Cerebral venous thrombosis (CVT) is an infrequent condition that poses a diagnostic and therapeutic challenge due to its highly variable presentation and the lack of clear consensus regarding patient management. The underlying etiology, clinical condition of the patient and resources available in the hospital require an individualized treatment strategy. We present two clinical cases in which CVT, being one same disease, resulted in two different management approaches.
The first case corresponded to a hypertensive 35-year-old male who reported to the emergency service due to headache and vomiting. Brain computed tomography (CT) and angioCT revealed a right frontal intraparenchymal hematoma, right subarachnoid hemorrhage, and thrombosis of the sigmoid sinus, right transverse sinus and middle third of the superior longitudinal sinus.
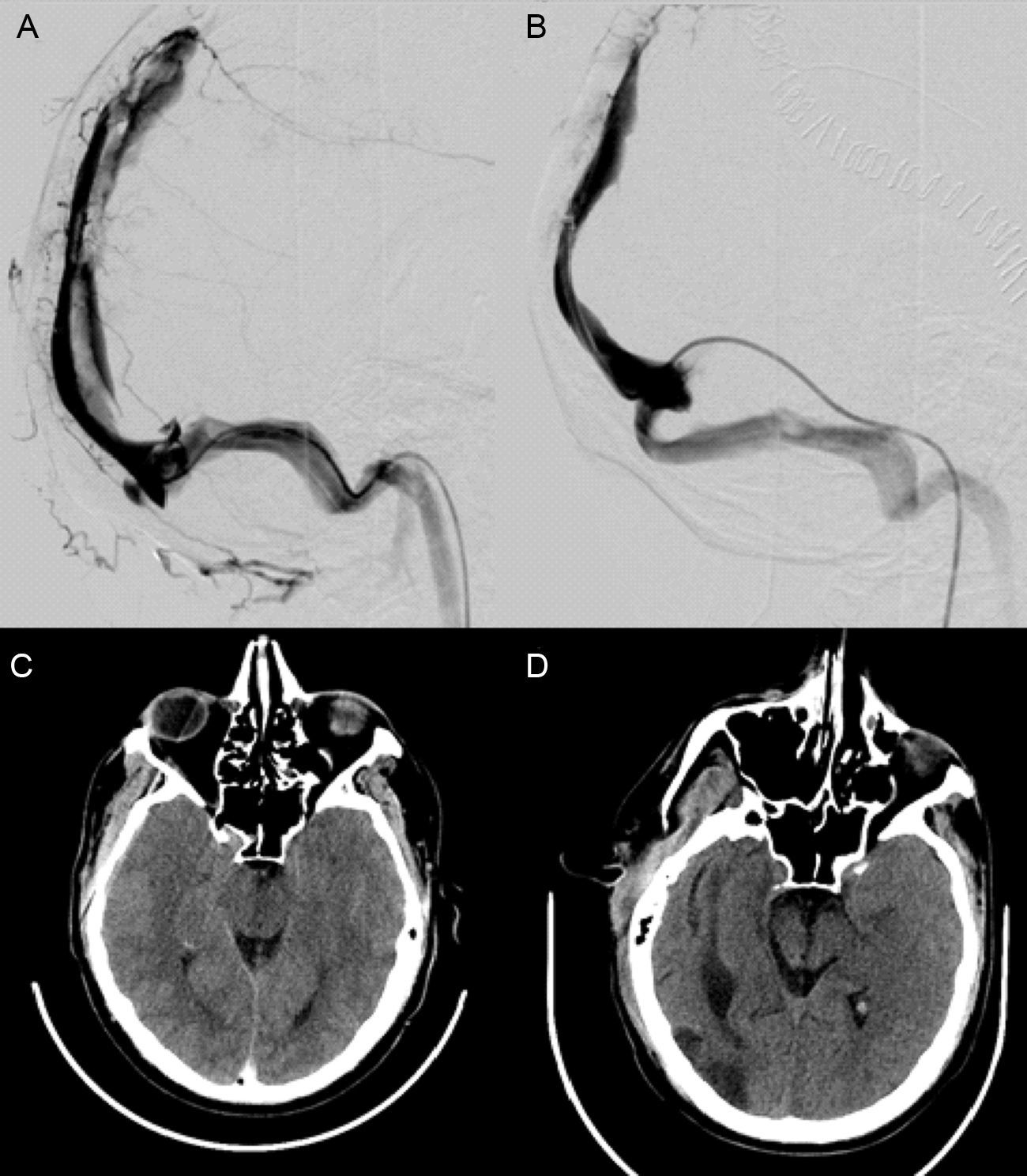
The patient presented a Glasgow Coma Score (GCS) of 14/15 points, with left hemiparesis and disorientation. Admission to the Intensive Care Unit (ICU) was decided, with the start of heparin sodium infusion. Over the following hours, and in view of the neurological deterioration, a brain CT scan was performed, revealing an increase in size of the hematoma, while phlebography showed the absence of opacification of the superior longitudinal and right transverse sinuses, suggestive of thrombosis (Fig. 1A). Mechanical thrombectomy proved ineffective. Local fibrinolysis was therefore decided (urokinase 60,000IU/h), following placement of a catheter in the longitudinal sinus.
