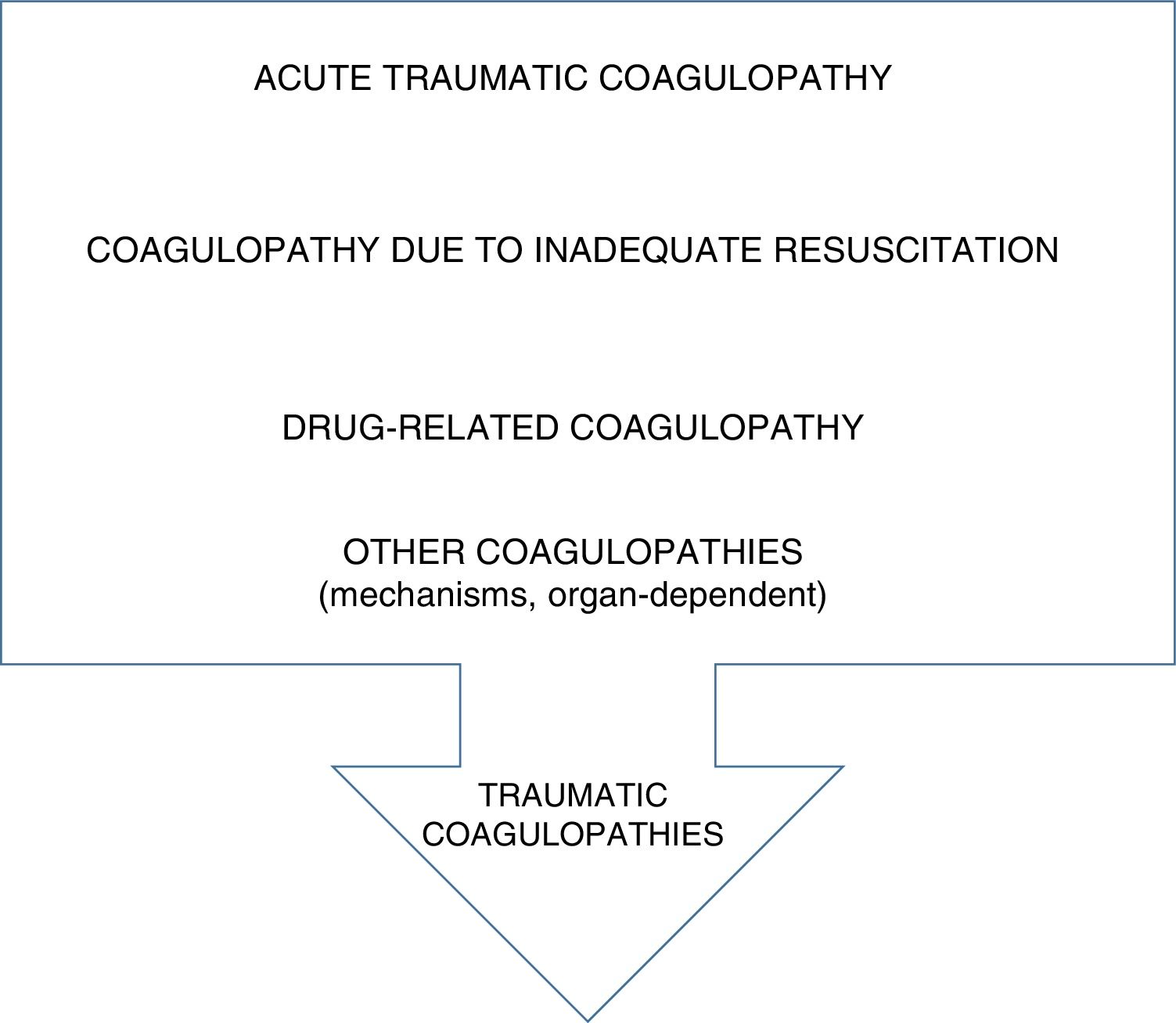
With the beginning of the century, knowledge on traumatic coagulopathy changed dramatically. The finding made by two different groups that one fourth of the patients with severe trauma showed coagulation dysfunctions at admission without any other of the factors traditionally associated with coagulopathy changed resuscitation strategies and the pathophysiological knowledge associated with hemorrhages and traumatic coagulopathy.1,2 The importance of this change impacted different aspects: first, it impacted traumatic disease significantly; secondly, it impacted the correlation between hemorrhage and coagulopathy as avoidable cause of mortality; and thirdly, this new type of coagulopathy was involved in all trauma endpoints (mortality, hospital stays, multi organ failure, etc.).3 Our mindset changed completely, and the management of coagulopathy improved with this finding as Fig. 1 shows.
