To know the real clinical practice of Spanish ICUs in relation to analgesia, sedation and delirium, with a view to assessing adherence to current recommendations.
DesignA descriptive cross-sectional study was carried out based on a national survey on analgesia, sedation and delirium practices in patients admitted to intensive care on 16 November, 2013 and 16 October, 2014. An on-line questionnaire was sent with the endorsement of the SEMICYUC.
SettingSpanish ICUs in public and private hospitals.
ResultsA total of 166 ICUs participated, with the inclusion of 1567 patients. The results showed that 61.4% of the ICUs had a sedation protocol, and 75% regularly monitored sedation and agitation – the RASS being the most frequently used scale. Pain was monitored in about half of the ICUs, but the behavioral scales were very little used. Delirium monitoring was implemented in few ICUs. Among the patients on mechanical ventilation, midazolam remained a very commonly used agent.
ConclusionsThis survey is the first conducted in Spain on the practices of analgesia, sedation and delirium. We identified specific targets for quality improvement, particularly concerning the management of sedation and the assessment of delirium.
Conocer la práctica clínica real de las UCI españolas en relación con la analgosedación y delirium, y valorar cómo se ajusta a las recomendaciones actuales.
DiseñoEstudio transversal descriptivo elaborado mediante encuesta nacional sobre prácticas de analgosedación y delirium de los pacientes ingresados en UCI los días 16 de noviembre de 2013 y 16 de octubre de 2014. Se envió un cuestionario a través de Internet con el aval de la SEMICYUC.
ÁmbitoUCI tanto públicas como privadas de todo el territorio nacional.
ResultadosSe incluyeron un total de 166 UCI y a 1.567 pacientes. El 61,4% de las UCI contaban con un protocolo de sedación. El 75% de las UCI monitorizaban la sedación y agitación, con RASS como la escala empleada con mayor frecuencia. El dolor se monitorizaba en algo más de la mitad de las UCI, pero las escalas conductuales eran de muy baja implantación. El delirium también presentaba un bajo nivel diagnóstico. Entre los pacientes en ventilación mecánica el midazolam continuaba siendo un sedante de muy amplio uso.
ConclusionesEsta encuesta es la primera realizada en España sobre analgosedación y delirium y nos muestra una fotografía sobre estas prácticas, señala algunos aspectos como los relacionados con la monitorización y usos de escalas, junto con el manejo del delirium, en los que los resultados del estudio animan a desarrollar proyectos docentes que acerquen la práctica clínica real a las recomendaciones nacionales e internacionales.
Management of pain, sedation, agitation and delirium is one of the most important aspects in the management of critically ill patients and it can condition their clinical prognosis. There is a growing number of studies that highlight the existing mid-term and long-term consequences of the non-optimal management of these aspects. Events like cognitive disorders, memory loss, or sleep disorders can occur in these patients and in most cases, it is difficult for them to get back to normal.1–3
Back in 2008, the SEMICYUC Sedation and Analgesia Working Group published an article including a wide variety of recommendations about monitoring and sedation management, analgesia and neuromuscular blockade in critically ill patients that was the result of a significant effort made by all of its members and to this day it is still a basic document on this regard when it comes to our patients.
Based on the actual studies and clinical practice, the clinical guidelines give a number of basic recommendations, such as keeping the patient pain-free using the analgesia that is most suitable for each case, indicating minimal sedation—provided there are not contraindications—and implementing the right tools to detect and prevent delirium.4–6 These recommendations have unequal follow-up in the different ICUs depending on different factors.
Pain is one of the most traumatic experiences among Intensive Care Unit (ICU) patients and it is the one they remember with the highest levels of stress and frequency once they have been discharged.7 Following the basic recommendations, the management of pain includes proper prevention, monitoring and treatment. Unnecessary nociceptive stimuli should be avoided, preventive analgesia should be administered, and pain scales should be used both with cooperative and uncooperative patients and the adequate multimodal analgesia should be guaranteed here, based on opiates, non-opiate drugs, locoregional analgesia techniques and non-pharmacological techniques.8,9
Sedation and agitation in UCI patients require multidisciplinary approach and protocolization, proper monitoring and shared collective awareness, both from the medical team and the nurse personnel.9 Reducing sedation, with the development of strategies that promote minimal sedation and the use of scales validated for their monitoring are basic pillars in today's management of critically ill patients.10,11 In that sense, today's guidelines recommend pharmacological and non-pharmacological strategies avoiding the use of benzodiazepines and promoting agents such as propofol or dexmedetomidine in an effort to improve the clinical result of the critically ill patient, minimize mechanical ventilation, or the probability of developing delirium.4–6
Delirium is a serious complication of critically ill patients, with an incidence rate of 80% in patients on mechanical ventilation. Several studies today speak of its negative impact, both in the short and the long run in ICU patients and still many others reveal that this factor is associated with cognitive dysfunction, long ICU stays and more mortality.12 The first difficulty is detecting the condition and to this end tools such as the Confusion Assessment Method for Intensive Care Unit (CAM-ICU) or the Intensive Care Screening Delirium Checklist can be used. Detection of delirium allows proper management and specific interventions on the environmental factors that contribute to its development.13
Several neighboring countries have conducted surveys to know about the clinical practice when managing sedation, pain and delirium in critically ill patients in their respective ICUs.14–23 However, to this day, a project of this nature had not been conducted in Spain, which would allow us to know the uses and customs when managing these aspects in critically ill patients.
