To identify predictors of mortality and neurological function in adult ICU patients recovering from cardiac arrest.
DesignA prospective cohort multicenter study was carried out.
SettingForty-six polyvalent ICUs.
PatientsA total of 595 patients recovering from out-of-hospital cardiac arrest (OHCA, n=285) or in-hospital cardiac arrest (IHCA, n=310).
Main outcome variablesSurvival and recovery of neurological function.
ResultsThe mean cardiopulmonary resuscitation time was 18min (range 10–30). Moderate hypothermia was used in 197 patients, and 150 underwent percutaneous coronary intervention (PCI). Return of spontaneous circulation (ROSC) was achieved within 20min in 370 patients. Variables associated to mortality (ICU and in-hospital) were age (odds ratio [OR]=1.0, 95%CI 1.0–1.0 per year), non-cardiac origin of cardiac arrest (OR=2.16, 95%CI 1.38–3.38; P=0.001) and ROSC >20min (OR=3.07, 95%CI 1.97–4.78; P<0.001), whereas PCI and the presence of shockable rhythm exhibited a protective effect. Favorable neurological outcome was associated to shockable rhythm, ROSC <20min, and cardiac origin of arrest. Hypothermia did not affect survival or neurological outcome in the multivariate analysis.
ConclusionsAge, non-cardiac origin of cardiac arrest and ROSC >20min were predictors of mortality. In contrast, cardiac arrest of cardiac origin, ROSC <20min, and defibrillable rhythms were associated to unfavorable neurological outcomes.
Identificar predictores de mortalidad y de función neurológica en pacientes adultos ingresados en las UCI, recuperados de una parada cardíaca.
DiseñoEstudio prospectivo de cohortes multicéntrico.
ÁmbitoCuarenta y seis UCI polivalentes.
PacientesSe incluyeron 595 pacientes recuperados de una parada cardíaca extrahospitalaria (OHCA, n=285) o intrahospitalaria (IHCA, n=310).
Variables de interés principalesSupervivencia y recuperación de la función neurológica.
ResultadosEl tiempo medio de reanimación cardiopulmonar fue de 18min (rango: 10-30). Se usó hipotermia moderada en 197 pacientes, y 150 se sometieron a intervención coronaria percutánea (PCI). El retorno de la circulación espontánea (ROSC) se logró en 20min en 370 pacientes. Las variables asociadas con la mortalidad (UCI y en el hospital) fueron la edad (odds ratio [OR]: 1,0; IC 95%: 1,0-1,0 por año), origen no cardíaco de la parada cardíaca (OR: 2,16; IC 95%: 1,38-3,38; p=0,001) y el ROSC>20min (OR: 3,07; IC 95%: 1,97-4,78; p<0,001), mientras que la PCI y la presencia de ritmo desfibrilable mostraron un efecto protector. El resultado neurológico favorable se asoció con ritmo desfibrilable, ROSC<20min y origen cardíaco de la parada. En el análisis multivariable, la hipotermia no afectó a la supervivencia ni al resultado neurológico.
ConclusionesLa edad, el origen no cardíaco de la parada cardíaca y el ROSC>20min fueron predictores de mortalidad. Por el contrario, la parada cardíaca de origen cardíaco, el ROSC<20min, y los ritmos desfibrilables se asociaron con un resultado neurológico favorable.
Sudden cardiac arrest is a major clinical and public health problem, with high mortality rates and the potential for irreversible and profound neurological damage and functional disability. Numerous factors can affect reported incidence and outcomes of out-of-hospital cardiac arrest (OHCA) and in-hospital cardiac arrest (IHCA), primarily because of differences in the underlying sources of data, populations included, types or causes of cardiac arrest, use of different tools to assess specific outcomes, or how cardiac arrest variables are collected and reported.1–3 Survival and neurological recovery following cardiac arrest are affected by multiple interdependent variables that include individual patient characteristics, emergency medical service (EMS) or hospital system characteristics, and circumstantial factors specific to the event.4,5 As incidence, survival, and neurological outcome are influenced by a number of modifiable (e.g. provision of health care) and non-modifiable (e.g. patient characteristics or location of arrest) factors,6,7 the development of national large registries of cardiac arrest is an essential first step for surveillance and quality improvement purposes.8–10
Several countries have developed collective efforts to develop OHCA registries, such as the Pan-Asian Resuscitation Outcomes Study (PAROS) network,11 the European Registry of Cardiac Arrest (EuReCa),12,13 the Cardiac Arrest Registry to Improve Survival (CARES),14,15 the All-Japan Utstein registry,16 the Victoria Ambulance Cardiac Arrest Registry (VACAR),17 the UK National Cardiac Arrest Audit (NCAA) database,18 or the Irish Out of Hospital Cardiac Arrest Register (OHCAR).19 Registries allow for the precise measurement of the mortality and morbidity burden of cardiac arrest, can better guide the selection and implementation of public health interventions, help to determine appropriate allocation of resources, identify at-risk or vulnerable populations, and eliminate potential care disparities through targeted interventions.20 Moreover, it can allow researchers to assess the impact of current and emerging treatments and provide an evidence base for high-quality care and best practices.