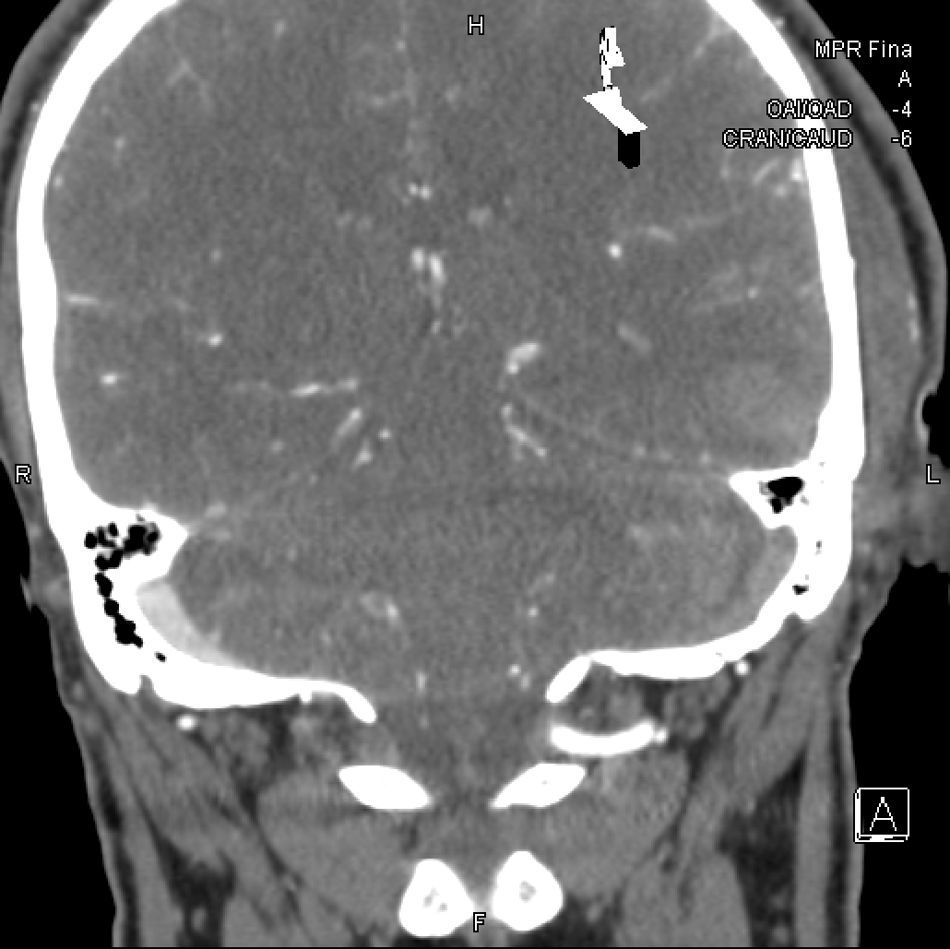
(A) Phlebography showing a filling defect in the superior longitudinal sinus. (B) Phlebography with the absence of filling defects and adequate drainage through the left transverse sinus. (C) Brain CT scan showing evidence of intracranial hypertension (bilateral erasure of the convexity sulci, diminished basal cistern size, increased mesencephalic anteroposterior axis). (D) Brain CT scan at discharge, showing improvement of the indirect signs of intracranial hypertension.
In the course of the following hours the patient presented right-side mydriasis. Measures for the control of intracranial pressure (ICP) were therefore adopted–the CT scan revealing intracranial hypertension without drainable lesions. An intraparenchymal ICP sensor was placed (Fig. 1C). Despite the measures adopted, the ICP values remained >25mmHg; urgent decompressive craniotomy (DC) was therefore performed and local fibrinolysis was continued. Repeat surgery was decided after 72h, expanding the DC due to intracranial hypertension secondary to extracranial hematoma overlying the initial craniectomy.