The goal of this document is to reveal and analyze the results of this nationwide survey on clinical practice regarding sedation, analgesia and delirium in ICUs of Spanish adults and define the aspects that should be improved.
Material and methodAt the 47th National Congress held in Santander back in 2012, the Sedation, Analgesia and Delirium Working Group from the Spanish Society of Intensive and Critical Medicine and Coronary ICUs (SEMICYUC) agreed to conduct a prevalence cut to know the actual sedation, analgesia and management practices of delirium in Spanish ICUs.
In order to be able to participate in this study, an email was sent to directors of ICUs nationwide, both public and private ICUs. The SEMICYUC census made it possible. Back in 2013, this was called SEDAN-UCI (prevalence cut of sedation and analgesia at ICUs) and in the 2014 edition it was called ENVAS (national study on analgesia and sedation monitoring) by analogy with ENVIN (national study on nosocomial infection monitoring) conducted by SEMICYUC Working Group of Infectious Diseases and Sepsis (GTEIS).
This document only includes data of adult patients hospitalized at Spanish ICUs. The participation had 2 stages. The first, in the form of a questionnaire about the characteristics of the unit in terms of the number of beds, the existence of a sedation reference, sedation, and pain scales used, etc. (Annex I). The second stage included a study on the prevalence of sedation and analgesia practices of the patients admitted to the ICU. Back in 2013, the dates chosen were November 16, 2013, and in 2014, October 16: the sedation and analgesia practices were obtained for 24 hours from 8 AM that same day through 8 AM the next day.
The study was approved by the Clinical Research Committee of the Virgen Macarena Hospital in Seville. Given its observational nature, the committee though that the study did not need to obtain any informed consent documents.
Quantitative variables are expressed as measures of central tendency and dispersion, median and interquartile range (median, IQR) and categorical or qualitative variables as frequency of occurrence and associated percentage (n, %). All analyses were conducted using the SPSS v15.00 statistical package (Chicago, Illinois, United States).
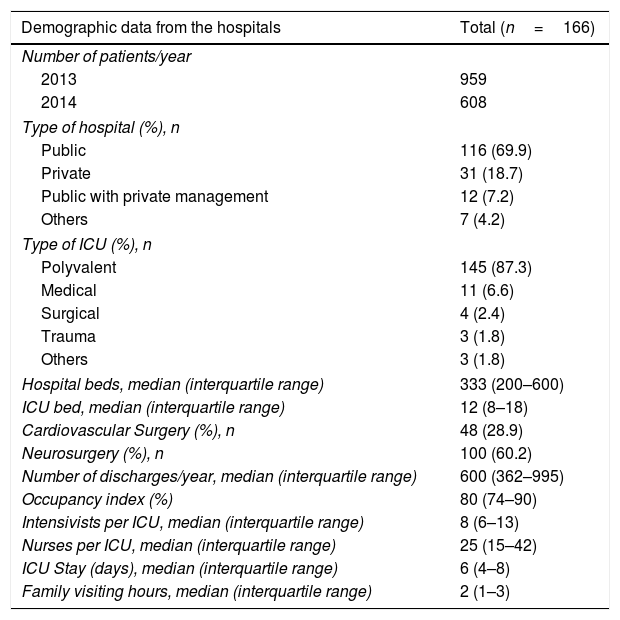
ResultsA total of 166 Spanish ICUs participated in the 2013 or 2014 survey. All the autonomous communities were represented, except for La Rioja, Ceuta and Melilla, with larger representations from the communities of Madrid, Cataluña, and Valencia. We should mention here that there was a majority of public hospitals (69.9%) and that 87% of the ICUs were polyvalent ICUs, with a bed median of 12 (8–18) and 8 intensivists per unit.6–13 The characteristics of the participating hospitals are shown in Table 1.
Results from the hospitals.
