Delirium is a very common brain functional disorder in patients admitted to the Pediatric Intensive Care Unit (PICU), with a reported prevalence of 11–44%.1–4 The occurrence of delirium in the PICU is associated to negative outcomes such as prolonged PICU stay, increased hospitalization costs, and greater morbidity and mortality.4–6 Different studies have found that infants aged two years or younger are at a higher risk of developing delirium.5,7,8 These observations support the need for validated instruments capable of detecting delirium.
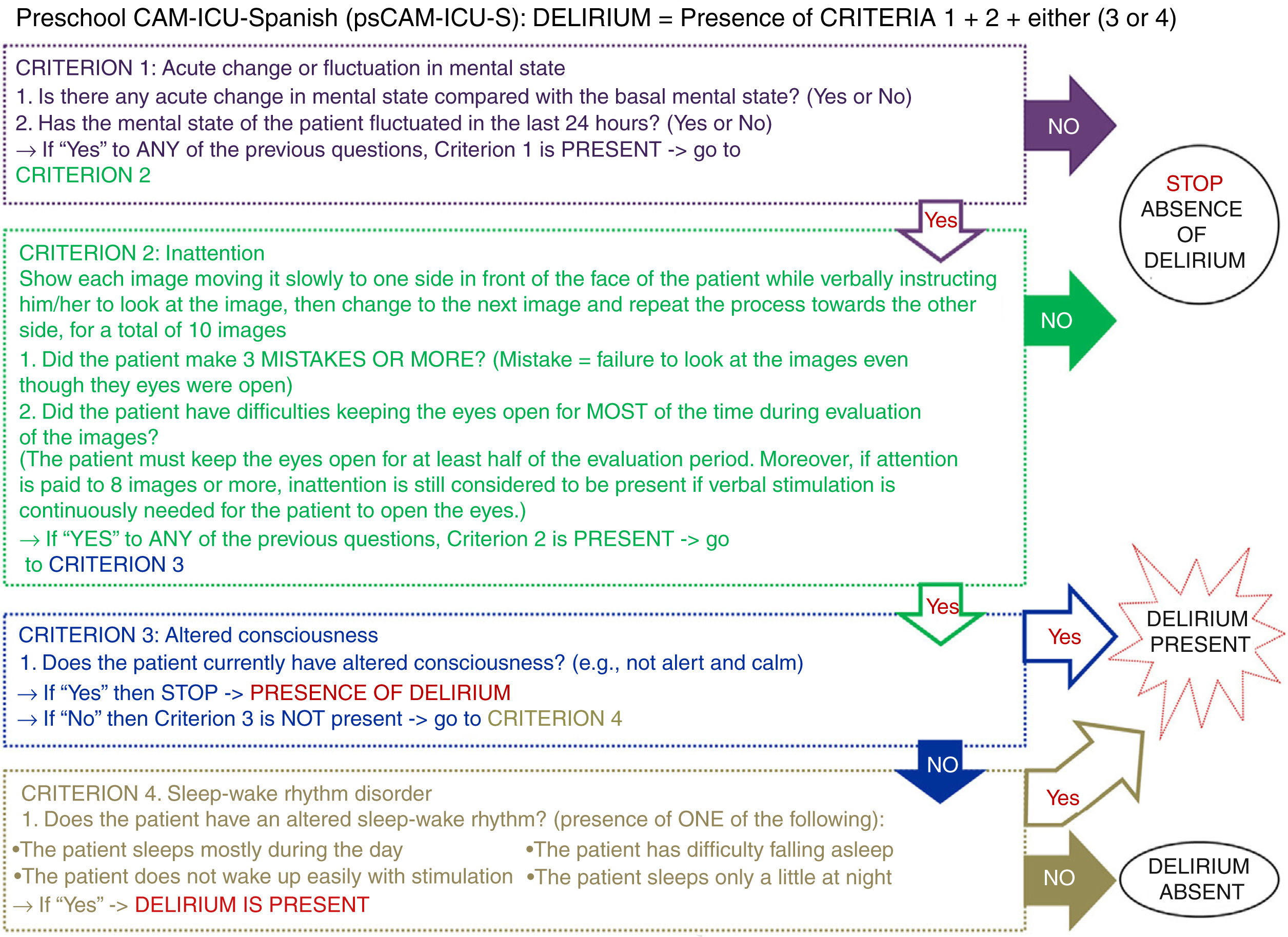
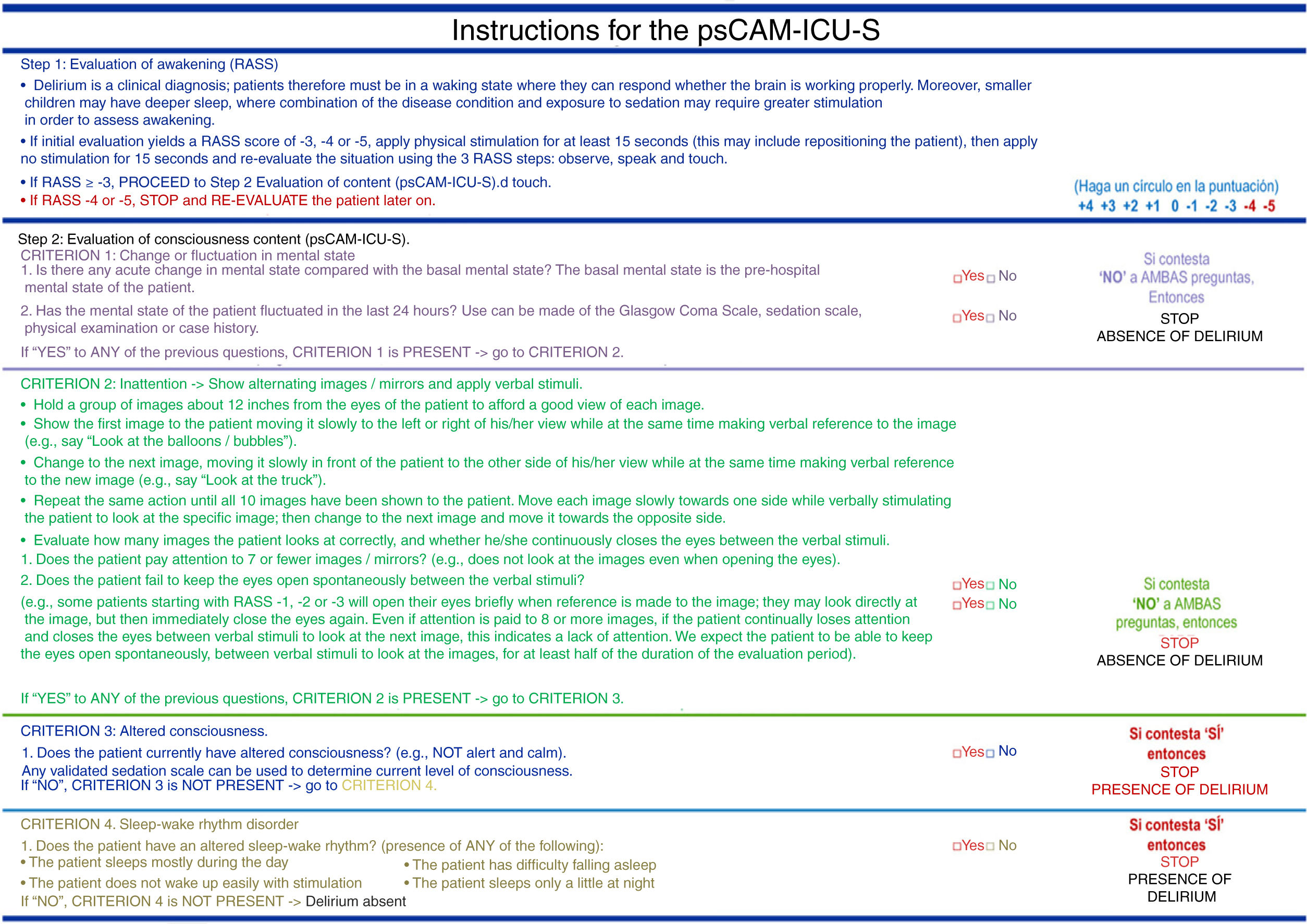
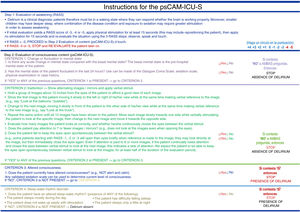
The Preschool Confusion Assessment Method for the Intensive Care Unit (psCAM-ICU) was designed based on the criteria of the pCAM-ICU (patients between 5–19 years of age) and CAM-ICU (adults), which are validated and reliable instruments widely used to assess the presence of delirium.2,9 The psCAM-ICU evaluates the four key manifestations of delirium, based on the Diagnostic and Statistical Manual of Mental Disorders – Fifth Edition (DSM-5), namely: acute change or fluctuation in mental state (1st criterion), inattention (2nd criterion), altered consciousness (3rd criterion) and disorganized brain (4th criterion). The evaluation of delirium involves two main steps: assessment of awakening using the Richmond Agitation – Sedation Scale (RASS) and the evaluation of consciousness content using the psCAM-ICU.