In Spain, knowledge about the epidemiology of cardiac arrest is still insufficient,21,22 although results of the first year (2013–1024) of the Out-of-Hospital Spanish Cardiac Arrest Registry (OHSCAR) revealed that OHCA affects a relatively young population, more than a half at home, with bystander of basic life support being performed hardly in one out of three cases.23 In the framework of the National Plan for Cardiopulmonary Resuscitation (PNRCP), a national registry of ICU patients recovering from OHCA or IHCA was developed with the support of the Spanish Society of Intensive Care Medicine and Coronary Units (SEMICYUC).24 The main objectives of this study were identify predictors of mortality and neurological function adult patients recovering from cardiac arrest admitted to Spanish ICUs.
MethodsStudy design and settingA prospective cohort multicenter study was conducted with the participation of 46 polyvalent ICUs throughout Spain, in which adult patients (18 years or older) with cardiological, medical or surgical conditions are admitted. The primary objective of the study was to determine predictors of mortality and neurological function. Secondary objectives were as follows: (a) to assess the clinical characteristics of patients recovering from cardiac arrest requiring ICU care, and (b) to evaluate the effect of moderate hypothermia on neurological outcome after successful cardiopulmonary resuscitation (CPR).
The study protocol (SAS/3470/2009) was approved by the Clinical Research Ethics Committee of Hospital Universitario de Valme, Sevilla, Spain, which was the reference center for this study (approval date December 16, 2014). Written informed consent was obtained from the patients or their legally authorized representatives. The study had the scientific support of the Working Group of Cardiologic Intensive Care of the SEMICYUC.
Study populationBetween January 2014 and June 2015, all consecutive patients aged 18 years or older who had recovered from a first cardiac arrest, either OHCA or IHCA, after advanced life support measures admitted to the participating ICUs were eligible. Patients with cardiac arrest of primary cardiac cause and non-cardiac origin were included, independently of the heart rhythm such as ventricular fibrillation, ventricular tachycardia, asystole, or electrical activity without pulse (electromechanical dissociation). Patients in whom death was the predictable outcome of their illness or after starting life support measures were excluded from the study as were those with a prior ‘do not resuscitate’ order.
Inclusion criteria for moderate (32–34°C) hypothermia were as follows: witnessed cardiac arrest, no purposeful movement to command and Glasgow Coma Scale <8 after recovery of spontaneous circulation, CPR initiated between 5 and 15min of cardiac arrest, and interval between initiation of resuscitation measures and recovery of spontaneous circulation (ROSC) ≤30min. Exclusion criteria were tympanic temperature <32°C; pregnancy; hypotension (mean arterial pressure <60mm Hg or systolic blood pressure <90mm Hg) despite the use of vasoactive drugs for >30min; hypoxemia with arterial oxygen saturation (SaO2) <85% for more than 25min; uncontrolled bleeding, thrombocytopenia or other coagulopathy; other causes of coma (head trauma, cerebrovascular accident, CNS depressant drugs, etc.); and terminal disease.
Data collectionData were entered electronically via a web-based platform (https://pcr-hipotermia.investigacion-intensivos.org) to create the first national registry of patients recovering from cardiac arrest and the use of therapeutic hypothermia in Spanish ICUs. Data were collected according to Utstein-style guidelines25 as recommended by the American Heart Association, defined and classified into four core elements as system, patient, process, and outcome (Figure 1, Supplementary online material). Variables included in the Utstein standard reporting template were collected at the time of the acute event, at hospital discharge, and at 6 and 12 months after cardiac arrest. Neurological outcome was defined according to the Cerebral Performance Category Scale (CPS)26 (1: return to normal cerebral function and normal living; 2: cerebral disability but sufficient function for independent activities of daily living; 3: severe disability, limited cognition, inability to carry out independent existence; 4: coma or vegetative state (unconscious); 5: brain death). Patients with CPC 1 or 2 were classified into favorable neurological outcome (normal/moderate) and those with CPC 3 and 4 into unfavorable neurological outcome (severe/coma).
Data on vital status and neurological function at 6 and 12 months after hospital discharge were collected by telephone follow-up, using the CPS scale27 and the Barthel index to rate activities of daily living.27
Statistical analysisIn a small previous survey of different participating ICUs, it was considered as average the admission to the ICU between 12 and 18 patients recovering from cardiac arrest annually, with an estimated sample of about 360 patients per year.
