To investigate the differences in mortality at 28 days and other prognostic variables in 2 periods: IBERICA-Mallorca (1996–1998) and Infarction Code of the Balearic Islands (IC-IB) (2008–2010).
DesignTwo observational prospective cohorts.
SettingHospital Universitario Son Dureta, 1996–1998 and 2008–2010.
PatientsAcute coronary syndrome with ST elevation of ≤24h of anterior and inferior site.
Main variables of interestAge, sex, cardiovascular risk factors, site of AMI, time delays, reperfusion therapy with fibrinolysis and primary angioplasty, administration of acetylsalicylic acid, beta blockers and angiotensin converting enzyme inhibitors. Killip class, malignant arrhythmias, mechanical complications and death at 28 days were included.
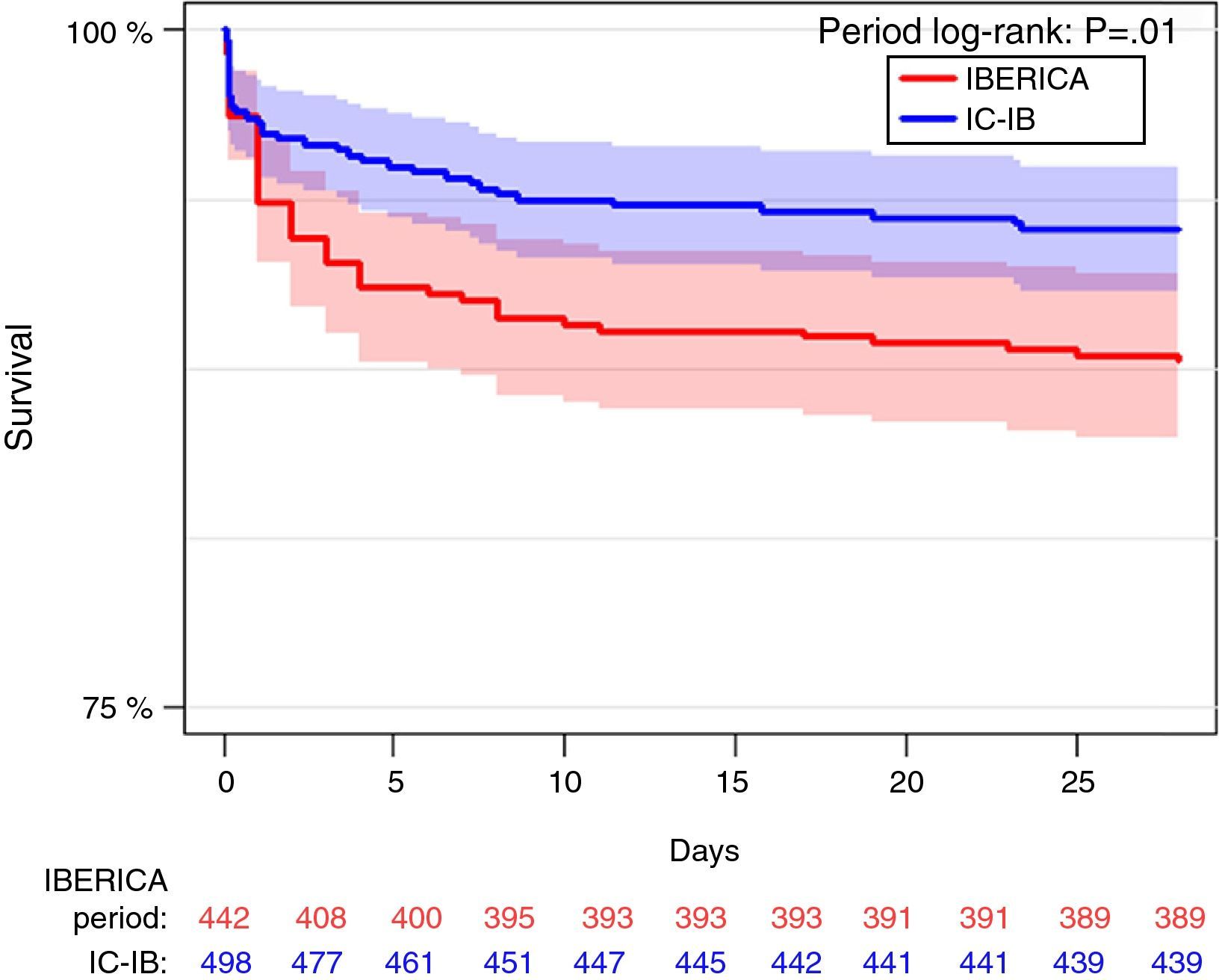
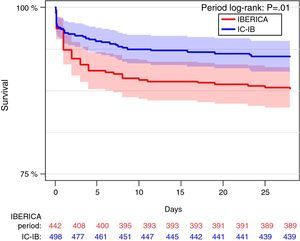
ResultsFour hundred and forty-two of the 889 patients included in the IBERICA-Mallorca and 498 of 847 in the IC-IB were analyzed. The site and Killip class on admission were similar in both cohorts. The main significant difference between IBERICA and IC-IB group were age (64 vs. 58 years), prior myocardial infarction (17.9 vs. 8.1%), the median symptoms to first ECG time (120 vs. 90min), median first ECG to fibrinolysis time (60 vs. 35min), fibrinolytic therapy (54.8 vs. 18.7%), patients without revascularization treatment (45.9 vs. 9.2%), primary angioplasty (1.0% vs. 92.0%). The mortality at 28 days was lower in the IC-IB (12.2 vs. 7.2%; hazard ratio 0.560; 95% CI 0.360–0.872; P=.010).
ConclusionThe 28-day mortality in acute coronary syndrome with ST elevation in Mallorca has declined in the last decade, basically due to increased reperfusion therapy with primary angioplasty and reducing delays time to reperfusion.
Investigar las diferencias en la mortalidad a 28 días y otras variables pronósticas en 2 periodos: IBERICA-Mallorca (1996–1998) y Código Infarto-Illes Balears (CI-IB) (2008–2010).
DiseñoDos cohortes prospectivas observacionales.
ÁmbitoHospital Universitario Son Dureta, 1996–1998 y 2008–2010.
PacientesSíndrome coronario agudo con elevación de ST de≤24h, de localización anterior e inferior.
Variables principales de interésEdad, sexo, factores de riesgo cardiovascular, localización, tiempos de actuación, tratamiento de reperfusión con fibrinólisis y angioplastia primaria, administración de ácido acetilsalicílico, betabloqueantes e inhibidores de la enzima conversora de la angiotensina. Se incluyeron el grado de Killip, las arritmias malignas, las complicaciones mecánicas y el fallecimiento a los 28 días.