| Demographic data from the hospitals | Total (n=166) |
|---|---|
| Number of patients/year | |
| 2013 | 959 |
| 2014 | 608 |
| Type of hospital (%), n | |
| Public | 116 (69.9) |
| Private | 31 (18.7) |
| Public with private management | 12 (7.2) |
| Others | 7 (4.2) |
| Type of ICU (%), n | |
| Polyvalent | 145 (87.3) |
| Medical | 11 (6.6) |
| Surgical | 4 (2.4) |
| Trauma | 3 (1.8) |
| Others | 3 (1.8) |
| Hospital beds, median (interquartile range) | 333 (200–600) |
| ICU bed, median (interquartile range) | 12 (8–18) |
| Cardiovascular Surgery (%), n | 48 (28.9) |
| Neurosurgery (%), n | 100 (60.2) |
| Number of discharges/year, median (interquartile range) | 600 (362–995) |
| Occupancy index (%) | 80 (74–90) |
| Intensivists per ICU, median (interquartile range) | 8 (6–13) |
| Nurses per ICU, median (interquartile range) | 25 (15–42) |
| ICU Stay (days), median (interquartile range) | 6 (4–8) |
| Family visiting hours, median (interquartile range) | 2 (1–3) |
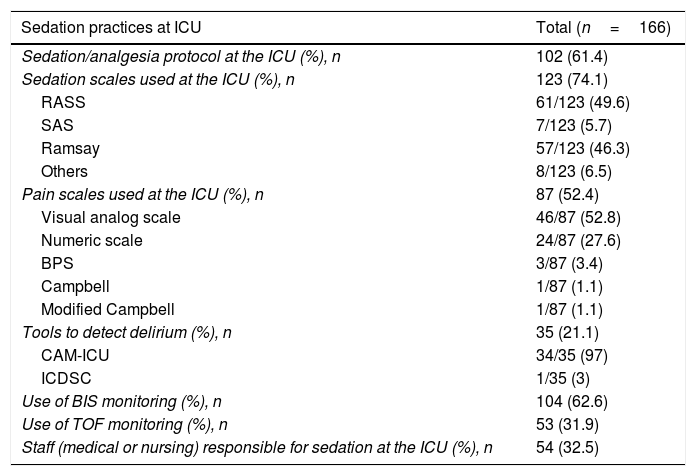
With respect to analgosedation and delirium practices (Table 2), we should also mention that 102 ICUs (61.4%) had a protocol available that regulated this practice and 54 ICUs (32.5%) had (medical or nursing) staff responsible for such practice. On the use of the scales, almost 75% of the ICUs monitored sedation; the scale most commonly used was the Richmond Agitation-Sedation Scale (RASS) (49% of the ICUs). Regarding pain, little more than 50% of the ICUs monitored pain: the most commonly used scales were the verbal numerical rating scale or the analog scale (VNRS, VAS) in 80% of the cases; however, behavioral scales such as the BPS or the Campbell scale are hardly ever implemented, only in 5.5% of the ICUs.
Sedation practices.
| Sedation practices at ICU | Total (n=166) |
|---|---|
| Sedation/analgesia protocol at the ICU (%), n | 102 (61.4) |
| Sedation scales used at the ICU (%), n | 123 (74.1) |
| RASS | 61/123 (49.6) |
| SAS | 7/123 (5.7) |
| Ramsay | 57/123 (46.3) |
| Others | 8/123 (6.5) |
| Pain scales used at the ICU (%), n | 87 (52.4) |
| Visual analog scale | 46/87 (52.8) |
| Numeric scale | 24/87 (27.6) |
| BPS | 3/87 (3.4) |
| Campbell | 1/87 (1.1) |
| Modified Campbell | 1/87 (1.1) |
| Tools to detect delirium (%), n | 35 (21.1) |
| CAM-ICU | 34/35 (97) |
| ICDSC | 1/35 (3) |
| Use of BIS monitoring (%), n | 104 (62.6) |
| Use of TOF monitoring (%), n | 53 (31.9) |
| Staff (medical or nursing) responsible for sedation at the ICU (%), n | 54 (32.5) |
In the survey only 35 ICUs, 21% of all the ICUs, monitored delirium: the most commonly used tool was the CAM-ICU (97% of the cases).
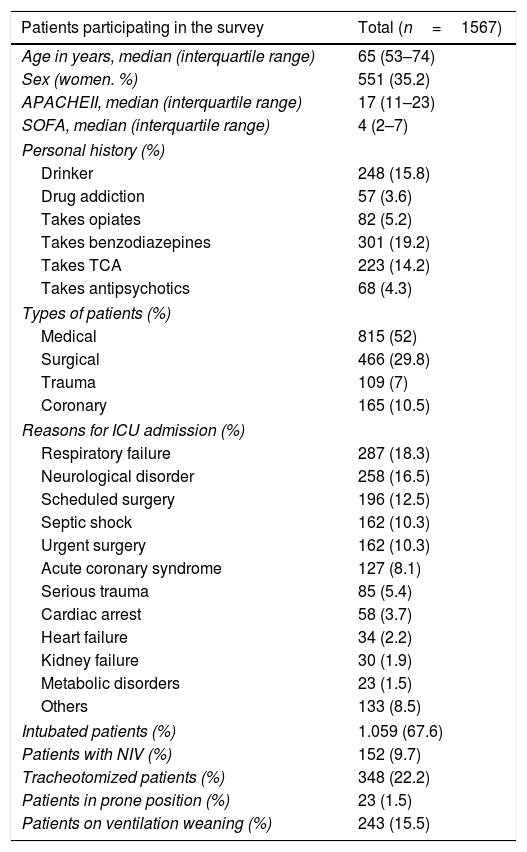
Regarding patients, 1567 were included in the study, 959 in 2013 and 608 in 2014 (Table 3). Among their basic characteristics, these should be highlighted: age, with an average of 65 years, APACHE II score of 17 (ad admission) and SOFA score of 4. When it comes to the personal history these were the main characteristics: being a drinker (15.8%), using benzodiazepines (19.2%), antidepressants (14.2%), antipsychotics (4.3%), or opiates (5.2%), and drug addiction (3.6%).
