Critically ill patients on mechanical ventilation (MV) due to several conditions may suffer from cardiac abnormalities during their hospital stay, thus giving rise to different cardiovascular events that, although they do not have symptomatic repercussions, they can have different clinical manifestations: high cardiac maker levels such as cardiac troponin-I (cTn-I), electrocardiographic abnormalities, or repolarization and arrhythmias. The presence of any of these manifestations would explain the higher morbimortality rate shown by different studies.1–3
Critically ill patients with septic shocks can suffer from these events more frequently and it is associated with a higher mortality rate.4 During sepsis an inflammatory response triggers that, through different mechanisms and inflammatory mediators, ends up leading to myocardial dysfunction5,6 that manifests itself as systolic or diastolic dysfunction, impaired cardiac output, inadequate oxygen supply and primary myocardial cell damage.6 For this reason, the high plasma levels of cTn-I found in sepsis may have to do with the appearance of such myocardial dysfunction, be a marker of such dysfunction and, consequently, associate higher mortality rates.7,8
We hereby present one observational prospective cohort study on the appearance of cardiovascular events in critically ill patients on MV with non-coronary acute processes conducted between February 1 and March 15, 2014. During this period, 1713 patients were admitted to the intensive care unit (ICU) but 879 of them were excluded due to heart disease, 294 patients because they did not require MV, and 36 because they stayed at the ICU for less than a day; 194 patients were lost during follow-up, and the sample size included 310 patients. Several variables were recorded such as the demographic data, the prior clinical history, the severity index according to the SAPS 3 and SOFA scoring systems, the appearance of cardiovascular events (arrhythmias, repolarization changes on the ECG in the continuous monitoring, high levels of cTn-I, hospital and ICU stays, in-hospital mortality and 1-year mortality). These variables were recorded since the MV was initiated and up to a maximum of 72h after the MV started. The study was approved by the hospital clinical research ethics committee but the patientś informed consent was not required.
In order to the compare categorical variables, the chi-square test and Fisher's exact test were used. To compare the continuous variables, the Student's t test and the Mann–Whitney test was used depending on whether their distribution was, or not, normal. The comparison among three (3) or more variables was conducted using the ANOVA test or the Kruskal–Wallis test. Similarly, one multivariate model of logistics regression was developed in order to assess the appearance of early cardiovascular events as an independent variable associated with in-hospital mortality. Finally, one annual survival analysis was conducted using the Kaplan–Meyer test. p values <0.05 were considered statistically significant.
Out of the 310 critically ill patients on MV studied, 197 patients (63.5%) were men being their average age 66.9±15.3 years old. Their prior clinical history included hypertension (52.6%), diabetes (27.4%) and obesity (24.5%), SAPS 3 61.5±15.7 and SOFA 7.3±3.4. Fifty-two point two per cent of the patients had medical conditions being the main diagnoses at admission sepsis and septic shock (33.4%) followed by non-cardiac surgical disease (20.3%) and respiratory conditions (20%). The hospital stay was 27.7±23.0 days, and the ICU stay was 13.5±13.0 days, being the duration of MV 10.4±11.4 days. The in-hospital mortality rate was 31.3% and the 1-year hospital mortality rate was 44.8%. Table 1 shows a comparison among the different variables based on the in-hospital mortality rate.
General characteristics of the patients studied based on their progression after hospital discharge.