ResultadosSe analizaron 442 pacientes de los 889 incluidos en el IBERICA-Mallorca y 498 de los 847 registrados en el CI-IB. La localización y el Killip fueron similares en ambas cohortes. Las principales diferencias significativas entre el grupo IBERICA y el CI-IB fueron: edad (64 vs. 58 años), infarto previo (17,9 vs. 8,1%), tiempo síntomas-primer ECG (120 vs. 90min), tiempo primer ECG-fibrinólisis (60 vs. 35min), tratamiento fibrinolítico (54,8 vs. 18,7%), pacientes sin reperfusión (45,9 vs. 9,2%), angioplastia primaria (1,0 vs. 92,0%). La mortalidad a los 28 días fue inferior en el CI-IB (12,2 vs. 7,2%; hazard ratio 0,560; IC 95% 0,360–0,872; p=0,010).
ConclusiónLa mortalidad a los 28 días en el síndrome coronario agudo con elevación de ST en Mallorca ha disminuido en la última década, probablemente debido a un mayor tratamiento de reperfusión con angioplastia primaria y a una reducción de los tiempos de reperfusión.
Acute coronary syndrome (ACS) registries have been introduced in Spain, making it possible to know the patient profile, management practices and evolution of the disease during the period of the registry, and allowing assessment of the impact of the adoption of clinical practice guides referred to ACS.1–5 The outcomes must be analyzed within a concrete time frame. Furthermore, the methodology underlying these registries is not homogeneous, and comparisons of the results obtained therefore must be made with caution.6
In our Autonomous Community (the Balearic Islands), the first data on acute myocardial infarction (AMI) were published by the IBERICA study (Investigation, Specific Search and Registry of Acute Coronary Ischemia [Investigación, Búsqueda Específica y Registro de Isquemia Coronaria Aguda]).7,8 The IBERICA study was a population-based registry of patients with AMI documenting the data referred to hospital management in 7 Spanish regions. The Hospital Acute Myocardial Infarction Registry Project (Proyecto de Registro de Infarto Agudo de Miocardio Hospitalario, PRIAMHO) allowed periodic evaluation of the management of patients with AMI and, in particular, the use of reperfusion techniques.9,10 The MASCARA study11 and the ARIAM registry3 (Analysis of Delay in Acute Myocardial Infarction [Análisis del Retraso en el Infarto Agudo de Miocardio]) in turn are important registries, because they offered us a view of the management of ST-segment elevation acute coronary syndrome (STE-ACS), reflecting an increase in the use of invasive strategies. A number of both national12,13 and international registries14–16 have shown that the implementation of primary angioplasty (PA) programs results in shortened intervention times, with improved outcomes in terms of patient mortality.