The patients’ characteristics.
| Patients participating in the survey | Total (n=1567) |
|---|---|
| Age in years, median (interquartile range) | 65 (53–74) |
| Sex (women. %) | 551 (35.2) |
| APACHEII, median (interquartile range) | 17 (11–23) |
| SOFA, median (interquartile range) | 4 (2–7) |
| Personal history (%) | |
| Drinker | 248 (15.8) |
| Drug addiction | 57 (3.6) |
| Takes opiates | 82 (5.2) |
| Takes benzodiazepines | 301 (19.2) |
| Takes TCA | 223 (14.2) |
| Takes antipsychotics | 68 (4.3) |
| Types of patients (%) | |
| Medical | 815 (52) |
| Surgical | 466 (29.8) |
| Trauma | 109 (7) |
| Coronary | 165 (10.5) |
| Reasons for ICU admission (%) | |
| Respiratory failure | 287 (18.3) |
| Neurological disorder | 258 (16.5) |
| Scheduled surgery | 196 (12.5) |
| Septic shock | 162 (10.3) |
| Urgent surgery | 162 (10.3) |
| Acute coronary syndrome | 127 (8.1) |
| Serious trauma | 85 (5.4) |
| Cardiac arrest | 58 (3.7) |
| Heart failure | 34 (2.2) |
| Kidney failure | 30 (1.9) |
| Metabolic disorders | 23 (1.5) |
| Others | 133 (8.5) |
| Intubated patients (%) | 1.059 (67.6) |
| Patients with NIV (%) | 152 (9.7) |
| Tracheotomized patients (%) | 348 (22.2) |
| Patients in prone position (%) | 23 (1.5) |
| Patients on ventilation weaning (%) | 243 (15.5) |
These were some of the reasons for ICU admission: 18.3% of the cases due to respiratory failure, 16.5% due to neurological causes, and 12.5% were admitted due to a scheduled surgery.
Of the overall number of patients, 1059 (67.6%) were intubated on the day of the study, 243 patients were on mechanical ventilator weaning (15.5%), and 152 on non-invasive ventilation (9.7%).
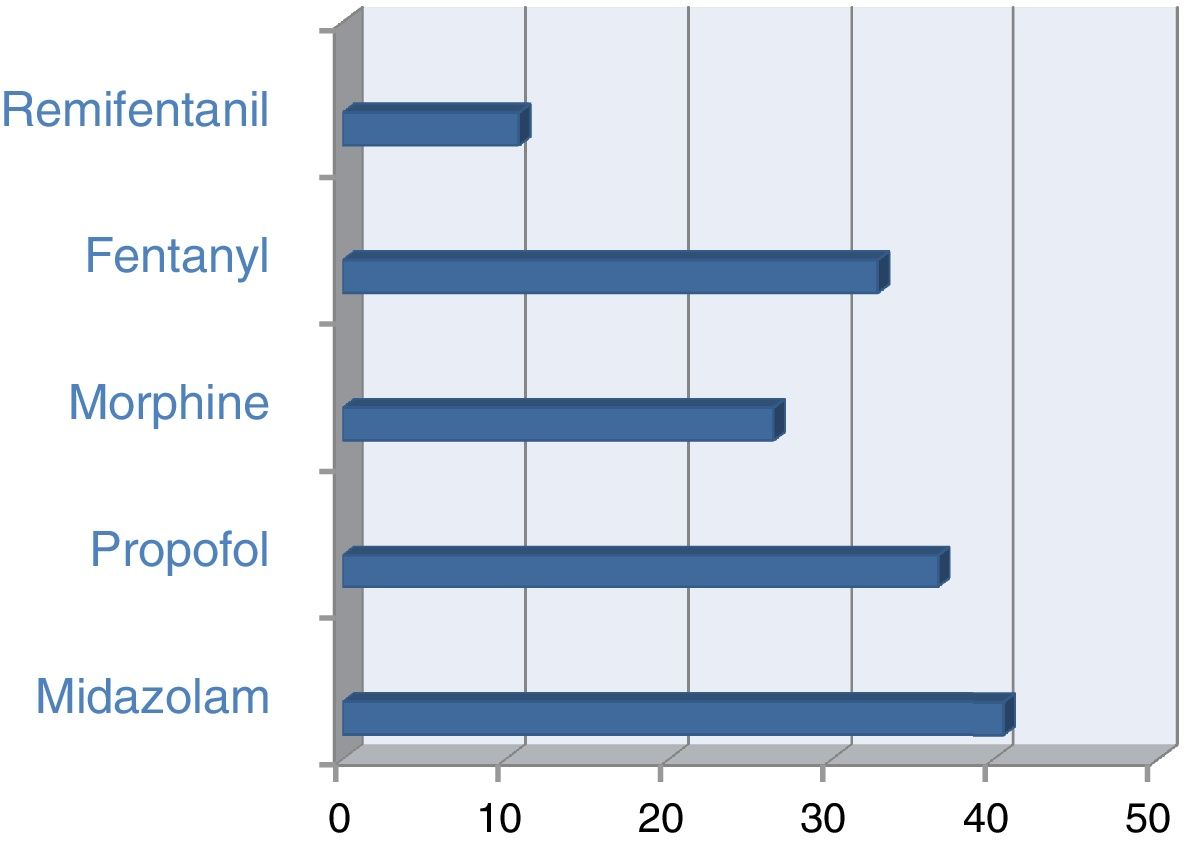
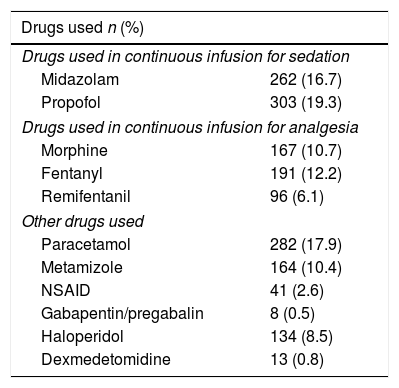
If we take a look at analgosedation relaxation (Table 4), we should emphasize that, overall, the most commonly used sedatives were midazolam in 16.7% of the cases and propofol in 19.3%, and, among analgesics, morphine in 10.7%, fentanyl in 12.2% and remifentanil in 6.1%. When it comes to other drugs, paracetamol was used almost in 18% of the patients and metamizole in 10%. The combination of these drugs was of common use.