Categorical variables are expressed as frequencies and percentages, and continuous variables as median and interquartile range (IQR) (25th–75th percentile). Percentages were compared with the chi-square (χ2) test and medians with the Wilcoxon rank-sum test for independent samples. In order to identify the variables that maintained independent association with each outcome, a multivariable logistic regression was performed. Models were summarized by their coefficients and the corresponding standard errors (SE), P values and adjusted odds rations (OR) with the 95% confidence interval (CI). For the predictors of the outcome deduced from the logistic model, an analysis of receiver operating characteristics (ROC) was carried out. The corresponding ROC curve was obtained and the area under curve (AUC) was estimated by means of a 95% CI. The discriminant threshold was chosen as one that minimizes using the closest top left criterion as follows: (1−sensitivity)2+(1−specificity)2. The corresponding sensitivity, specificity and predictive values were estimated by means of 95% CI. Also, in order to assess the final neurological outcome, the classification and regression trees (CART) procedure was used to predict the CPS class of each patient. The basis of the decision tree algorithms is the binary recursive partitioning of the data. The most discriminative variable is first selected to partition the data set into child nodes. The splitting continues until some stopping criterion is reached. At each terminal node, the probability of each class was estimated as the proportion of patients belonging to that node that developed the event. The tree was constructed according to the following algorithm: in the first stage, the tree grows until all cases are correctly classified, and in the second stage, we used the tenfold cross-validation method of successive pruning. Finally, the tree that minimized the error measurement (deviance) was chosen. Statistical significance was set at P<0.05. Data were analyzed using the R package, version 3.1.0.
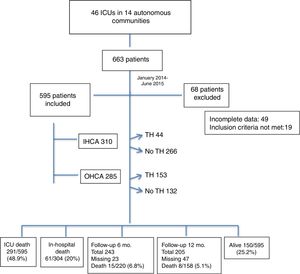
ResultsStudy populationBetween January 2014 and June 2015, a total of 663 patients recovering from cardiac arrest were admitted to the ICU but 68 (10.2%) were excluded because inclusion criteria were not met (n=19) or incomplete data collection (n=49). The study population included 595 patients, with a median age of 68 years admitted to 46 ICUs of 14 autonomous communities throughout Spain. Fig. 1 shows the disposition of patients according to the site of cardiac arrest (OHCA, n=285; IHCA, n=310), use of therapeutic hypothermia (n=197), and final outcome. The Utstein standardized template for reporting outcomes of cardiac arrest is shown in Figure 1 of the supplementary online material. Salient data of the study population included a predominance of males (69.4%), presence of bystanders in 48.6% of the cases, cardiac cause of arrest in 57.3%, shockable rhythms in 47.2%, ROSC between 30s and 20min in 62.2%, median total CPR time 18min, therapeutic moderate hypothermia in 33.1%, and percutaneous coronary intervention (PCI) in 25.2%.
ICU and in-hospital mortalityA total of 291 patients (48.9%) died during their ICU stay and 61 (10.2%) during hospitalization, with an overall mortality rate of 59.1% (352/595). Variables associated with ICU mortality and overall mortality are shown in Table 1. Age, non-cardiac cause of cardiac arrest and duration of ROSC were significant factors related to ICU mortality. Also, among patients who died, there were significantly lower percentages of shockable rhythms, PCI procedures, and therapeutic hypothermia. Similar results were observed regarding factors associated with overall in-hospital mortality.
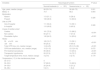
Variables associated with ICU mortality and overall mortality in patients recovering from cardiac arrest.
| Variables | All patients | Death in the ICU | Overall deaths in the ICU and hospital | ||||
|---|---|---|---|---|---|---|---|
| n=595 | No, n=304 | Yes, n=291 | P value | No, n=243 | Yes, n=352 | P value | |
| Age, years, median (range) | 68 (56–77) | 66 (53–75) | 70 (58.5–78) | 0.002 | 66 (53–74) | 70 (58–78) | <0.001 |
| Males, % | 69.4 | 68.8 | 70.1 | 0.720 | 70.0 | 60.0 | 0.810 |
| Bystanders | |||||||
| Absent | 306 (51.4) | 149 (49.0) | 157 (54.0) | 0.228 | 121 (49.8) | 185 (52.6) | 0.508 |
| Present | 289 (48.6) | 155 (51.0) | 134 (46.0) | 122 (50.2) | 167 (47.4) | ||
| Site of CPR | |||||||
| Out-of-hospital | 285 (47.9) | 148 (48.7) | 137 (47.1) | 0.695 | 124 (51.0) | 161 (45.7) | 0.204 |
| In-hospital | 310 (52.1) | 156 (51.3) | 154 (52.9) | 119 (49.0) | 191 (54.3) | ||
| Cause of cardiac arrest | |||||||
| Cardiac | 341 (57.3) | 208 (68.4) | 133 (45.7) | <0.001 | 176 (72.4) | 165 (46.9) | <0.001 |
| Non-cardiac | 254 (42.7) | 96 (31.6) | 158 (54.3) | 67 (27.6) | 187 (53.1) | ||