The IBERICA registry included individuals between 25 and 74 years of age residing on the island of Mallorca and treated due to AMI in both the public and private healthcare settings, with a follow-up of 28 days.7 There was no concrete intervention program during the period of the registry (1 June 1996 to 31 December 1998). In March 2008 the Balearic Islands Infarction Code (Código Infarto de les Illes Balears, CI-IB) care program was launched from the public healthcare setting.17 The aim of this initiative was to afford immediate STE-ACS management based on mechanical revascularization as the first treatment option in the reference hospital. A registry was carefully designed to document all the variables derived from the care process, and was formalized by the legislation of the Autonomous Community. An electronic format was used.
The present study comprises a comparative analysis of the data of the IBERICA registry and the CI-IB in patients with STE-ACS presenting an evolution of less than 24h and admitted to Son Dureta University Hospital, with the determination of differences in mortality after 28 days of follow-up following a decade of changes.
Materials and methodsDesignThe IBERICA registry was designed as a prospective, population-based, continuous multicenter study of AMI involving individuals between 25 and 74 years of age residing in different areas of the Balearic Islands, Castilla-La Mancha, Catalonia, Murcia, Navarra, the Basque Country and Valencia. The study period was from 1 July 1996 to 31 December 1998. During this period there were no consensus-based protocols, and the hospital intervention strategy was fundamented upon the recommendations of the clinical practice guides of the American Heart Association.18 Quality control was established, guaranteeing homogeneity of the methods and of the data collected. The variables were recorded using non-electronic case report forms. The investigators were trained and certified in the study coordinating center.
The CI-IB17 is a prospective, community-based, continuous multicenter registry involving patients diagnosed with STE-ACS presenting an evolution of less than 24h, with activation of the Infarction Code, and seen in any setting of the public healthcare network. Within the intervention strategy, a primary percutaneous coronary intervention model was defined, establishing agreement of the protocols according to the clinical practice guides19 with all the implicated physicians and Departments. This registry was started on 1 March 2008. The variables are recorded in electronic format in a core database managed by the public Ib-Salut service of the Balearic Islands. In order to guarantee quality and homogeneity of data collection, all the investigators participating in the field work were trained and placed in charge of follow-up, data quality control and logistic support in the data monitoring processes. No new variables have been added in either registry.
Study settingThe Autonomous Community of the Balearic Islands has a population of 1,106,049 inhabitants. A single reference hospital is available, with a hemodynamics laboratory, operating 24h a day, every day of the year. The Coronary Unit, ascribed to the Department of Intensive Care Medicine, has 8 beds. Up until November 2010, the reference center was Son Dureta University Hospital, which was replaced by Son Espases University Hospital, opened in December 2010.
Study populationThe IBERICA study only included patients between 25 and 74 years of age. In order to allow comparison of the two cohorts, inclusion was limited to those patients with STE-ACS of anterior and inferior location that met electrocardiographic reperfusion criteria in both periods,18,19 limiting the age to 25–74 years, and comprising patients attended in the same reference hospital with a definitive diagnosis of AMI defined by myocardial enzyme values (e.g., creatine kinase) over twice the upper limit of normal, and with a follow-up period of 28 days from the time of the event. Patients from other centers were excluded.
Study variablesThe study variables were stratified into 5 groups:
- 1.
Demographic characteristics: age, gender, cardiovascular risk factors (hypertension, smoking, dyslipidemia, insulin-dependent diabetes mellitus, non-insulin-dependent diabetes mellitus), history of ischemic heart disease (previous infarction or chest pain) and Killip class20 upon admission.
- 2.