Drugs used.
| Drugs used n (%) | |
|---|---|
| Drugs used in continuous infusion for sedation | |
| Midazolam | 262 (16.7) |
| Propofol | 303 (19.3) |
| Drugs used in continuous infusion for analgesia | |
| Morphine | 167 (10.7) |
| Fentanyl | 191 (12.2) |
| Remifentanil | 96 (6.1) |
| Other drugs used | |
| Paracetamol | 282 (17.9) |
| Metamizole | 164 (10.4) |
| NSAID | 41 (2.6) |
| Gabapentin/pregabalin | 8 (0.5) |
| Haloperidol | 134 (8.5) |
| Dexmedetomidine | 13 (0.8) |
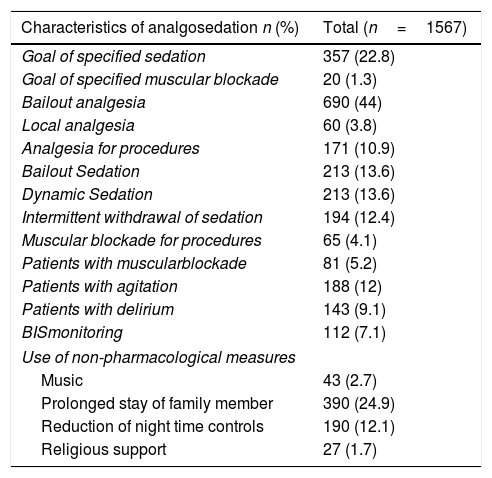
The goal of sedation was only specified in 22.8% of these patients and bailout sedation was only prescribed in 13.6% (Table 5). When it comes to analgesia, it was determined that opiates were used in less than 30% of the patients; however, bailout analgesia is considered in 44% of the cases and the use of specific analgesia for procedures is only used in 10.9% of the patients. Locoregional analgesia is a marginal procedure, used in 3.8% of the cases. Neuromuscular blockade was used in 81 patients, 5.2% of the overall number of patients. The level of blockade was specified in one fourth of the cases only.
Characteristics of analgosedation.
| Characteristics of analgosedation n (%) | Total (n=1567) |
|---|---|
| Goal of specified sedation | 357 (22.8) |
| Goal of specified muscular blockade | 20 (1.3) |
| Bailout analgesia | 690 (44) |
| Local analgesia | 60 (3.8) |
| Analgesia for procedures | 171 (10.9) |
| Bailout Sedation | 213 (13.6) |
| Dynamic Sedation | 213 (13.6) |
| Intermittent withdrawal of sedation | 194 (12.4) |
| Muscular blockade for procedures | 65 (4.1) |
| Patients with muscularblockade | 81 (5.2) |
| Patients with agitation | 188 (12) |
| Patients with delirium | 143 (9.1) |
| BISmonitoring | 112 (7.1) |
| Use of non-pharmacological measures | |
| Music | 43 (2.7) |
| Prolonged stay of family member | 390 (24.9) |
| Reduction of night time controls | 190 (12.1) |
| Religious support | 27 (1.7) |
When it comes to the use of practices to optimize the sedation of patients (Table 5), we saw that BIS monitoring for deep sedation or neuromuscular blockade was used in 112 patients, 7.1% of the cases; dynamic sedation in 13.6% and the daily withdrawal of sedation in 12.4%.
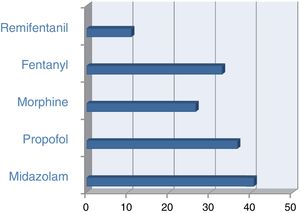
These were the data for the group of patients on invasive mechanical ventilation with sedatives: 40.6% were on midazolam and 36.5% on Propofol. These are the figures for analgesics: 26.4% of ventilated patients were on morphine and 32.8% on fentanyl (Fig. 1). Among the patients with neuromuscular blockade, 85.2% of them were on midazolam and 38.3% on propofol; a little over 20% were using both sedatives simultaneously and almost 99% of had been prescribed some type of opiate. In these patients, BIS monitoring was used in 43.2% of the cases. In patients on non-invasive ventilation, analgesia with opiates was used in 45.3% of the cases.