| Shockable rhythm | 281 (47.2) | 182 (59.9) | 99 (34.0) | <0.001 | 156 (64.2) | 125 (35.5) | <0.001 |
| ROSC | |||||||
| 30s to 20min | 370 (62.2) | 218 (71.7) | 152 (52.2) | <0.001 | 178 (73.3) | 192 (54.5) | <0.001 |
| >20min | 225 (37.8) | 86 (28.3) | 139 (47.8) | 65 (26.7) | 160 (45.5) | ||
| Total CPR time, min, median (range) | 18 (10–30) | 15 (7–27) | 20 (12–31) | <0.001 | 15 (6–27) | 20 (11.5–30) | <0.001 |
| CPR time defibrillation, min, median (range) | 11 (6–17) | 10 (5–16) | 12 (7–18) | 0.042 | 10 (5.5–15) | 12 (6–18) | 0.112 |
| PCI treatment procedures | 150 (25.2) | 108 (35.5) | 42 (14.4) | <0.001 | 95 (39.1) | 55 (15.6) | <0.001 |
| Therapeutic hypothermia | 197 (33.1) | 116 (38.2) | 81 (27.8) | 0.007 | 99 (40.7) | 98 (27.8) | 0.001 |
| Target temperature time, hours, median (range) | 3 (2–6) | 4 (2–6) | 2 (1.5–4) | 0.002 | 4 (2–6) | 3 (2–5) | 0.095 |
| Temperature (°C) in the maintenance phase | |||||||
| 30–31.9 | 6 (3.1) | 1 (0.9) | 5 (6.2) | 0 | 6 (6.2) | ||
| 32–33.9 | 132 (67.7) | 76 (66.1) | 56 (70.0 | 67(68.4) | 132 (67.7) | ||
| 34–35.9 | 47 (24.1) | 29 (25.2) | 18 (22.5) | 25 (25.5) | 47 (24.1) | ||
| 36–38.4 | 10 (5.1) | 9 (7.8) | 1 (1.2) | 6 (6.1) | 4 (4.1) | ||
CPR: cardiopulmonary resuscitation; ROSC: return of spontaneous circulation; PCI: percutaneous coronary intervention; range means interquartile range (25th-75th percentile). Data expressed as frequencies and percentages in parenthesis unless otherwise stated.
In the multivariable analysis (Table 2), age, non-cardiac cause of cardiac arrest, ROSC >20min, and total CPR time were independently associated with death during stay in the ICU. By contrast, shockable rhythm and PCI procedure were inversely associated with ICU mortality. The same variables were selected in the logistic regression model for overall in-hospital mortality (Table 2). Results of ROC analyses based on predictive scores derived from the logistic regression models for ICU mortality and in-hospital mortality are shown in Figures 2 and 3 of the supplementary online material. The closest.topleft discriminant threshold for death during ICU stay was −0.1394, with 74.2% (95% CI 68.8–79.2) sensitivity and 62.3% (95% CI 56.7–67.9) specificity. The closest.topleft discriminant threshold for overall in-hospital mortality was 0.2977, with a sensitivity of 73.9% (95% CI 68.9–78.4) and a specificity of 65.3% (95% CI 58.9–71.3).
Results of multivariate analysis. Variables associated with ICU mortality and overall in-hospital mortality.
| Variables | Coefficient (β) (standard error) | P value | Odds ratio (95% confidence interval) |
|---|---|---|---|
| Death during stay in the ICU | |||
| Age, for each year | 0.019 (0.006) | 0.002 | 1.02 (1.01 to 1.03) |
| Non-cardiac cause of cardiac arrest | 0.662 (0.218) | 0.002 | 1.94 (1.26 to 2.97) |
| ROSC >20min | 1.069 (0.215) | <0.001 | 2.91 (1.91 to 4.44) |
| Total CPR time | 0.016 (0.006) | 0.008 | 1.02 (1.00 to 1.03) |
| Shockable rhythm | −0.898 (0.214) | <0.001 | 0.41 (0.27 to 0.62) |
| PCI procedure | −0.614 (0.246) | 0.013 | 0.54 (0.33 to 0.88) |
| Constant term (intercept) | −1.763 (0.513) | <0.001 | |
| Death during hospitalization | |||
| Age, for each year | 0.022 (0.006) | <0.001 | 1.0 (1.00 to 1.03) |
| Non-cardiac cause of cardiac arrest | 0.770 (0.229) | <0.001 | 2.16 (1.38 to 3.38) |
| ROSC >20min | 1.122 (0.226) | <0.001 | 3.07 (1.97 to 4.78) |
| Total CPR time | 0.015 (0.006) | 0.02 | 1.01 (1.00 to 1.03) |
| Shockable rhythm | −0.960 (0.218) | <0.001 | 0.38 (0.25 to 0.59) |
| PCI procedure | −0.602 (0.240) | 0.012 | 0.54 (0.34 to 0.88) |
| Constant term (intercept) | −1.428 (0.520) | 0.006 | |
ROSC: return of spontaneous circulation; CPR: cardiopulmonary resuscitation; PCI: percutaneous coronary intervention.
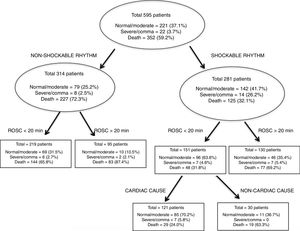
Of the 243 patients who were alive at hospital discharge, 221 (90.9%) showed a normal/moderate neurological function and 22 (9.0%) an unfavorable neurological outcome (severe/coma). As shown in Table 3, patients in the severe/coma group were significantly younger and presented shockable rhythms less frequently as compared to patients with normal/moderate neurological function. Other differences included a higher percentage of patients with of non-cardiac cause of cardiac arrest, ROSC >20min, longer duration of CPR, therapeutic hypothermia, and PCI procedures in the severe/coma group. The classification tree of the neurological outcome at hospital discharge is shown in Fig. 2. The most favorable neurological outcome was observed in the nodes of shockable rhythm, ROSC <20min, and cardiac cause of cardiac arrest, with 70.2% (95% CI 80.7–94.0) of patients with normal neurological function or moderate neurological dysfunction. By contrast, the worse neurological outcome was observer in the nodes of non-shockable rhythm and ROSC >20min, with 87.4% (95% CI 62.1–78.4) of patients with severe neurological dysfunction or in a comatose state.