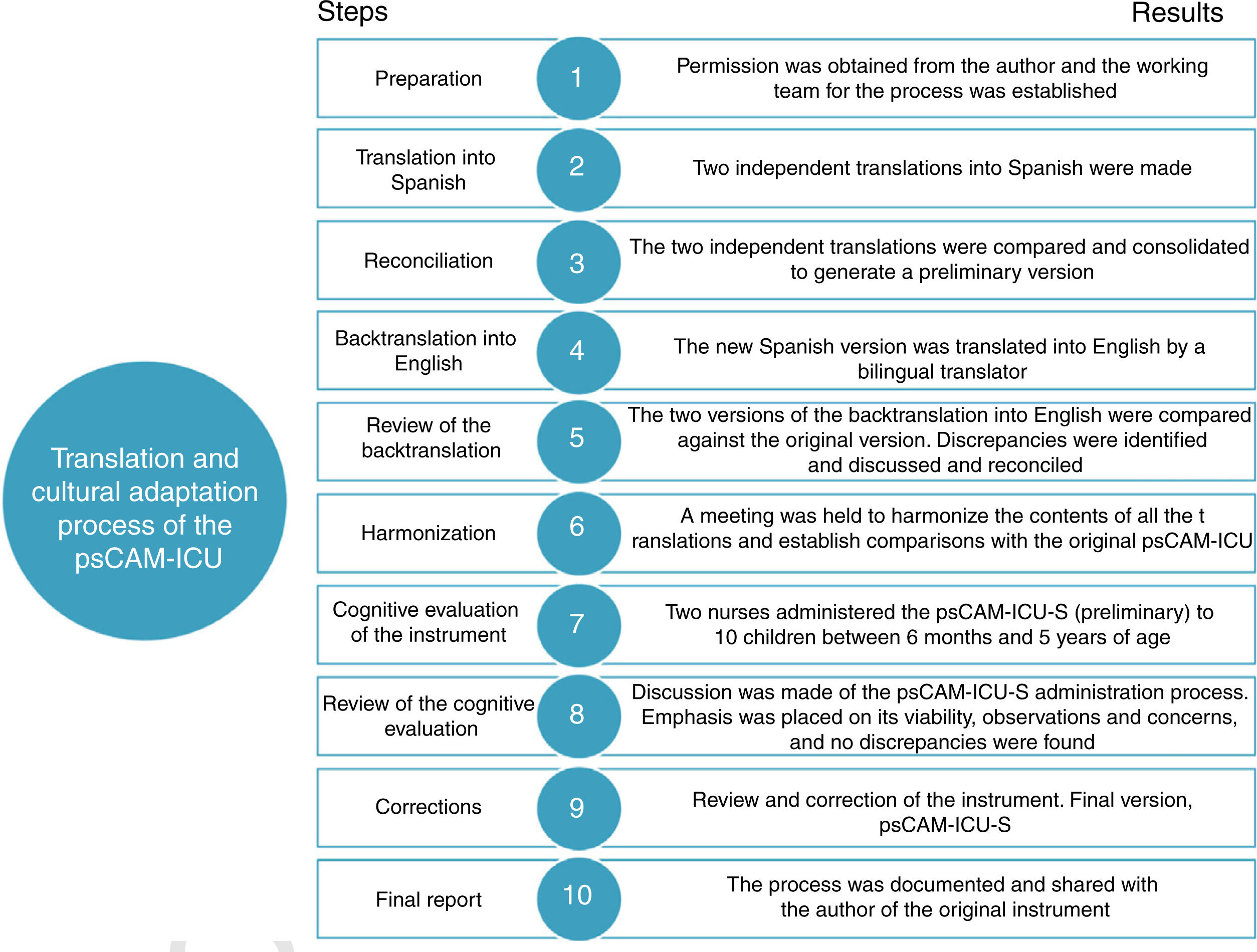
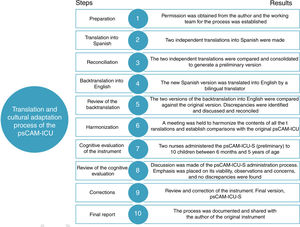
The translation and cultural adaptation of the psCAM-ICU was carried out using the 10 steps of the Principles of Good Practice (PGP) for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes Measures.10 Step 1 (Preparation) involves the obtainment of authorization from the author of the original instrument and configuration of the working team. Dr. Heidi Smith agreed and participated as consultant throughout the process. The team comprised two research nurses, a certified translator (Spanish as mother tongue), three bilingual translators (English and Spanish) with prior experience in the translation of health-related instruments, two research assistants, a pediatric intensivist and a pediatric intensive care nurse. One of the translators acted as coordinator of the project.