Reperfusion treatment: fibrinolysis and PA. The administration of aspirin, beta-blockers and angiotensin converting enzyme inhibitors (ACEIs) was also documented. The criteria for fibrinolysis in the IBERICA group were atypical chest pain for over 20min, with ST-segment elevation >1mm on two or more consecutive leads and within the first 24h of evolution.18 The CI-IB registry considered activation of the Infarction Code with the aim of performing mechanical reperfusion when the ECG tracing showed an ST-segment elevation of >1mm on at least two limb leads, or an elevation of at least 2mm on two or more contiguous chest leads, accompanied by typical chest pain for over 20min within the first 12h of evolution.19 Each patient was individualized after between 12 and 24h. In cases with an evolution of under three hours, with non-availability of the hemodynamics room, pre-hospital fibrinolysis was carried out in the medicalized ambulance (061), in the Emergency Care Department, on in the Department of Intensive Care Medicine.
- 3.
The following time intervals were defined: time from symptoms onset until the first diagnostic ECG, and time from the first diagnostic ECG to reperfusion treatment.
- 4.
Surgery was included as follow-up procedure 28 days after the event.
- 5.
The complications studied during follow-up were: severe arrhythmias (ventricular fibrillation or sustained ventricular tachycardia), Killip class,20 stroke (hemorrhagic and/or ischemic) and mechanical complications (interventricular communication, mitral valve rupture and free wall rupture). Survival 28 days after the event was analyzed. Discharged patients were contacted in the outpatient clinic or by telephone.
The Research Ethics Committee did not consider the obtainment of informed consent to be necessary, since the registries were anonymous. Data dissociation was carried out to ensure anonymity, eliminating any link capable of identifying the patient. Confidentiality of the information was observed at all times as specified by Organic Act 15/1999 of 13 December, referred to Personal Data Protection, and Act 41/2002 of 14 November, regulating patient autonomy and the rights and obligation referred to clinical documentation and information.
Statistical analysisA descriptive analysis was made of the variables, calculating the mean and standard deviation (SD) in the case of quantitative variables with a normal distribution, and the median and quartiles in those with a non-normal distribution. Qualitative variables in turn were reported as frequencies and percentages, with the corresponding 95% confidence interval (95%CI). The contrasting of hypotheses was based on the Student t-test, Mann–Whitney U-test and the chi-squared/Fisher exact test, respectively. Survival was analyzed based on the Kaplan–Meier method for estimating the curves after 28 days, and the log-rank test was used to compare both periods. Multivariate analysis was also performed based on a Cox proportional hazards model to explore the relationship between the most relevant variables, the prognostic and all the potentially confounding parameters, and mortality up to 28 days. In sum, patient age, gender, diseases associated to cardiovascular risk and their treatment, time from symptoms onset to first monitoring, initial reperfusion treatment received, severity upon admission (Killip class), and complications were analyzed. The results were expressed as hazard ratios with the corresponding 95%CI. Statistical significance was considered for p<0.05. The IBM® SPSS® version 22.0 statistical package was used throughout.
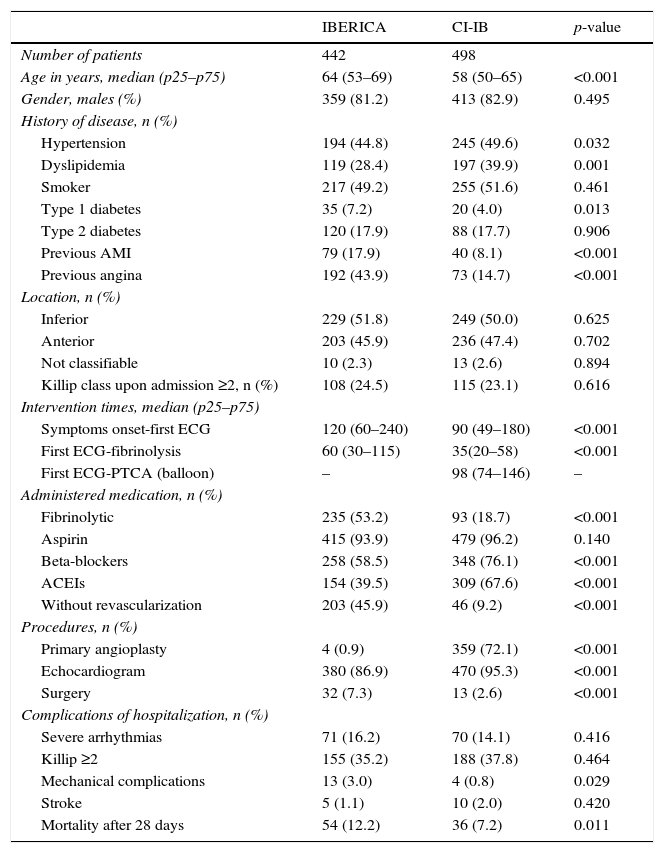
ResultsDemographic characteristicsA total of 889 cases of AMI were recorded during the IBERICA-Mallorca study period, and of these 442 met the inclusion criteria. In the CI-IB registry we selected 847 consecutive patients with STE-ACS. Of these, 498 were included in the comparative analysis. The demographic and clinical characteristics are summarized in Table 1. The median age was 64 years in the IBERICA period and 58 years in the CI-IB period, with a predominance of males in both periods. There was a greater proportion of patients with hypertension and dyslipidemia, and a lesser proportion with previous angina and previous AMI, in the group of patients corresponding to the CI-IB period. No differences were observed in terms of the site of AMI or in Killip class upon admission.