Neurological outcome at hospital discharge in 243 cardiac arrest survivors.
| Variables | Neurological function | P value | |
|---|---|---|---|
| Normal/moderate (n=221) | Severe/coma (n=22) | ||
| Age, years, median (range) | 66 (53–74) | 56 (49–72) | 0.001 |
| Males, % | 70.1 | 68.2 | 0.954 |
| Bystanders | |||
| Absent | 113 (51.1) | 8 (36.4) | 0.326 |
| Present | 108 (48.9) | 14 (63.6) | |
| Site of CPR | |||
| Out-of-hospital | 111 (50.2) | 13 (59.1) | 0.326 |
| In-hospital | 110 (49.8) | 9 (40.9) | |
| Cause of cardiac arrest | |||
| Cardiac | 161 (72.9) | 15 (68.2) | <0.001 |
| Non-cardiac | 60 (27.1) | 7 (31.8) | |
| Shockable rhythm | 142 (64.3) | 14 (63.6) | <0.001 |
| ROSC | |||
| 30s to 20min | 165 (74.7) | 13 (59.1) | <0.001 |
| >20min | 56 (25.3) | 9 (40.9) | |
| Total CPR time, min, median (range) | 14 (6–25) | 25.5 (15–38) | <0.001 |
| CPR time defibrillation, min, median (range) | 10 (5–15) | 12.5 (9–18) | 0.072 |
| PCI treatment procedures | 85 (38.5) | 10 (45.5) | <0.001 |
| Therapeutic hypothermia | 83 (37.6) | 16 (72.7) | <0.001 |
| Target temperature time, hours, median (range) | 4 (2–6) | 3 (2–5) | 0.179 |
| Temperature (°C) in the maintenance phase | |||
| 30–31.9 | 0 | 0 | |
| 32–33.9 | 57 (69.5) | 10 (62.5) | |
| 34–35.9 | 20 (24.4) | 5 (31.2) | |
| 36–38.4 | 5 (6.1) | 1 (6.2) | |
CPR: cardiopulmonary resuscitation; ROSC: return of spontaneous circulation; PCI: percutaneous coronary intervention; range means interquartile range (25th–75th percentile). Data expressed as frequencies and percentages in parenthesis unless otherwise stated.
Of the 243 patients who were discharged alive from the hospital, at 6 months follow-up, 23 patients were missing and 15 had died, with a mortality rate of 6.8% (15/220). At 12 months, 47 patients were missing and 8 patients died, with a mortality rate of 5.1% (8/158). The CPC category was I or II in 32% and III or IV in 1.5%. According to the Barthel index, 22.3% of patients were fully independent, 6.4% dependent, and 2.2% totally dependent. In most cases, neurological outcome at 6 months was maintained at 12 months.
Therapeutic hypothermiaTherapeutic hypothermia used in 197 patients (33.1%) was significantly associated with survival. The ICU mortality rate was 27.8% in the hypothermia group as compared to 38.2% in the non-hypothermia group (P=0.007); also, the overall in-hospital mortality rate was lower among patients treated with hypothermia (27.8% vs. 40.7%, P=0.001). As shown in Table 4, patients treated with hypothermia as compared to those not treated with hypothermia were significantly younger and showed higher percentages of cardiac cause of arrest, shockable rhythms, and longer duration of CPR. These variables were independently associated with hypothermia in the logistic regression analysis (Table 4).
Variables significantly associated with moderate therapeutic hypothermia.
| Variables | All patients | Therapeutic hypothermia | P value | |
|---|---|---|---|---|
| (n=595) | No (n=398) | Yes (n=197) | ||
| Age, years, median (range) | 68 (56–77) | 70 (60–78) | 61 (50–72) | <0.001 |
| Cause of cardiac arrest | ||||
| Cardiac | 341 (57.3) | 192 (48.2) | 149 (75.6) | <0.001 |
| Non-cardiac | 254 (42.7) | 206 (51.8) | 48 (24.4) | |
| Shockable rhythm | 281 (47.2) | 149 (37.4) | 132 (67.0) | <0.001 |
| Total CPR time, min, median (range) | 18 (10–30) | 15 (7–25) | 24 (15–36.5) | <0.001 |
| Logistic regression model | |||
|---|---|---|---|
| Variables | Coefficient (β) (SE) | P value | Odds ratio (95% confidence interval) |
| Age, for each year | −0.033 (0.007) | <0.001 | 0.97 (0.96 to 0.98) |
| Non-cardiac cause of arrest | −0.771 (0.217) | 0.001 | 0.46 (0.29 to 0.73) |
| Shockable rhythm | 0.766 (0.217) | <0.001 | 2.15 (1.40 to 3.29) |
| Total CPR time | 0.023 (0.006) | <0.001 | 1.02 (1.01 to 1.03) |
| Constant term (intercept) | 0.747 (0.748) | 0.318 | |
CPR: cardiopulmonary resuscitation.