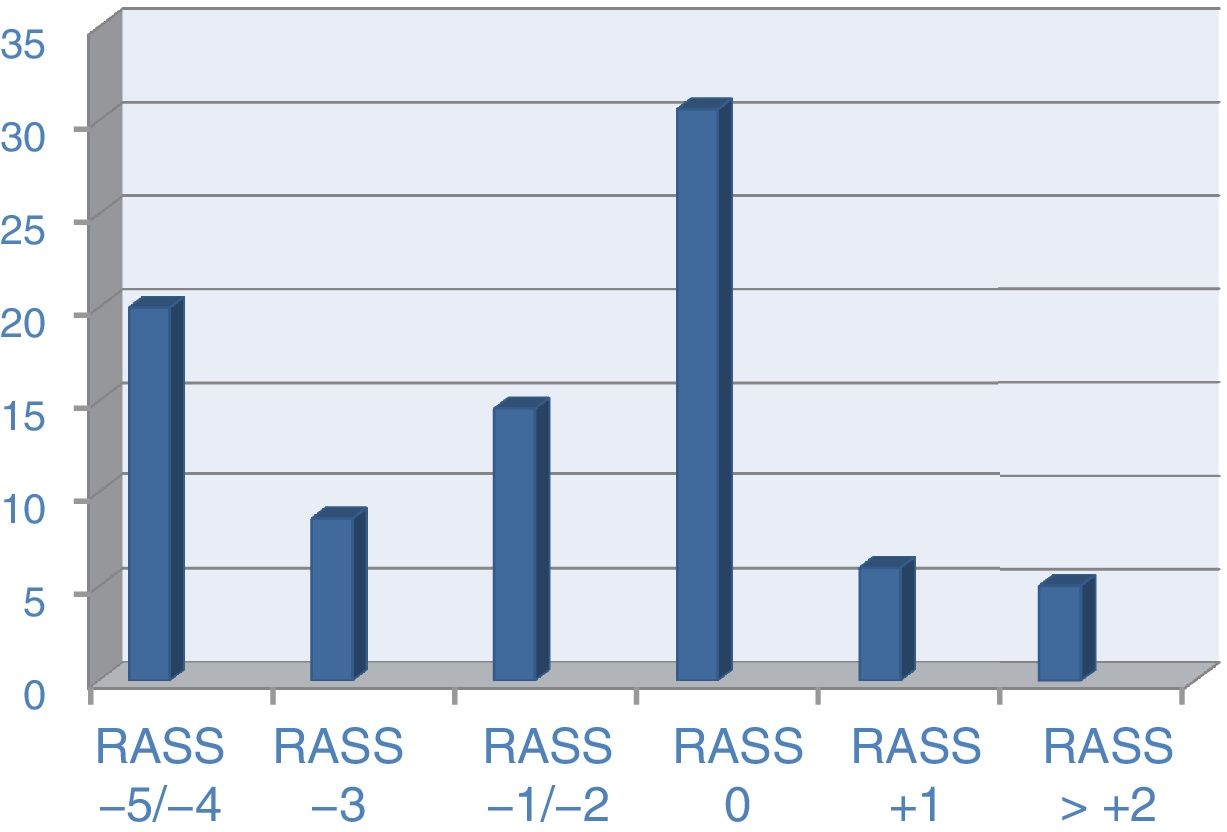
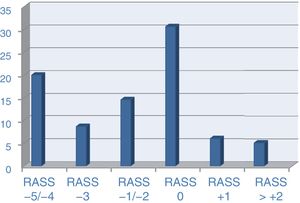
The RASS scale was used as a reference to assess the level of sedation on that day. In the specific group of patients on invasive mechanical ventilation, the RASS scale was recorded in 899 cases (84.9% of ventilated patients) with the following levels of sedation: RASS of 5 in 10.8% of the cases, RASS of 4 in 12.7%, RASS of 3 in 10.1%, RASS of 2 in 7.6%, RASS of −1 in 9.7%, RASS of 0 in 36%, RASS of +1 in 7.1%, RASS of +2 in 4%, and beyond this point, in around 1% of the cases (Fig. 2).
When it comes to delirium, we find that 12% of the patients had shown agitation during the previous 24 hours (Table 5), and 9.1% (143 patients) showed delirium, diagnosed by the CAM-ICU in almost 81% of the cases. On this regard, haloperidol was used in 8.5% (134) of the patients being the use of dexmedetomidine incidental below 1%.
When it comes to non-pharmacological measures (Table 5), we asked on the use of music, TV and the press that was considered in 2.7% of the patients only. Other measures were the relative staying, used in 24.9% of the cases, and less night controls in 12.1%. During these moments the median of visiting hours from relatives was 2.
We should consider some incidents where this aspect of the patient may be involved. Among them we find accidental extubations that occurred in just 0.5% of the cases, and withdrawal of probes or catheters in 2.2% of the patients. Mechanical fasteners were used in 14.2% of all patients, a percentage that remains in similar figures (14.8%) in patients on invasive ventilation. Accidental falls occurred in 0.2% of the cases.