Demographic and clinical characteristics of the study population.
| IBERICA | CI-IB | p-value | |
|---|---|---|---|
| Number of patients | 442 | 498 | |
| Age in years, median (p25–p75) | 64 (53–69) | 58 (50–65) | <0.001 |
| Gender, males (%) | 359 (81.2) | 413 (82.9) | 0.495 |
| History of disease, n (%) | |||
| Hypertension | 194 (44.8) | 245 (49.6) | 0.032 |
| Dyslipidemia | 119 (28.4) | 197 (39.9) | 0.001 |
| Smoker | 217 (49.2) | 255 (51.6) | 0.461 |
| Type 1 diabetes | 35 (7.2) | 20 (4.0) | 0.013 |
| Type 2 diabetes | 120 (17.9) | 88 (17.7) | 0.906 |
| Previous AMI | 79 (17.9) | 40 (8.1) | <0.001 |
| Previous angina | 192 (43.9) | 73 (14.7) | <0.001 |
| Location, n (%) | |||
| Inferior | 229 (51.8) | 249 (50.0) | 0.625 |
| Anterior | 203 (45.9) | 236 (47.4) | 0.702 |
| Not classifiable | 10 (2.3) | 13 (2.6) | 0.894 |
| Killip class upon admission ≥2, n (%) | 108 (24.5) | 115 (23.1) | 0.616 |
| Intervention times, median (p25–p75) | |||
| Symptoms onset-first ECG | 120 (60–240) | 90 (49–180) | <0.001 |
| First ECG-fibrinolysis | 60 (30–115) | 35(20–58) | <0.001 |
| First ECG-PTCA (balloon) | – | 98 (74–146) | – |
| Administered medication, n (%) | |||
| Fibrinolytic | 235 (53.2) | 93 (18.7) | <0.001 |
| Aspirin | 415 (93.9) | 479 (96.2) | 0.140 |
| Beta-blockers | 258 (58.5) | 348 (76.1) | <0.001 |
| ACEIs | 154 (39.5) | 309 (67.6) | <0.001 |
| Without revascularization | 203 (45.9) | 46 (9.2) | <0.001 |
| Procedures, n (%) | |||
| Primary angioplasty | 4 (0.9) | 359 (72.1) | <0.001 |
| Echocardiogram | 380 (86.9) | 470 (95.3) | <0.001 |
| Surgery | 32 (7.3) | 13 (2.6) | <0.001 |
| Complications of hospitalization, n (%) | |||
| Severe arrhythmias | 71 (16.2) | 70 (14.1) | 0.416 |
| Killip ≥2 | 155 (35.2) | 188 (37.8) | 0.464 |
| Mechanical complications | 13 (3.0) | 4 (0.8) | 0.029 |
| Stroke | 5 (1.1) | 10 (2.0) | 0.420 |
| Mortality after 28 days | 54 (12.2) | 36 (7.2) | 0.011 |
PTCA: percutaneous transluminal coronary angioplasty; CI-IB: Balearic Islands Infarction Code; ECG: electrocardiogram; AMI: acute myocardial infarction; IBERICA: Investigation, Specific Search and Registry of Acute Coronary Ischemia; ACEIs: angiotensin converting enzyme inhibitors.