The present study present relevant clinical data of a representative homogeneous sample of adult patients recovering from cardiac arrest and admitted to Spanish ICUs28 over a 17-month period and followed for 12 months after the index episode. We cannot report incidence data since the total number of patients suffering from cardiac arrest attended during the study period is unknown. However, the international, prospective, multicenter EuReCa ONE study of patients who suffered an OHCA during October 2014 attended and/or treated by an EMS from 248 regions in 27 countries, covering an estimated population of 174 million, provided disaggregated data by country.12 For Spain, with a total population of 47,270 inhabitants covering all 17 autonomous communities, an incidence of cardiac arrest of 28 cases per 100,000 inhabitants per year, and an incidence of 19 cases of CPR per 100,000 cases per year was reported.12 Using these data and analyses, different countries, regions, systems, and concepts can benchmark them-selves and may learn from each other to further improve survival.
The templates Utstein-style contribute to improved public health internationally by providing a structured framework with which to compare medical services systems. Representatives of the International Liaison Committee on Resuscitation developed updated Utstein guidelines during 2012 through 2014, with recommendations for reporting OHCA.26 Data elements were grouped by system factors, dispatch/recognition, patient variables, resuscitation/post-resuscitation processes, and outcomes. This template facilitates reporting of the rhythms treated as an efficacy measure of medical services. The update of the IHCA templates is currently pending.
Epidemiological data in our study included a predominance of males, mean age in the sixth decade, bystanders providing resuscitation measures in 48.6% of cases, quite similar rates of OHAC and IHCA, cardiac cause of arrest in 57.3% of cases, shockable rhythms in 47.2%, and ROSC <20min in 62.2%. Data of other studies carried out in Spain have shown similar results.23,29–31 In 8997 patients with OHCA attended by an emergency team of the Spanish EMS over 1-year period (2013–2014),23 72% were men with a mean age of 61 years, initial rhythm was shockable in 22.1% patients, and basic life support before emergency team arrival was provided by bystander in 30% of patients.
The primary objective of the study was to assess survival in patients admitted to the ICU after recovery from cardiac arrest. Of the 595 patients included in the study, 304 (51.1%) were alive at the time of ICU discharge. Sixty-one patients died during hospitalization, with an overall survival rate of 40.8%. Predictors of ICU and in-hospital mortality included age, non-cardiac cause of arrest, ROSC >20min, and CPR time, as well as the presence of shockable rhythms and PCI as protective factors. Cardiac arrest survival rates and the likelihood of good neurologic outcomes and functional status vary substantially according to disparities of the affected patient populations and related comorbidities, the quality of local chain, proximity to trained providers and appropriate treatments, and the number of transitions that must occur between various providers, such as EMS and hospital staff.32 In a recent large, prospective population-based registry conducted over 2 years in Paris, France, the survival rates were 7.3% (279/3816) among patients in which CRP was attempted and 21% (279/1335) among those who were admitted alive to the hospital.33 In the nationwide Danish Cardiac Arrest Registry of a study population of 19,468 patients, the 30-day survival improved from 3.5% in 2001 to 10.8% in 2010, which in turn was significantly associated with a concomitant increase in bystander CPR.34 Moreover, in an analysis of the Get with the Guidelines–Resuscitation Registry of patients with IHCA in the U.S., risk-adjusted rates of survival to discharge in the overall cohort of 84,625 hospitalized patients increased from 13.7% in 2000 to 22.4% in 2009.35 A prospective analysis of the UK National Cardiac Arrest Audit (NCAA) database with data related to 22,628 patients showed an overall unadjusted survival to hospital discharge of 18.4%.36 An analysis of trends in patient characteristics and outcome following admission to UK critical care units following CPR for the period 2004–2014 showed a reduction in mortality following ICU admission (OR 0.96 per year).37 Cariou et al.38 have reported ten priorities for strengthening the local chain of survival in OHCA, including high bystander CPR rate and early defibrillation programs in the community; good quality advanced life support; monitoring the quality of CPR (end-tidal carbon dioxide or near-infrared spectroscopy); developing advanced therapies in refractory cardiac arrest (mechanical chest compression devices, extracorporeal life support); improving post-resuscitation care (hypothermia, PCI); prognostication; rehabilitation; development of high-quality cardiac arrest registries; and to promote and develop high-quality research.
In relation to neurological outcome, shockable rhythm, ROSC <20min, and cardiac cause of arrest were associated with favorable neurological function. In a systematic review of the European Resuscitation Council and the European Society of Intensive Care Medicine,39 bilateral absence of either pupillary and corneal reflexes or N20 wave of short-latency somatosensory evoked potentials were identified as the most robust predictors of poor outcome in adult comatose survivors of cardiac arrest.
