interventions are to be fundamented on gratitude to the donors and their families, and to the entire healthcare system, for the efforts made in the obtainment of organs.
As intensivists, we must consolidate our commitment to transplantation and society, contributing the values inherent to our specialty and working to increase organ donation. The scarcity of organs for transplantation has a high cost in terms or mortality and quality of life for many patients. We therefore have an undeniable ethical and professional duty in this field.
Financial supportThe authors have received no financial support for the conduction of this study.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Thanks are due to Jimena Escudero, of the Department of Anglo-German and French Philology (University of Oviedo) for translation of part of the manuscript.
Please cite this article as: Escudero D, Otero J. Medicina intensiva y donación de órganos. ¿Explorando las últimas fronteras? Med Intensiva. 2015;39:373–381.