In the patients subjected to reperfusion treatment, the introduction of the CI-IB led to shortening of the intervention times versus the IBERICA cohort. A significant decrease was observed in the median interval between symptoms onset and first ECG (90 vs 120min, respectively; p<0.001) and in the interval between first ECG and fibrinolysis treatment (35 vs 60min; p<0.001).
TreatmentThe percentage of patients that received no reperfusion treatment was lower in the CI-IB than in the IBERICA cohort (9.2% vs 45.9%; p<0.001). In the CI-IB group we observed an increase in the use of beta-blockers (76.1% vs 58.5%; p<0.001), ACEIs (67.5% vs 39.5%; p<0.001) and aspirin, though in the latter case statistical significance was not reached.
PrognosisThe in-hospital complications, including malignant ventricular arrhythmias and the poorest Killip classes (III–IV) were similar in both periods (Table 1).
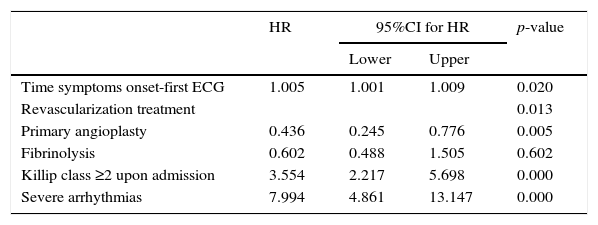
The mortality rate after 28 days of follow-up was lower in the CI-IB cohort (7.2% vs 12.2%; hazard ratio 0.560; 95%CI 0.360–0.872; p=0.010). The survival curves are shown in Fig. 1. A Cox model was developed with the variables associated to mortality up to 28 days after the event (Table 2).
Multivariate analysis of mortality after 28 days.
| HR | 95%CI for HR | p-value | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Time symptoms onset-first ECG | 1.005 | 1.001 | 1.009 | 0.020 |
| Revascularization treatment | 0.013 | |||
| Primary angioplasty | 0.436 | 0.245 | 0.776 | 0.005 |
| Fibrinolysis | 0.602 | 0.488 | 1.505 | 0.602 |
| Killip class ≥2 upon admission | 3.554 | 2.217 | 5.698 | 0.000 |
| Severe arrhythmias | 7.994 | 4.861 | 13.147 | 0.000 |
ECG: electrocardiogram; HR: hazard ratio; 95%CI: 95% confidence interval.
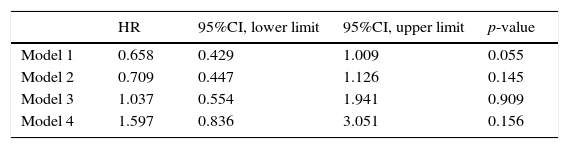
We also constructed Cox proportional hazards models referred to survival after 28 days corresponding to the CI-IB cohort versus the IBERICA group. The hazard ratio for the period was 0.658 (95%CI 0.429–1.009; p=0.055) on adjusting for age and gender, and 1.597 (95%CI 0.429–1.009; p=0.156) on introducing revascularization with fibrinolysis or PA (Table 3).
Multivariate analysis of mortality after 28 days corresponding to the patients of the CI-IB registry versus the IBERICA cohort.
| HR | 95%CI, lower limit | 95%CI, upper limit | p-value | |
|---|---|---|---|---|
| Model 1 | 0.658 | 0.429 | 1.009 | 0.055 |
| Model 2 | 0.709 | 0.447 | 1.126 | 0.145 |
| Model 3 | 1.037 | 0.554 | 1.941 | 0.909 |
| Model 4 | 1.597 | 0.836 | 3.051 | 0.156 |
HR: hazard ratio; 95%CI: 95% confidence interval
Model 1: adjusted for age and gender.
Model 2: model 1 plus dyslipidemia, smoker, type 1 diabetes, type 2 diabetes, previous AMI and previous angina.
Model 3: model 2 plus fibrinolysis and primary angioplasty.
Model 4: model 3 plus severe arrhythmias, Killip class ≥2 and Killip class ≥2 upon admission.
The results of this study reveal a positive evolution following introduction of the Infarction Code strategy in our Community, with a decrease in mortality mainly due to a marked increase in the use of reperfusion treatment, particularly PA.