Sandroni et al.40 reported a comprehensive review on the prediction of neurological outcome after cardiac arrest and recommended prognostication tests (clinical examination, electrophysiology, biomarkers and neuroimaging) in patients who are comatose at 72h or more after ROSC. Among prognostic tests, ocular reflexes and somatosensory evoked potentials are the most robust. This multimodal approach combining multiple prognostication tests is recommended so that the risk of falsely pessimistic prediction is minimized.
In a systematic review and meta-analysis of 20 studies with 1845 patients, bilateral absence of pupillary reflexes more than 24h after ROSC, bilateral absence of corneal reflexes more than 24h, and bilateral absence of somatosensory-evoked potentials between days 1 and 7 accurately predicted poor neurological outcome.41 Martinell et al.42 presented a score with 10 variables for early identification of patients at high risk of poor prognosis after OHCA of presumed cardiac origin. This study is a post hoc analysis of a cohort of the Target Temperature Management trial applicable only to patients with OHCA of cardiac cause. Predictors of poor outcome were older age, non-defibrillable rhythm and duration of ROSC were similar to that found in our study. Other predictors such as Glasgow Coma score, partial pressure of CO2 in arterial blood value <4.5kPa at hospital admission, and lower pH would have been only applicable to patients with hypothermia in our study (n=197), so it is not possible to make an inference to the total 595 patients included in the study. Other variables such as the administration of adrenaline or the absence of bilateral pupillary of corneal reflexes were nor collected in our database, the design of which was previous to the statement of the European Resuscitation Council of the European Society of Intensive Care Medicine.39 A recent review by Narayan et al.1 describes new challenges to address the sudden cardiac arrest epidemics in the framework of responding, understanding, predicting and preventing. The response could be improved by technology assisted by community response systems (automated external defibrillator). Efforts to understand and predict cardiac arrest can be improved by refining the taxonomy along phenotypic and pathophysiological “risk axes” and prevention must integrate these concepts.
There is no single agreed physical disability measure. The Barthel index is proposed as the standard index for clinical and research purposes. There are few studies reporting long-term follow-up up to 12 months and most have been carried out up to 6 months after the event. Interestingly, the neurological sequelae data measured with the Barthel index after 12 months of the event, with a totally independent rate of 22%, are clinically relevant and have not been previously reported.
At present there is still controversy about the role of hypothermia as a post-resuscitation measure for survival and neurological outcome, and the term temperature control is preferred, 36°C as an objective, although it is still a subject of debate. At the time we designed the study, it was recommended by the European Resuscitation Council and, it seemed appropriate to include it as a study variable in those hospitals in which this technique was available. Therapeutic hypothermia was not selected as an independent predictor of survival in the multivariate analysis probably because other variables, such as age, shockable rhythm, non-cardiac cause of arrest, and duration of CPR were strongly associated with hypothermia. In a systematic review and meta-analysis of 11 studies, the use of therapeutic hypothermia after OHCA decreased the mortality and improved the odds of good neurological outcome, even when including patients with non-shockable rhythms, more lenient downtimes, unwitnessed arrest and/or persistent shock.43 Another systematic review showed a beneficial effect of hypothermia in shockable rhythms only.44 However, in the IHCA setting, use of therapeutic hypothermia compared with usual care was associated with a lower likelihood of survival to hospital discharge and a lower likelihood of favorable neurological survival.45 On the other hand, the benefit of targeted temperature management (TTM) with therapeutic hypothermia has been assessed in a systematic review and meta-analysis with pooled data of five randomized controlled trials with 1389 patients, and no differences in mortality or neurological outcomes were found.46 The authors concluded that employing therapeutic hypothermia as a standard of care strategy of post-arrest care in survivors may need to be reevaluated.
The present study is observational in nature and, as such, is subject to limitations including selection bias as patients with cardiac arrest are attended on site and those not recovering do not reach the hospital, and information bias, particularly regarding difficulties of exact recording of derived times and intervals. The potential effect of confounding variables was addressed by the use of logistic regression analysis. Neurological outcome at follow-up especially at 12 months is limited by the number of losses to follow-up with findings at risk of attrition bias. Also, data on decisions about limitation of life support were not recorded, neither the number of patients who were organ donors and, in this case, if they were in asystole.
In summary, we here report clinically relevant data of the first national registry of patients recovering from cardiac arrest admitted to Spanish ICUs. This information is clinically pertinent and useful since contributes to a better knowledge of the epidemiology, post-resuscitation management, and neurological outcome of patients having cardiac arrest. Salient findings include a similar rate of OHCA and IHCA and a percentage of bystanders lower than 50%, with age, non-cardiac cause of arrest, ROSC >20min, and total CPR as significant predictors of ICU mortality. The most favorable prognosis regarding neurological function was obtained in the presence of shockable rhythm, ROSC <20min, and cardiac cause of the arrest. Data of the neurological sequela measured with the Barthel index after 12 months of the event, with a fully independent rate of 22% is clinically relevant and has not been previously reported.