TodayAcute traumatic coagulopathy, as it was first called, now called trauma-induced coagulopathy is defined as an endogenous state of hypercoagulability probably induced by a maladaptive response to hypoperfusion and mediated by several associated mechanisms (reduced thrombin generation, fibrinogen consumption and depletion, activated C protein, release of tissue plasminogen activator, presence of an imbalance in the fibrinolytic system, endothelial damage, and platelet energetic failure).4,5 Particularly, the study of the fibrinolytic system in trauma is especially relevant here. Associated with this system and one antifibrinolytic agent (tranexamic acid), the first controlled study with significant results in the management of traumatic disease (CRASH-2) has been conducted. The possibility that tranexamic acid has beneficial effects beyond the effects known so far is one of the most promising lines of research in the management of traumatic disease.6,7
This concept of primary, endogenous coagulopathy is sometimes associated with inadequate resuscitation strategies, the consumption of coagulation factors, the prior use of antiaggregant or anticoagulant drugs (less and less common) or other coagulopathy alterations involved in the lesional mechanisms (blast, penetrating, etc.) or organ-specific (central nervous system, lung) in the configuration of the patient's clinical scenario with a severe traumatic hemorrhage.8,9
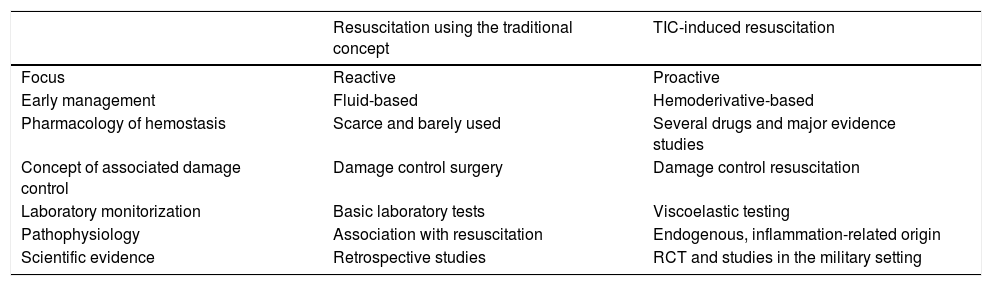
Following in the footsteps of this knowledge, the resuscitation strategy for the management of traumatic hemorrhagic shock has changed as Table 1 shows, and such a change is characterized by:
- •
More proactive approach based on hemostatic resuscitation (earlier use of hemoderivatives) in a high and balanced ratio (balanced correlation between RBC concentrates, fresh-frozen plasma products, and platelets).10
- •
Displacement of hemorrhage management therapies and correction of coagulopathy at the earliest stage of care (pre-hospital and early care stage).
- •
Expansion of damage control strategies (radiology, resuscitation, surgery) without making it very clear how these strategies impact or coexist with one another (a better physiological reserve induced by a more adequate resuscitation strategy may reduce the need for damage control).
- •
Development of predictive coagulopathy scores and activation of massive blood transfusion protocols.
- •
Individual approach using point-of-care devices to the coagulation phenomenon by studying the agents involved (complete blood count, platelets, endothelium, etc.).
- •
First controlled-studies of procoagulant therapies (factor vii, tranexamic acid, different blood components, coagulation factors, other drugs).
- •
Extrapolation of the knowledge acquired from the military experiences of specific logistic characteristics to the civilian population.8–10
Changes in resuscitation with the new concept of coagulopathy.
| Resuscitation using the traditional concept | TIC-induced resuscitation | |
|---|---|---|
| Focus | Reactive | Proactive |
| Early management | Fluid-based | Hemoderivative-based |
| Pharmacology of hemostasis | Scarce and barely used | Several drugs and major evidence studies |
| Concept of associated damage control | Damage control surgery | Damage control resuscitation |
| Laboratory monitorization | Basic laboratory tests | Viscoelastic testing |
| Pathophysiology | Association with resuscitation | Endogenous, inflammation-related origin |
| Scientific evidence | Retrospective studies | RCT and studies in the military setting |
RCT, randomized controlled trials; TIC, trauma-induced coagulopathy.