In step 2 (Translation into Spanish), the certified translator and another translator carried out independent translations of the psCAM-ICU. In step 3 (Reconciliation), a panel composed of one of the research nurses, a translator and the project coordinator compared both Spanish translations and found them to be similar. However, a discrepancy was observed between the title of the fourth criterion (disorganized brain) and the questions that evaluate this criterion. This had also been reported by Matsuishi et al.11 in the translation of the psCAM-ICU into Japanese. The mentioned criterion refers to disorganization of thought or function, which in infants and preschool children manifests with alteration of the sleep-wake rhythm, inconsolability and/or a lack of recognition of the environment or parents / caregivers.2 At the time of development of the original instrument, these three components described the fourth criterion (disorganized brain); however, following a component sensitivity and specificity analysis, two of the components were eliminated, leaving only alteration of the sleep-wake rhythm for clinical evaluation. Since the term “disorganized brain” is confusing and this criterion only evaluates alteration of the sleep-wake rhythm, the research team in consultation with the author of the original instrument determined that the most adequate title for the fourth criterion would be “sleep-wake rhythm disorder”. Following consensus regarding the content, a preliminary version of the instrument in Spanish was developed.
Steps 4 and 5 (Backtranslation into English and Review of the backtranslation) involved the participation of two translators that had not taken part in the previous steps. Two versions of the preliminary version in Spanish translated into English were produced and then compared against the original version of the instrument (in English) by the project coordinator. Both translations were seen to be similar to the original version. In step 6 (Harmonization), a comparison table was developed, including information on the original instrument, the backtranslation version and explanations to justify the discrepancies found or the changes made. The mentioned table was shared and discussed with Dr. Smith, the author of the original psCAM-ICU.
Step 7 (Cognitive evaluation of the instrument) suggests administration of the translated instrument to a group of participants belonging to the population of interest in order to identify comprehension problems. For this purpose, two assistant research nurses administered the psCAM-ICU (preliminary version in Spanish) to 10 children between 6 months and 5 years of age. The instructions and questions were easily understood by the children. In step 8 (Review of cognitive evaluation of the instrument), the nurses, a translator and one of the research nurses met to discuss the findings of application of the psCAM-ICU. Furthermore, one of the research nurses met with the pediatric intensivist and pediatric intensive care nurse to assess semantic, conceptual and experience equivalences. This allowed evaluation of the clarity of words or phrases, the quality of writing, and its pertinence to Puerto Rican culture.
Step 9 (Correction of the new version in Spanish) was carried out to check the presence of errors, and the final version in Spanish was completed (psCAM-ICU-S), along with the instructions for applying the instrument (Figs. 1 and 2). These can be accessed at https://www.icudelirium.org/. Lastly, step 10 (Final report) involved the preparation of a final report that was shared with the author of the original instrument (Fig. 3).
We have adapted the psCAM-ICU-S in its cultural and linguistic domains for Spanish-speaking caregivers and patients between 6 months and 5 years of age. Incorporation of this instrument to the clinical scenario will contribute to future studies and to the identification of reliable results referred to delirium.
FundingThe authors declare that no funding was received for carrying out this work.
Thanks are due to the nursing staff of the Intensive Care Unit of the University Pediatric Hospital of Puerto Rico, and to Prof. Gladys Vélez and Dr. Elizabeth Román as translators.
Please cite this article as: Figueroa-Ramosa MI, Arroyo-Novoa CM, García-DeJesús RL, Sepúlveda-Santiago CS, Solís-Báez SS, Ely EW, et al. Traducción y adaptación cultural al español del Preschool Confusion Assessment Method for the Intensive Care Unit. Med Intensiva. 2020;44:453–456.