Contributions of authorsA. Loza: study design, writing of the study protocol and submission to the Institutional Review Board, review of individual patients’ case report forms, data analysis and interpretation, results interpretation, literature search, writing of the manuscript, and approval of the final version.
F. del Nogal: study design, data analysis and interpretation, writing of the manuscript with important contributions for scientific content, and approval of the final draft.
D. Macias: supervision and coordination of the online registries, review of the manuscript, and approval of the final draft.
C. León, A. Lesmes: writing of research grants, data analysis and interpretation, literature search, writing of the manuscript, and approval of the final draft.
L. Socias, L. Herrera, L. J. Yuste, J. Ferrero, B. Vidal, J. Sánchez: screening, inclusion of the patients in the study and follow-up assessments, data collection, care of the patients, critical review of the manuscript, and approval of the final draft.
Conflict of interestNone declared.
The authors thank Pedro Saavedra, Mathematics Department, Universidad de las Palmas de Gran Canaria, for statistical analysis and interpretation of data and Marta Pulido, MD, for editing the manuscript and editorial assistance.
Andalucía: A. Loza, D. Macías and A. Lesmes (Hospital Universitario de Valme, Sevilla); Luis Martín, A. Bohórquez (Hospital Universitario Virgen del Rocío, Sevilla); J. J. Arias. (Hospital de Jerez de la Frontera, Jerez de Frontera, Cádiz); E. Aguilar (Hospital Comarcal Infanta Margarita, Cabra, Córdoba); O. Rufo (Hospital San Juan de Dios, Sevilla); J.C. Luque (Hospital Comarcal de Antequera, Antequera, Málaga); T. García (Hospital Universitario Carlos Haya, Málaga); and J. C. Robles (Hospital Universitario Reina Sofía, Córdoba). Aragón: I. Ostabal, A.L. Ruiz and J.L. Ibáñez (Hospital Universitario Miguel Servet, Zaragoza); E. Civiera (Hospital Lozano Blesa, Zaragoza); and P. Laguardia (Hospital Royo illanova, Zaragoza). Canarias: A.E. Trujillo (Hospital General de La Palma, La Palma). Castilla la Mancha: V. Córcoles (Hospital Universitario de Albacete, Albacete); L. J. Yuste (Hospital General Universitario de Ciudad Real, Ciudad Real); A. Zabalegui and S. Ossa (Hospital Universitario de Burgos, Burgos); V. Fraile, A. González and J. Sánchez (Hospital Universitario Río Hortega, Valladolid); O. López (Hospital de Soria, Soria); and M. R. Truchero (Hospital de Ávila, Ávila). Catalunya: B. Sánchez and R. Algarte (Hospital Universitari Mútua Terrassa, Terrassa, Barcelona); A. Fernández (Parc Sanitari Sant Joan de Déu, Barcelona); and J.C. López (Hospital Universitari de Bellvitge, L’Hospitalet de Llobregat, Barcelona). Euskadi: J.A. Urturi (Hospital Santiago Apostol, Vitoria); N. Etxebarría and G. Lara (Hospital Universitario de Donostia, Donostia-San Sebastián). Extremadura: F.J. Fuentes (Hospital Universitario de Badajoz, Badajoz). Galicia: V. Gómez and L. Lage (Hospital Universitario de Vigo, Vigo); A. Varela (Hospital Ntra. Sra. de Fátima, Pontevedra); C.J. Fernández (Hospital Arquitecto Marcide, A Coruña); and A.V. Aller (Hospital Universitario A Coruña, A Coruña). Illes Balears: L. Socias (Hospital Son Llàtzer, Palma); R. Fernández-Cid (Hospital Mateu Orfila, Menorca); and M. E. Bartual (Hospital Can Misses, Eivissa). Madrid: M. Cruz (Hospital del Sureste, Madrid); M.C. García (Hospital Infanta Elena, Madrid); J. Ferrero and I. Temprano (Hospital Universitario Fundación Alcorcón, Madrid); J.L. Flordelís (Hospital Universitario Severo Ochoa, Madrid); J.A. Álvarez and A. Lesmes (Hospital Universitario de Getafe, Madrid); A. Blandino (Hospital Ramón y Cajal, Madrid); and M.P. González (Hospital Infanta Sofía, Madrid). Murcia: L. Herrera (Hospital Universitario de Cartagena); C. Palazón (Hospital Universitario Reina Sofía, Murcia); and M.J. Párraga (Hospital General Universitario Morales Meseguer, Murcia). Navarra: J. Roldán (Hospital de Navarra, Pamplona). Valencia: P. Manzano (Hospital de Denia, Alicante); J. Ruiz and B. Vidal (Hospital General Universitari de Castelló, Castelló de la Plana); and C. Anton (Hospital Universitario de la Ribera, Valencia), Spain.
PCRR-HT is the Spanish acronym for Recovered Cardiorespiratory Arrest-Hypothermia; GTCIC-PNRCP is the Spanish acronym for Working Group of Cardiac Intensive Care Units-National Plan of Cardiopulmonary Resuscitation; SEMICYUC is the Spanish acronym for Spanish Society of Intensive Care Medicine and Coronary Units).