Based on the actual state of knowledge, the future will probably bring us more accurate definitions of the concepts of coagulopathy from the laboratory standpoint which, in turn, will allow individual approaches specific for each patient and disease progression. The validation of the different laboratory methods and their generalization to different economic settings and levels of healthcare is something that we will probably be a matter of future discussion.11
Another aspect that has been partially developed today but that will probably be evolved in the years ahead is the early prediction of coagulopathy to activate the logistics of a proactive management of this disease. The actual medical literature available is methodologically poor and inaccurate due to the existence of survival bias after excluding dead patients and those who require immediate surgical or invasive hemostasis. The medical literature includes up to 35 determined predictive variables and the most valid ones from the predictive point of view are consistent with the empirical recommendations established by the clinical guidelines for the management of traumatic hemorrhages (lesional mechanism, systolic arterial blood pressure, hemoglobin, lactate, INR, and FAST).11–13
Experience in the management of coagulopathy and traumatic hemorrhagic shock will probably penetrate other fields of expertise with different considerations (GI, intraoperative, obstetric hemorrhages, etc.).
We will have to study the consequences as thrombotic phenomena derived from using procoagulant therapies in this type of high thromboembolic risk process.
We will probably see advances made in the possibilities of modulating the adaptive response of coagulation and its association with inflammatory response until achieving a somehow precision medicine for the management of this disease.
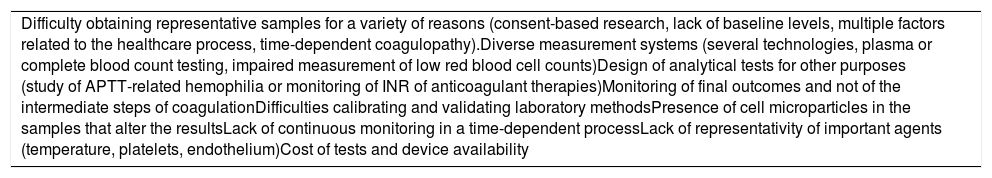
Another challenge for the future will be solving the great difficulties involved when studying these entities (shown on Table 2) that, at times, foster contradictory theories on trauma-induced coagulopathy.
Difficulties studying the coagulopathy of traumatic disease.
| Difficulty obtaining representative samples for a variety of reasons (consent-based research, lack of baseline levels, multiple factors related to the healthcare process, time-dependent coagulopathy).Diverse measurement systems (several technologies, plasma or complete blood count testing, impaired measurement of low red blood cell counts)Design of analytical tests for other purposes (study of APTT-related hemophilia or monitoring of INR of anticoagulant therapies)Monitoring of final outcomes and not of the intermediate steps of coagulationDifficulties calibrating and validating laboratory methodsPresence of cell microparticles in the samples that alter the resultsLack of continuous monitoring in a time-dependent processLack of representativity of important agents (temperature, platelets, endothelium)Cost of tests and device availability |
APTT, activated partial thromboplastin time; INR, international normalized ratio.
The study of the actual management of trauma-induced coagulopathy shows that we still have a long road ahead of ourselves when it comes to improving the storage and logistics involved in the administration of hemoderivatives. Also, together with the need for developing healthcare protocols for multiple victims, we will also have to make an estimate of the actual needs for hemoderivatives under these circumstances.12
In sum, we could say that understanding the mechanisms or coagulopathies involved in trauma is very important if we want to reduce traumatic disease-related mortality. Although it may seem obvious, we should emphasize that this was not always the case. After describing a type of alteration of traumatic coagulopathy with multiple mechanisms, we have different approaches available (viscoelastic testing, aggregometry, etc.) for the quantitative and qualitative characterization of such alterations and the different methods of treatment available. The integration of all this knowledge poses a major challenge that we will have to face in the years to come.
Conflicts of interestThe authors declared no conflicts of interest whatsoever.
Please cite this article as: Chico Fernández M, Mudarra Reche C. Las coagulopatías del trauma. Med Intensiva. 2019;43:497–499.