In recent years, novel articles on airway management, such as the INTUPROS trial, a multicenter study on the reality of this practice in Intensive Care Medicine Departments across Spain,1 or new clinical practice guidelines on difficult airway (DA2,3 management, have been published.
We would like to present some key concepts in airway management in the Intensive Care setting that, in our opinion, are not adequately covered by the currently available guidelines, which are aimed at patients who will undergo an elective procedure2 and are therefore, not representative of the daily reality of critical patients, exposed to different organ failure scenarios that compromise their physiological reserve.1
Historically, the terms direct laryngoscopy (DL) and orotracheal intubation (OTI) have been considered virtually synonymous. Today, the industry offers a wide range of devices that allow OTI to be performed by other means, which makes knowing the device and having proper training in its use a necessity, because in the hands of untrained personnel, the success rate may be even lower than that achieved with conventional DL.
The DA has traditionally been assessed fundamentally from an anatomical point of view, which is related to the difficulty in visualizing the laryngeal structures by DL according to the Cormack-Lehane classification. In 2015, Monsier et al. introduced the concept of the physiological airway.4 This represents a more precise approach in Intensive Care Medicine for, although all patients have a latent risk of presenting an anatomically difficult airway, organ failure, and an unfavorable clinical context are much more prevalent in our concrete setting. Nevertheless, this improved approach may still be insufficient, and we thus propose the following definitions in three scenarios that combine the above concepts (Table 1):
- -
Emergent DA: Extreme threat for the patients life, in a scenario of imminent or actual cardiac arrest. No delay is possible, and there are associated physiological and contextual difficulties.
- -
Urgent DA : Patients requiring definitive airway isolation through OTI in a short space of time, but in whom it is possible to delay the procedure for several minutes to optimize the context. Although organ failure is present, there is enough time to optimize oxygenation and hemodynamics and for airway evaluation.
- -
Elective DA: The indication for airway isolation is not organ failure. The anatomical risk is always latent, but the clinical context is favorable and the physiology is stable. These are the patients who adhere best to the DA guidelines but are also those least frequently seen in the Intensive Care Unit (ICU).
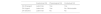
DL remains the most commonly used option, although video laryngoscopy (VDL) is associated with a higher first pass success rate.1,5 In the coming years, it is expected that VDL will displace DL as the technique of choice. However, the technique is often spoken of generically, without distinguishing which type of laryngoscope is used, even though each of the different devices found on the market has its specific characteristics, indications, forms of use, and learning curves. We propose distinguishing the following three families of devices (Table 2):
- -
VDL MAC blade: the technique employed when using this device resembles DL and represents the most organic transition to VDL. Simply put, it may be concluded that any situation where OTI using Macintosh DL is indicated can be approached with a VDL MAC, with the certainty that it will offer at least similar (and probably better) vision and probability of success.
- -
VDL Hyperangulated blade: this VDL facilitates glottic vision and does not require alignment of the oropharyngeal-laryngeal axis; however, progression of the endotracheal tube (ETT) through the chordae imay be difficult It improves OTI in a DA scenario but might make it more difficult when approaching an anatomically normal airway.
- -
VDL Channel: This type of device consists of an angled blade similar to the above, but, in addition, comes with a channel that helps direct the ETT. Even though the ETT might be easier to direct and advance, combining the device with accessories (bougies, suction tube, etc.) can be difficult, and a minimum mouth opening of 1.5−2 cm is required.
Proposed classification for videolaryngoscope (VDL) families.
| VDL MAC | Hyperangulated VDL | VDL with channel | |
|---|---|---|---|
| Commercial examples | McGrath Mac®C-MAC Mac®Glidescope MAC®i-View® | McGrath X-Blade®C-MAC D-Blade®Glidescope LoPro® | Airtraq®KingVision® with channelPentax AWS® |
| Indication | First choice | Expected or known anatomically difficult airway | Expected or known anatomically difficult airway |
| Technique | Similar to DLSuitable also for DL | Modified laryngoscopyIntroduction by midlineSagittal plane rotation | Specific techniqueIntroduction by midlineUpward tractionCoronal plane rotation |
| Advantages | Useful in space conflict (macroglossia, microstomia, etc.)Easy to combine with bougies, fiberscope or suction cannulas | Full visualization of the glottisNo axial alignment requiredEasy to combine with bougies, fiberscope or suction cannulas | Full visualization of the glottisNo axial alignment requiredThe ETT is inserted alongside the blade. |
| Inconveniences | Requires some degree of axial alignment | Difficulty in advancing the ETT | More difficult to combineMinimal mouth opening (1.5−2 cm) |
Although recommended as a salvage option in failed airway,2,3 supraglottic devices (SGDs) are only rarely used in daily ICU practice,1 due either to lack of practice or to lack of an after plan once placed. If a compatible device has been chosen, it is possible to intubate using fibroscopy through the SGD. For those who do not have sufficient expertise for such a technique, the SGD provides stability and time to organize the next step toward a definitive airway isolation method.
Even though, in the operating room, the gold standard in patients with known or predicted DA is awake OTI with fibroscopy2 and that DA in the ICU is 55 times more frequent than in the operating room,7 the use of fibroscopy in the ICU is exceptional.1 In the critically ill patient, the difficulty is usually contextual and physiological, not exclusively anatomical, so this recommendation is not generally applicable in routine practice. Nevertheless, under appropriately selected conditions, the fiberscope can be very useful:
- -
Elective OTI in known or anatomically suspected DA. Isolated airway involvement in an otherwise stable patient, with a favorable context that allows it to be considered.
- -
Definitive isolation of the airway from an SGD.
- -
A combined technique with a VDL in particularly complex cases.
Finally, it is worth mentioning the often underestimated relevance of basic yet crucial aspects, such as position optimization, airway pharmacology or human team coordination, among others.3,6,8
In conclusion, there are several points where the DA guidelines and clinical practice are not properly adjusted. On one hand, it may be necessary to critically review our training and performance in this regard. On the other hand, the guidelines themselves could likely be better adapted to the reality of critically ill patients, taking into account their particularities. We believe it is necessary to look for a new approach adapted to critically ill patients, combining the experience of DA management in the operating room with the context and physiological impairments inherent to critical care, both for the training of residents and for the development of specific clinical practice guidelines for DA in the critically ill patient.
CRediT authorship contribution statementAll the authors have actively participated in the literature search, drafting of the manuscript, and correction of the different versions.