| Variables analyzed | Patient's progression after hospital discharge | p value | |
|---|---|---|---|
| Dead n=97 | Survivors n=213 | ||
| Age (years), (mean±SD) | 70.5±12.6 | 65.2±16.1 | 0.002 |
| SAPS 3 at admission, (mean±SD) | 65.1±1.0 | 59.8±15.7 | 0.005 |
| Stay at the ICU (days), (mean±SD) | 10.1±9.9 | 15.0±13.8 | 0.002 |
| Hospital stay (days), (mean±SD) | 16.8±17.6 | 32.6±23.4 | <0.001 |
| Sex (%) | |||
| Female | 43.2 | 33.3 | 0.093 |
| Male | 56.7 | 66.7 | – |
| Risk factors | |||
| Arterial hypertension, n (%) | 60 (61.9) | 104 (48.8) | 0.037 |
| Diabetes mellitus, n (%) | 31 (32.0) | 54 (25.4) | 0.270 |
| Smoking, n (%) | 18 (18.8) | 56 (26.3) | 0.195 |
| Dyslipidemia, n (%) | 21 (21.6) | 53 (24.9) | 0.569 |
| Obesity, n (%) | 30 (30.9) | 46 (21.6) | 0.172 |
| Reason for admission | |||
| Sepsis and septic shock, n (%) | 28 (28.9) | 76 (35.7) | 0.247 |
| Respiratory failure, n (%) | 18 (18.6) | 44 (20.7) | 0.760 |
| GIT surgery, n (%) | 19 (19.6) | 44 (20.7) | 0.880 |
| Other causes, n (%) | 32 (33.0) | 49 (23.0) | 0.622 |
| Type of patient | |||
| Medical, n (%) | 60 (61.9) | 111 (52.1) | 0.077 |
| Surgical, n (%) | 36 (37.1) | 93 (43.7) | – |
| Trauma, n (%) | 1 (1) | 9 (4.2) | – |
| Early cardiovascular events | |||
| Arrhythmias, n (%) | 64 (66.0) | 110 (51.6) | 0.019 |
| Changes in ST segment, n (%) | 9 (9.4) | 19 (9.0) | 1.0 |
| Cardiac troponin-I (pg/ml), n (%) | |||
| Up to 45 | 71 (35.2) | 21 (21.6) | 0.039 |
| 46–200 | 32 (38.6) | 51 (23.9) | – |
| >200 | 44 (45.4) | 87 (40.8) | – |
| Some early cardiovascular event, n (%) | 89 (91.8) | 171 (80.3) | 0.012 |
GIT: gastrointestinal tract.
Eighty-three point nine per cent of the patients (260) suffered from an early cardiovascular event at admission (69%) and during the first of admission day, mainly (70.6%). The most common event was the appearance of arrhythmias (56.1%) followed by high levels of cTn-I (42.3%) and repolarization changes (9%). The patients with this or that cardiovascular event were older patients (67.9±15.2 vs. 61.6±15; p=0.008) and scored higher in the SAPS 3 severity index (62.6±15.4 vs. 55.2±15.6; p=0.002). The variables studied associated with in-hospital mortality are shown in Table 1.
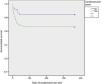
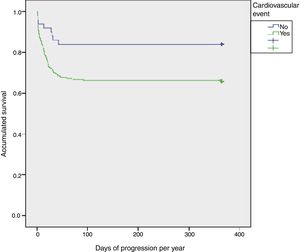
Mortality after hospital discharge was higher in patients with some cardiovascular event (35.8% vs. 8.2%, p=0.007). The results obtained in the multivariate analysis showed that the appearance of any cardiovascular events studied was associated with a higher mortality rate after hospital discharge (OR: 2.61; 95% CI: 1.124–6.096; p=0.026). Finally, in the survival analysis there was a statistically significant difference in the patient's progression with higher 1-year mortality rates in patients with cardiovascular events (p=0.013) (Fig. 1).
The fact that the patients included in the study were elderly patients with a high percentage of cardiovascular risk factors, high severity indices and whose main diagnosis was sepsis and septic shock means that these characteristics lead to higher chances of developing cardiovascular events and associated myocardial dysfunction.9
We should mention here that a high percentage of patients showed high levels of troponin-I (TnI), which is consistent with what different studies have described when it comes to showing higher mortality rates associated with cardiovascular events and, particularly, with the high levels of TnI reported.7,10 On the other hand, the echocardiographic findings confirm and impaired associated myocardial function.
Therefore, the results from our study confirm that the appearance of cardiovascular events occurs in a high percentage of critically ill patients. That is why we firmly believe that conducting routine echocardiographic controls and determining the levels of cTn-I during the first stages of their process should be used systematically in the standard practice for the assessment of the cardiac abnormalities that may have repercussions in a higher mortality rate.
It does not seem clear, though, whether the risk associated with the appearance of these events may be actually attenuated, or simply shows the highest degree of severity of the patients. A few preventive measures can be proposed such as, on the one hand, determining the levels of cTn-I in high risk surgical patients or, on the other hand, therapeutic measures such as initiating or adjusting the dose of antiaggregant drugs, statins, ACE inhibitors, or beta-blockers, whenever possible. Eventually, it would be through new studies that we would be able to confirm the utility of all these measures.
Please cite this article as: Ortega-Sáez M, López-Messa JB, Román-García B, Manuel-Merino FJ, Andrés-de-Llano J, Moradillo-González S. Repercusión clínica de la aparición de eventos cardiovasculares precoces en pacientes críticos en ventilación mecánica. Med Intensiva. 2018;42:563–566.