DiscussionFirst and foremost, this has been the very first survey ever conducted nationwide with the participation of a large number of adult ICUs, both public and private, to find out about analgosedation and neuromuscular blockade practices among critically ill patients. Also, this is the first step to know what degree of correlation these practices keep with the practice approved by the actual standards, recommendations and clinical practice guidelines.4–6
These results show a rather representative picture of the clinical practice when the survey was conducted represented in a nationwide sample of ICUs, including all levels of healthcare, with a wide range of beds per ICU and hospital. We should point out that almost 70% of the hospitals that responded to the survey were public centers.
When data on analgosedation practices were analyzed, we saw that over 50% of the ICUs have a protocol available that regulates these practices. However, few ICUs have their own (medical or nursing) specific staff on this field to contribute more specific knowledge in complex cases.24 If this practice is analyzed in neighboring countries, we will see that this percentage is a little higher compared to countries like the UK, France or Poland;14,15,18 however, we are still far from the level of protocols the United States has (according to a worldwide survey, 83%).17
If we focus on specific aspects, we can see that almost 75% of the ICUs monitor their patients’ sedation. This is a basic, crucial aspect when managing analgosedation8,24 and, although the percentage can be considered high, there is still a lot of room for improvement that would suggest making an effort to monitor sedation in all of our patients. If we do not monitor, it is difficult to avoid issues like oversedation that can be dangerous for our patients.25 When it comes to the use of scales, the RASS is the most commonly used sedation scale, however, we should say that other scales such as the Ramsay scale are still widely used. If we take a look at our neighboring countries, we will find a similar pattern with an extensive use of the RASS scale,14,15,18 together with the Ramsay scale though. Regarding these practices, both the United States and Nordic countries use the RASS scale consistently.16,17 To this day, the use of the RASS scale is becoming more generalized.26 Added to this is how easy it is to use, with positive values for agitation states and negative values for sedation states.
When it comes to pain, the basic priority issue in the management of ICU patients27,28 and the one issue that many of these patients remember as one of the most negative memories of their ICU stay, a little over 50% of all ICUs monitor pain. This is indicative that in many cases the assessment of this basic aspect of our patients’ care is still seen as something marginal, yet despite the fact that in all clinical guidelines it is considered as the first step to achieve comfort and wellbeing in our critically ill patients. Today there are many publications that reveal the negative consequences that the inadequate pain management has in ICU patients.29 Pain is not only involved in the appearance of chronic pain, but also non-treated pain contributes to the appearance of delirium, depression, anxiety, fear and, ultimately, to the appearance of post-traumatic stress disorders. Also, pain is involved in an higher response to stress that can contribute to states of hyperglycemia, mechanical ventilation asynchrony, or sleep alterations, among other consequences.29,30
When analyzing the type of patients, it is with cooperative patients, with the use of VAS and VNRS scales, that the assessment of pain is performed more often, while with uncooperative patients, behavioral scales such as the ESCID, the BPS or the Campbell scale are practically marginal, indicative of the almost null pain assessment in these patients. In our neighboring countries, the assessment of pain is far more advanced than ours. In countries like France, in communicative patients pain is assessed in almost 70% of these patients, while in non-communicative patients, it is assessed in up to 30%15; In Germany, assessment levels are close to 80%, and in the United States, the levels of pain assessment are even higher.21 Today, the use of the ESCID scale is becoming more popular to monitor the pain of non-cooperative patients. Also, the validation of this scale in both medical and surgical patients as been of great help for these monitoring purposes.31
When it comes to delirium, the data indicate that monitoring was even scarcer than in the case of pain: a little over 30 ICUs used tools to detect it. It seems that at that time this complication was still a marginal issue of our routine clinical practice: perhaps delirium was still considered as an effect of little clinical repercussion in the short- or mid-term, even though many studies show the contrary these days: how delirium is involved in increased ICU or hospitals or how much difficult it makes the mechanical ventilation weaning. In sum, delirium leads to more morbimortality in the ICU patient.32,33 Both in our country and in our neighboring countries, the CAM-ICU scale is the most commonly used one for the detection of delirium,34 however, as it happens with pain, we are far from the monitoring levels reached by the UK, for example where almost 70% of ICU can detect it.14,20
Only in over 22% of the patients the goal of sedation is specified in the treatment while in the remaining cases, despite the use of sedatives, the level of sedation wanted is never specified: this is still a more marginal issue in critical patient care.24 Compared to other countries, we can see that we are still far from their level of accomplishment. Thus, in Great Britain the goal of sedation is shown in 42% of the patients in their daily rounds.14,20 When it comes to analgesia practices, bailout analgesia is guidelined in less than half the patients and analgesia for procedures in 10% of patients. These data are indicative that there is still room for improvement in this essential aspect of the critical patient.27,28 The use of locoregional analgesia is still marginal in most of our ICUs.
