In the context of the critically ill child, the decisions that have to do with the adequacy of therapeutic effort (ATE) are, at the same time, cause for debate and reason for clinical interest. This is particularly the case in situations where the expected improvement has not occurred and technology is key for life support purposes.1–3 At present, the medical literature that describes end-of-life care in pediatric intensive care units (PICU)4 is scarce.
We hereby present a study that describes the characteristics of patients who have died in our PICU during the last decade. It is an observational retrospective study conducted after obtaining the approval from the clinical research ethics committee. The clinical reports of whose patients who died in the PICU from January 1 2006 through December 31 2016 were reviewed. The variables collected were: epidemiological, presence of underlying disease prior to PICU admission, cause for admission, care received (hemodynamic, respiratory, renal, antimicrobial, hematological and nutritional), main cause of death, days of stay at the PICU, day of admission, and adaptation of life support (cause, referral activity, and participation of the family in end-of-life care). A descriptive analysis of the answers was conducted using the SPSS® 19.0 software for Windows. Qualitative data were expressed as absolute frequencies and percentages, and quantitative data as means and interquartile ranges or as means and standard deviations based on the characteristics of the variable under analysis. In cases where one comparative analysis was conducted, qualitative data were compared using the chi-square test. p values <0.05 were considered statistically significant.
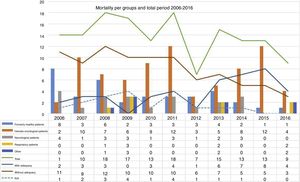
9049 children were reviewed of which 151 (1.7%) died; 147 patients (77 boys/70 girls) with an average age of 6.3 years old (IQR 0.05–21 years old) were included in the study. There were, on average, 13.7±3.4 deaths per year. Seventy-eight (78) out of the 147 patients had hemato-oncological conditions. Of the total number of patients with hemato-oncological conditions who died, 56/78 received one hematopoietic progenitor-cell transplantation (HPCT) (Fig. 1). Thirty-six (36) patients did not have a clinically significant disease (24.5%).
Mortality per groups and end-of-life approach in the study period. The straight lines from up to bottom represent overall mortality, patients where the ATE remained unreported, and patients were the ATE was actually reported. The dotted lines represent patients were the end-of-life approach remained unreported. The different frequency bars show, from left to right, and per year: health patients, hemato-oncological patients, neurological patients, respiratory patients, and patients included in the group “other”.
The most common cause for admission was respiratory failure (55/147) followed by sepsis/serious infection (35/147). Patients without a personal clinical history were admitted to the PICU following severe trauma (11/36) and septic shock (7/36).
Hemodynamic support was used in 117/147 patients. In 45/147 patients non-invasive mechanical ventilation was required, while 138/147 patients required invasive mechanical ventilation; 70/147 patients suffered renal failure being extra-renal depuration required in 34/70 patients; 115/147 patients required transfusion of hemoderivatives and 60/136 patients parenteral nutrition.
The most common cause of death was refractory hypoxemia (51/146; in one patient the main cause for death was not reported) followed by sepsis (31/146) and brain death (31/146). In patients without a significant clinical history, brain death was the main cause of death (18/36); among the patients with hemato-oncological disease (43/78) the main cause of death was refractory hypoxemia.
When it comes to the ATE, in 88 out of the 147 patients, this remained unexplained. The most common cause of death in the group without ATE was brain death (31/88) followed by sepsis/septic shock (26/88). In 41/59 of the remaining patients a report was given on the ATE as well as on why and what measures implemented. Twenty-seven (27) patients had hemato-oncological conditions being refractory hypoxemia the disease these measures were more commonly implemented against (22/41; p=0.001). Only in 2 out of the 75 patients who died due to acute or sudden disease life support adequacy measures were implemented. Only in one patient without an underlying prior disease ATE measures were implemented. The ATE measures were more commonly implemented following hemodynamic instability (p=0.04), need for mechanical ventilation (p=0.002), renal failure (p=0.01), parenteral nutrition (p<0.05) and transfusions of hemoderivatives (p=0.04).
The patients whose ATE was reported had longer hospital stays (22±17 days versus 5±7.7 days, p<0.05). The reason why the ATE was implemented had to do with both the irreversibility of the disease that prompted the PICU admission (in 18 out of 41 patients) and the poor prognosis of the underlying disease (in 12 out of 41 patients). Both the hemodynamic and the ventilatory support were withdrawn in 8/41 patients. Measures focused on well-being, sedation and analgesia were a priority in 7/41 patients. It was decided not to implement any new extraordinary measures in 6/41 patients and in 4/41 patients any pharmacological therapy not aimed at improving the patient's well-being was withdrawn. In 16 patients, the therapeutic remains unknown. The family was informed at all time and involved in the decision-making process in 29/41 patients.
In the series provided more than half of the patients who died suffered from hemato-oncological disease. In these, the HPCT was a prior common event.5 In turn, the ATE is often reported in patients with a prior condition and it would determine their prognosis prior to their referral to the PICU.3,6
This decision was barely reported in healthy children or in severe and acute processes with a quick resolution.
The ATE was associated with longer hospital stays. Although we do not mean to say that in order to consider the ATE it was required that a “certain amount of time” would need to pass, it does seem that this aspect was key in the decision-making process. Refractory hypoxemia was the main cause of death in the group of patients where the ATE was reported.6 Parents and caregivers were included in more than half the cases of ATE. It is well known that its perspective influences the therapeutic goal and defines well-being as a priority.4,7
This study has some limitations though. Except for epidemiological data, the remaining data were not collected thoroughly. They do not even include information on severity assessment scales at admission and in 4 patients no variable could be collected for the study. It would certainly be interesting to collect prospective and multicenter data with the exact time and moment when each change is implemented in the decision-making process.
In sum, given the specific conditions of our center, patients with onco-hematological conditions and, in particular, those with a prior history of HPCT are the main group of patients where the ATE was reported. Mainly, it was associated with long hospital stays, being the inotropic drug and ventilatory support withdrawal the most common measures implemented. We hope that this study will revitalize the debate and increase our actual knowledge on the ATE in the PICUs of our country. The creation of a national registry on this regard not only seems interesting but necessary.
Please cite this article as: Leoz Gordillo I, García-Salido A, Niño Taravilla C, de Lama Caro-Patón G, Iglesias Bouzas MI, Serrano González A. Mortalidad y adecuación del esfuerzo terapéutico en un servicio terciario de cuidados intensivos pediátricos: revisión de 11 años. Med Intensiva. 2018;42:561–563.