Local fibrinolysis was subsequently maintained, and control phlebography revealed effective drainage through the left transverse sinus, with partial repermeabilization of the right transverse sinus (Fig. 1B). In view of the above, local fibrinolysis was suspended and systemic anticoagulation was started, with no bleeding complications.
Clinical and radiological stabilization was subsequently observed (Fig. 1D), and the patient was moved to the hospital ward after 26 days in the ICU, with a GCS of 14/15 points and left hemiplegia.
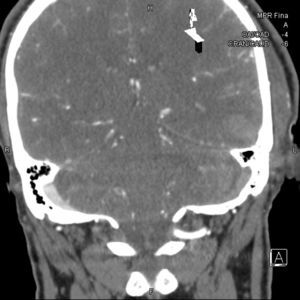
The second case corresponded to a 56-year-old male with a history of arterial hypertension and peripheral vertigo who suffered a fall from a height of one meter, with occipital traumatic brain injury (TBI). The patient reported to the emergency service with agitation, disorientation and a GCS of 14/15 points. The brain CT scan revealed skull base fracture with involvement of the left petrous part of the temporal bone and left occipital fracture, as well as laceration and thrombosis of the left transverse and sigmoid sinuses, with the extension of thrombosis toward the ipsilateral internal jugular zone (Fig. 2). Admission to the ICU for monitoring and pressure control was decided, adopting an expectant approach with regard to anticoagulation. The patient remained 12 days in the ICU, with imaging controls, and a GCS of 14/15 points at all times. Discharge from intensive care was therefore decided, without residual neurological defects.
Cerebral venous thrombosis is an infrequent condition that poses diagnostic and management problems. The annual incidence is 1.3 cases per 100,000 inhabitants.1 Cerebral venous thrombosis secondary to traumatic brain injury is even less frequent–accounting for approximately 4% of all cases of CVT.2 Cerebral venous thrombosis is particularly frequent in women between 20 and 35 years of age, being associated to pregnancy or puerperium and the use of oral contraceptives. The disorder accounts for 0.5% of all cerebrovascular events.3 The manifestations at onset usually comprise headache, seizures, and focal neurological defects.4
With regard to diagnosis, magnetic resonance imaging combined with venous resonance imaging is the technique of choice, though CT venography is an adequate alternative and is more widely available.3
Patients with spontaneous thrombosis of the sinuses and with no contraindications to anticoagulation should receive low molecular weight heparin or unfractionated heparin via the intravenous route in order to double the activate partial thromboplastin time and arrest the thrombotic process.5 At present, anticoagulation with low molecular weight heparin is advised, since it is more stable and no adjustment of the coagulation times is required. General antiedema measures should be added to anticoagulation: raising of the patient headrest, recording of mean arterial pressures in order to maintain a cerebral perfusion pressure of >70mmHg, normothermia, and the avoidance of solutions containing dextrose.
The prescription of antiepileptic drugs for the prevention or management of seizures is subject to controversy, and no studies supporting their use are available.6 In those cases where neurological worsening is observed despite anticoagulant therapy,7 with no associated intracranial hypertension, endovascular procedures are recommended in centers with experience in the use of such techniques.8 The efficacy of endovascular mechanical extraction or local fibrinolysis is not supported by clinical trials but by case series; the level of evidence supporting the benefits of such measures is therefore limited.4 Decompressive craniectomy could offer benefit in patients that develop malignant intracranial hypertension, and in cases where initial medical treatment has moreover failed.9
In our first case, mechanical thrombectomy proved ineffective. We subsequently administered local fibrinolysis through the longitudinal sinus catheter, since the restoration of flow is faster and more efficient than with heparin, assuming the bleeding risk.4
However, in the case of traumatic CVT, anticoagulant use is controversial and should be indicated on an individualized basis, since favorable outcomes have been reported in patients without neurological impairment or complications, in which an expectant approach has been decided.2,10
Please cite this article as: Sevilla Martinez M, Lorente Conesa MC, Silvente Fernandez S, García Bautisita E, Guerrero López F. Trombosis venosa cerebral: una misma enfermedad con diferentes abordajes. Med Intensiva. 2017;41:377–379.