Regarding practices to optimize analgosedation, the BIS monitoring was used in cases of deep sedation or neuromuscular blockade in 112 patients (29%). Among them, 35 patients were on blockade (43% of the patients blockaded). Other practices, such as dynamic sedation, in 13% of the patients or intermittent withdrawal, in 12% continue to be practices that have not yet been fully implemented in Spanish ICUs.35
With these results we should think that, when this survey was conducted, the use of benzodiazepines like midazolam as a sedative occurs in a high percentage of patients on mechanical ventilation. Similarly, although the use of opiates reaches a high percentage of patients, 30% of them do not use them, which goes against the actual guidelines that recommend the use of opiate-type analgesics as the first therapeutic step.4–6 Once again we can see how the management of pain is a marginal issue in most ICU patients.7,11,27,28 In our neighboring countries, the widespread use of benzodiazepines is a reality. Thus, most French intensivists use midazolam in over 75% of their patients.15 In Poland, benzodiazepines are used for sedation for over 24 hours in more than 90% of the cases.18 On the contrary, in countries like Great Britain, propofol is the most widely used agent (98% of the cases),14,20 or in the Nordic countries, the same thing happens in almost 80% of the cases.16
When speaking about sedation, we should talk about how the patients were the day of the survey, taking the RASS scale as the reference scale, since it was the scale chosen for assessment that day and not the one typically used by the hospital. Among the 1567 patients who participated in the survey, in 330 this information was not completed (21.1% of the total). We should emphasize that out of those who completed the data we find RASS=0 in 49% of the patients and 22% of the cases with superficial sedation (RASS of −1/−3). When analyzing these data, we should say that almost 70% of the patients had a proper level of sedation the day the survey was conducted and according to the actual, guidelines and standards.10,11 Nevertheless, this fact initially opposes the widespread use of midazolam type of agents or the scarce implementation when it comes to specifying the daily goal of sedation for the patients.
To conclude, we should say something about the issue of family visiting hours.36,37 At this moment, when expanding ICU visiting hours is seen as a way of keeping a closer family contact and thus, as a way of keeping patients’ orientated and as a way of reducing the risk of delirium, we should say that the average ICU stays were 2 hours. A survey where intensivists from the European Society of Intensive Medicine and other international societies participated revealed that 64% of European ICUs have less than 5 visiting hours a day, being the percentage of 24 hour-open doors in ICUs in Europe close to 19% as opposed to 82% in the United States.17 With regard to the other non-pharmacological measures, they showed a small rate of implementation when the survey was conducted. Interventions like music therapy, reduction of night time controls, or religious support are practices that are not widely used in our ICUs at this time – similar data to the data found in other sedation surveys conducted such as in Poland,18 where over 55% of intensivists do not use non-pharmacological measures in connection with delirium. Worldwide,17 these measures also have low implementation rates: interventions to favor sleep such as dimming the lights or the night time noise hardly make it to a 24% implementation rate.
As to the limitations, first we report the most important one is the time elapsed since the survey was conducted, which can be suggestive that, at the present time, some of the practices we made questions about have changed. However, this same fact should make us conduct new surveys to confirm whether this change has indeed occurred, and we are actually complying more with the actual guidelines and standards. Secondly, we report that this type of surveys is usually answered by the ICUs that are most interested in this aspect of critically ill patients, meaning that the results should not be extrapolated to all ICUs.
The Americans have recently published the new guidelines37 on the management of sedation, analgesia and delirium, and among other novelties, they speak about the management of sleep alterations and immobility, two aspects that are considered basic when it comes to critical patient comfort and wellbeing, in addition to being closely connected with situations such as PTSD or delirium. These guidelines continue to highlight the importance of assessing pain and delirium, as well as keeping the patient under mild sedation, in the absence of contraindications, and avoiding the use of benzodiazepines.
To conclude, we must say that this survey is the first of its kind ever conducted in Spain on analgosedation and delirium practices and it paints a picture of these practices, emphasizing some aspects such as those having to do with monitoring and the use of scales together with the management of delirium. The results of this study encourage us to develop educational projects that bring the actual clinical practice to the national and international recommendations.
Authors/collaboratorsE.P.H designed and implemented the online form used for data mining purposes, and conducted the first statistical analyses. M.G.S, J.C.L, I.C.R, C.G-E.V, M.A.R.O, C.P.R, T.M.M, D.E, H.T, C.C.J, and E.P.H developed the study idea and design. M.G.S did the initial draft of the manuscript. All undersigned parties have supervised and approved the final draft of this manuscript.
Conflicts of interestM.G.S declared conflicts of interest with Orion-Pharma y Medtronic. The remaining authors declared no conflicts of interest whatsoever.
First and foremost we wish to thank all those intensivists who collaborated while conducting the surveys. Without them we would not have been able to finish this study (Annex II). We apologize if someone was left out of this list.
We also wish to thank the Orion-Pharma laboratory for contributing to the analysis of study data.
In Annex: additional material related GTSAD members.
Please cite this article as: García-Sánchez M, Caballero-López J, Ceniceros-Rozalén I, Giménez-Esparza Vich C, Romera-Ortega MA, Pardo-Rey C, et al. Prácticas de analgosedación y delirium en Unidades de Cuidados Intensivos españolas: Encuesta 2013-2014. Med Intensiva. 2019;43:225–233.