In patients without spontaneous respiratory efforts, driving pressure (DP) of the respiratory system is defined as the difference between plateau pressure and positive end-expiratory pressure (Pplat–PEEP), quantified in static conditions. However, it can also be expressed as the association between tidal volume and compliance of respiratory system under static conditions (TV/Cstat), which is representative of the stress applied to the lungs. The importance of this parameter was already proposed by the team led by Amato back in 1998. Twenty years later, the same team associated DP with mortality in patients with acute respiratory distress syndrome (ARDS).1,2
However, although the term DP has been used indistinctively to refer to the difference between Pplat – PEEP and the TV/Cstat ratio, and has become established in the routine clinical practice, some authors don’t think that it is appropriate. It is questioned whether the difference between 2 static variables registered at the end of inspiration and expiration can be defined (where the established PEEP can be different compared to the total PEEP), as well as the correlation between TV and Cstat. Therefore, the term tidal pressure (TP) to define TV/Cstat was proposed against the term DP (Pplat–PEEP).3
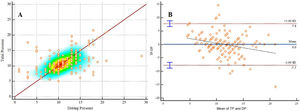
In this context, we tried to verify the degree of correlation between DP (Pplat–PEEP) and TP (TV/Cstat). Therefore, using data from our registry of patients with COVID-19 developed after obtaining approval from the local research ethics committee and the patients/representatives’ consent (in print and/or through the phone) the Pearson correlation coefficient and the Bland-Altman correlation analysis were used to describe the correlation between DP and TP. The statistical software package MedCalc® version 19.5.3 was used (MedCalc Software Ltd, Ostende, Bélgica; https://www.medcalc.org; 2020).
The analysis included all adult patients admitted with confirmed infection due to SARS-CoV-2 treated with volume-controlled continuous mandatory mechanical ventilation (VC-CMV). While in the supine position, after sedation and neuromuscular blocking within the first 24 h after starting mechanical ventilation (MV) the following parameters were quantified: Cstat (estimated with the values obtained from this expression: Cstat = TV/Pplat – PEEP), PEEP (total PEEP = PEEP administered + AutoPEEP; through a pause at the end of expiration), TV administered and Pplat (quantified in the zero flow point during the pause at the end of expiration).
Data from 185 patients were analyzed—129 men (69.7%)–with a median age of 65 years (p25–75: 56–72). The most widely described comorbidity in 102 patients was arterial hypertension (55%) followed by dyslipidemia (39%), and diabetes mellitus (25%). The median of the PaO2/FiO2 ratio when patients were connected to mechanical ventilation was 108 (p27–75: 90–132). The 28-day mortality rate of the entire cohort was 14.6%.
DP and TP kept a moderate correlation (Fig. 1A; r2 = 0.44; 95%CI, 0.31–0.55; P < .0001). The Bland-Altman analysis confirmed that TP was higher compared to DP with a mean of 0.02 cmH2O with 95% confidence intervals from −0.58 to 0.63. The line of regression estimated for the differences reveals a negative tendency of the differences parallel to the growth of the magnitude of the variable quantified (Fig. 1B).
Pearson correlation coefficient (1 A), and Bland-Altman analysis (1 B) comparing driving pressure and tidal pressure.
DP, driving pressure; TP, tidal pressure; 1 A: Pearson r2 = 0,44; IC 95%, 0.31–0.55; P < .0001. 1 B: 0.02 cmH2O overestimation with 95% confidence intervals from −0.58 to 0.63.
In our cohort of patients, although TP slightly overestimates DP, both parameters seem to overlap in patients without spontaneous respiratory efforts. Maintaining pasive conditions (without flow) on both sides of the cycle when the Pplat and total PEEP are registered is essential.4 These conditions provide the lack of any inspiratory effort, which prevents Pplat underestimation (or overestimation if the patient exhales actively); and, on the other hand, facilitates the measurement of total PEEP (total PEEP = PEEP administered + AutoPEEP) through a pause at the end of expiration. However, we should mention that, at times, respiratory secretions can create a somehow unidirectional valve effect since in expiration they totally occlude the airway stopping the airflow from getting out completely. In these situations, AutoPEEP cannot be detected during the expiratory pause maneuver since the airways never make contact with the alveoli that are distal to secretions. The only way to detect entrapment would be to see what impact the changes made to the scheduled PEEP have on the Pplat during the inspiratory pause. AutoPEEP won’t be measured: non-dynamic non readily quantifiable AutoPEEP.5
Similarly, we agree with Marini and Baldomero, who think that, while in the search for the main variables revealing stretching and alveolar damage, the concept of TP can be confusing as a bedside variable because it can promote the idea that translates the information of the total dynamic pressure necessary to overcome the resistive and the elastic components.6
In restrictive situations, the normal thing to do is that inspiratory and expiratory times administered should be long enough to be able to equalize working and alveolar pressures (it would take over 3 constants of time). However, if the situation under which dynamic data are obtained is influenced by increased resistances, then the mechanical power applied could be overestimated or else the system Cstat underestimated. In conclusion, the takeaway from our study is that static quantifications should be made here.
Once this has been taken into consideration, in our study we did not have any problems associated with using pressure-controlled continuous mechanical ventilation (PC-CMV) or not making pauses. Therefore, based on our own data, we believe DP is more useful compared to TP to show the system static conditions.
FundingNone whatsoever.
Conflicts of interestNone reported.