Disease registries are useful because they evaluate the effects of treatment interventions, and thus more closely reflect the real life working conditions.21 Assuming that registries are necessary and useful, since they help determine the resource needs and the results of treatment,6 a relevant aspect of our registries is the fact that they compile data on a continuous and prospective basis, in an attempt to reduce possible information bias, complying with design and quality control criteria. These features allow us to regard the two registries as cohort studies representative of the care of patients with STE-ACS in our region.
On examining the demographic data we found males to predominate in both registries, and the patients were moreover younger in the CI-IB cohort. This could be attributed to the selection of younger patients sent to the reference hospital for reperfusion treatment with angioplasty, and also to the numerous meetings with the public healthcare centers and emergency services involved to explain them the importance of immediate identification and management of these patients.
The divergent data obtained regarding the risk factors could be due to changes in criteria, though the selection of cases may have exerted an influence. According to the data of the CORSAIB registry,22 the prevalence of hypertension and hypercholesterolemia in the population between 35 and 75 years of age in the Balearic Islands is 47% and of 24%, respectively. The increase in prevalence of these risk factors in patients of the CI-IB cohort could be due to a change in the cutoff point defining hypercholesterolemia.23 In this analysis, it should be mentioned that despite the smoking cessation campaigns, the percentage of smokers was not reduced in the patients with STE-ACS. The decrease in patients with a history of ischemic heart disease during the CI-IB period could be attributed to the progressive introduction of mechanical reperfusion as a therapeutic option starting in 2003, and to secondary prevention measures.24,25 Primary prevention with an increased use of statins possibly could contribute to reduce the number of ischemic events and modify the form of clinical presentation, with a progressive increase in the number of patients suffering non-ST-segment elevation acute coronary syndrome versus those with STE-ACS.26,27
The clinical characteristics upon admission were similar in both cohorts. The intervention time interval or delay is one of the parameters used to assess the quality of management in the emergency care setting. In the present study, the CI-IB cohort showed clear improvements in the intervals both from symptoms onset to the first diagnostic ECG tracing and from the first diagnostic ECG tracing to reperfusion treatment. The main reasons for this shortening of intervals could be improved health education; certain qualitative aspects in electrocardiographic diagnosis such as the introduction of a telephone-based ECG transmission application28; the maintenance of care dynamics as a key element in CI-IB; and improved efficacy in the decision making process on the part of the out-hospital and in-hospital emergency care services. In this regard, the concept of single three-party telephone contact among the attending physician (at the side of the patient), the coordinator of the 061 service, and the hemodynamist on duty makes an extremely important contribution to improve intervention efficacy. These results are consistent with those found in the literature.24,29
Independently of the different proportions in thrombolysis and mechanical revascularization seen on comparing both periods, an aspect which we consider to be important in our analysis is the significant decrease in patients who did not received reperfusion treatment during the interval 2008–2010. This finding highlights the great implication and adherence to protocol of the different professionals implicated in the acute ischemic heart disease management program.30,31
In our study, we observed an increased use of beta-blockers and angiotensin converting enzyme inhibitors in the CI-IB cohort – the percentages being higher than in other studies.11,32 This difference may be due to increased adherence to the recommendations of the clinical practice guides on one hand, and to the efforts to improve and homogenize management in the CI-IB through use of the registry on the other. Aspirin is considered a fundamental part of treatment in AMI with ST-segment elevation. Its use was slightly more prevalent in the CI-IB cohort and more frequent than in other studies.30–32
The main aspect deserving comment in our analysis is the decrease in 28-day mortality risk in the CI-IB cohort. The mortality rate was approximately twice as high in the IBERICA study. Our results are comparable to those of other both national33–35 and international studies.36,37 A number of factors could contribute to this difference. Firstly, mention must be made of the importance of early revascularization therapy and the increase in the percentage of patients that receive such treatment in the invasive strategy-based program. Secondly, the observed shortening in times to reperfusion treatment would also be a contributing factor. Lastly, there may be differences in the medical management profile, with an increased use of new antiplatelet drugs in the later registry. The validity of these results must be examined with caution, however, since the data come from two cohorts where the main limitation is vulnerability to confounding factors and possible patient screening bias – the analysis being limited to those patients admitted to the Department of Intensive Care Medicine and assisted in the reference hospital with the availability of a hemodynamics unit 24h a day.
Study limitationsComparisons between registries have important limitations, due to differences in the populations involved and in the inclusion criteria used. One of the important aspects of our study is that both registries represented exhaustive and consecutive cohorts of patients admitted alive to intensive care with ST-segment elevation. This has been an observational single-center study, and although the variables were documented on a prospective basis in both periods, certain differences in definition may have conditioned the results obtained. We consider that the findings of both registries illustrate the care process in the studied periods, though their comparative analysis may be conditioned by some limitations. On one hand, we cannot rule out the existence of bias referred to both the patient screening criteria and the exclusion criteria, fundamentally referred to the electrocardiographic reperfusion criteria used in the two periods. On the other hand, there may have been confounding variables related to the evolution of infarction from symptoms onset, or to the care process used, in the comparative analysis. Likewise, we do not know the efficacy of fibrinolytic treatment, particularly in the IBERICA cohort. These considerations mean that interpretation of the clinical results must be made with caution. Nevertheless, we believe that introduction of the invasive strategy program in STE-ACS produced the greatest difference in results between the two study periods.
ConclusionsThe 28-day mortality rate in STE-ACS has decreased over the last decade in Mallorca, mainly as a result of increased reperfusion treatment with PA, and a shortening of the reperfusion times.
Conflict of interestThe authors have received no financial support of any kind for carrying out this study. Likewise, no agreements resulting in benefits or payments for the authors have been signed with any commercial entity.
The authors thank Dr. Jaume Marrugat, of the Institut Municipal d’Investigació Mèdica de Barcelona, for his comments and support with the IBERICA registry data.
We thank the investigators of the CI-IB and IBERICA registries (see Annex I) for their interest, effort and dedication; development of the study and data compilation would not have been possible without their contribution.
Thanks are due to the Consellería de Salut for its constant support of the project.
We also wish to thank the OTIC (Information Technology Department of the Servicio de Salut) for software support and maintenance: Carlos Juan Bermell, Sergio Suárez, Gabriel Picó, Luis F. Manzanero. Thanks are also due to the Alamo Consulting Department: César Aparicio, Marc Sansalvador, Sara Serrano, Luis Riesco.
Group of investigators of the IBERICA-Mallorca registry: Armando Bethencourt, José Carrasco, Miguel Fiol, José Francisco Forteza, Alfredo Gómez, Jerónimo Grau, Miguel Ribas, Antonio Rodríguez, Joan Soler, Salvador Solivellas, Miguel Triola, Jorge Orellana, Pedro Ibáñez, Enrique Sospedra, Gabriel Redondo, Silvia Carretero, Magdalena Esteva, Jaime Bergadá, José Ignacio Ayestarán, Catalina Rubert, Josefina Gutiérrez, Francisco Alberti, Ana Rotger, Elena Bosch, Antonio Nicolau and Bernardo Vidal.
Group of investigators of the CI-IB registry: Miquel Fiol, Armando Bethencourt, Andrés Carrillo, Carlos Fernandez Palomeque, Vicente Peral, Alberto Rodríguez, Cristina Royo, Mireia Ferreruela, Alfredo Gómez, Rosa González, Marcos Pascual, Mar Alameda (Hospital Universitario Son Espases); Catalina Rubert, Lorenzo Socias, Catalina Forteza, Joan Torres, Tomás Ripoll (Hospital Son Llàtzer); Ramón Fernández Cid (Hospital Fundació Mateu Orfila); Sebastián Roig, Marga Vilar, Bernardo García de la Villa (Hospital Manacor); Marta Generelo (Hospital de Inca); Iñaki Unzaga, Inma Prieto, Juana María Vidal (SAMU 061); Guillem Frontera (IdISPa).
IB-Salut: Joan Pou, Luis Alegre, Antonia Salvá.
Information Technology Department (OTIC): Carlos Juan Bermell, Sergio Suárez, Gabriel Picó, Luis F. Manzanero. Alamo Consulting: César Aparicio, Marc sansalvador, Sara Serrano, Luis Riesco.
The names of the members of the CI-IB and IBERICA Research Group are listed in Annex I.
Please cite this article as: Socias L, Frontera G, Rubert C, Carrillo A, Peral V, Rodriguez A, et al. Análisis comparativo de 2 registros de infarto agudo de miocardio tras una década de cambios. Estudio IBERICA (1996–1998) y Código Infarto-Illes Balears (2008–2010). Med Intensiva. 2016;40:541–549.