Our population is growing older, and this implies an increase in age-related chronic diseases. As a result, we have a growing number of elderly persons with multiple health problems and with a poor functional reserve.1 All this indicates that the number of frail individuals in the Intensive Care Unit (ICU) will continue to rise.1 Such patients present greater disability at the time of discharge, are more likely to be admitted to a sociosanitary center, and experience greater mortality and longer convalescence periods.2,3
In view of the above, early detection of frailty is needed, and we should be aware of the prognostic usefulness of frailty as a complement to the usual mortality-centered scales employed (APACHE, SAPS3, etc.). In this way we could redirect our efforts to ensure earlier empathic and honest conversations focused on the shared planning of care, respecting the desires, preferences and values of our patients and their relatives.3 In addition, the detection of frailty at discharge from the ICU could be of help in continuous clinical decision making and in improving the efficiency of the healthcare system.
The Health Plan4 of Catalonia (Spain) 2011–2015 sought to place priority on prevention and care in people with advanced chronic disease conditions. The primary care teams (PCTs), using the NECPAL (NECesidades PALiativas [Palliative Needs]) tool,5 identified two frail person profiles: complex chronic patients (CCPs) and patients requiring an advanced chronicity care model (ACCM), with the idea of adopting an individualized care plan (Individualized Shared Intervention Plan [ISIP]) including advanced decision planning (ADP). All this in turn is recorded in the shared case history of Catalonia (SCHC) with the purpose of facilitating decision making.
The NECPAL tool was designed by the Qualy-ICO-CCOMS observatory, and has been validated in our setting for the identification of people with advanced chronic disease, an estimated life expectancy of 12 months, and a need for palliative care of some kind – the activation of specific plans therefore being necessary5 (Appendix B, see Supplementary material).
Given the new populational paradigm, the important and persistent barriers facing decision making regarding the adequacy of life support care (ALSC) and end-of-life care,6 which obliges intensivists to decide in this regard, and in concordance with the Health Plan4 of Catalonia, we decided to be more proactive in detecting these patients, conducting prognostic follow-up and seeking to ensure early detection of their predictable palliative needs.
In this context, over a period of 6 consecutive months and in all patients discharged from our ICU, we determined whether they were identified as CCPs or ACCM, and whether they had ISIP and/or ADP. If the patients were identified but did not have ISIP and/or ADP, interconsultation of the liaison nurse with the PCTs was made, recording the time to implementation of the ISIP and/or ADP. In turn, based on the NECPAL, we identified those patients in need of palliative care, reporting them to the LN to facilitate their identification as CCPs or ACCM and implementation of the ISIP and/or ADP. Lastly, during one year of follow-up, we checked how many patients were finally catalogued and whether they had their ISIP and/or ADP.
The study was approved by the Ethics Committee of our center. Since no interventions different from those of routine practice were involved, informed consent from the patients or their representatives was not considered necessary.
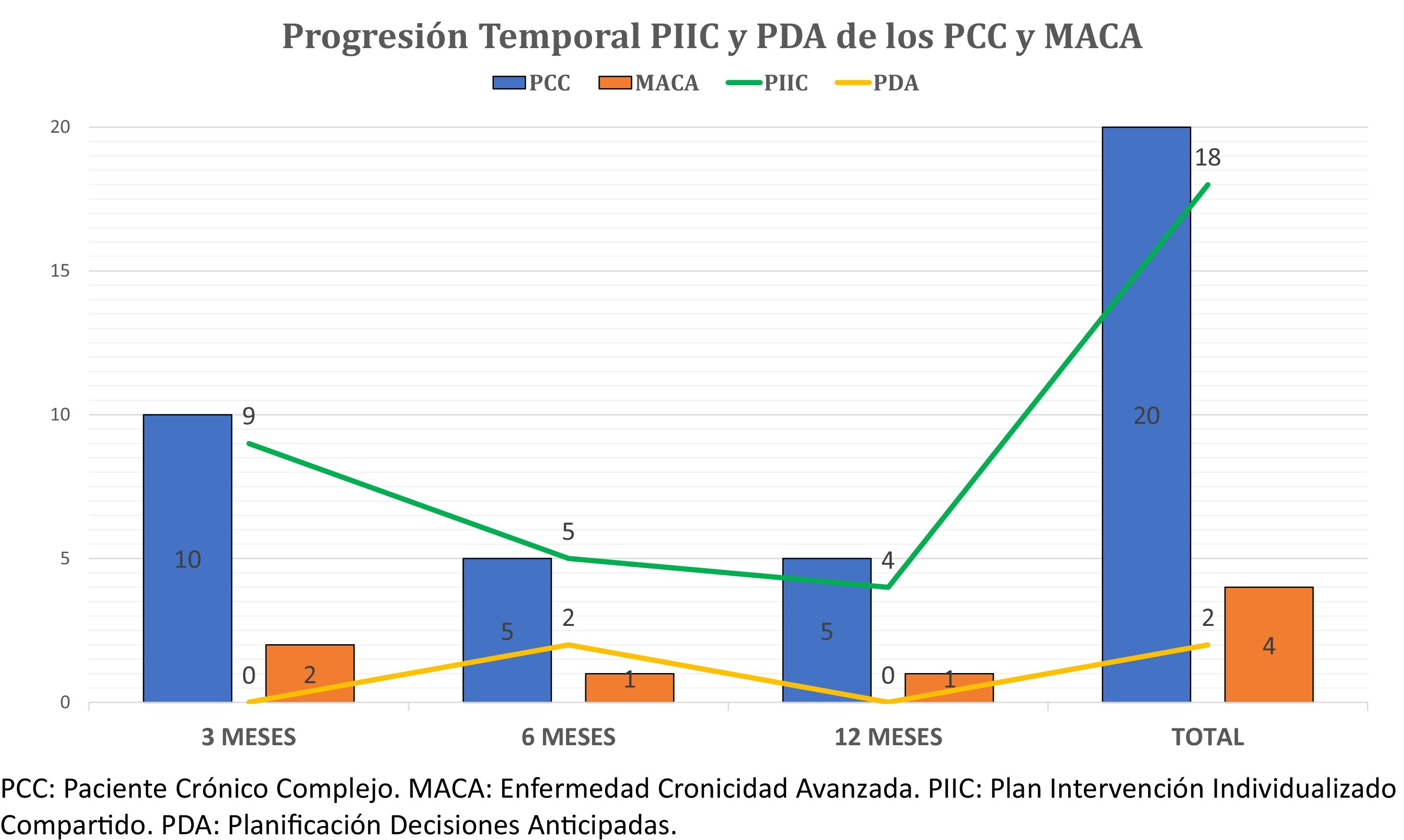
Of the 471 discharged patients, 24.6% (n = 116) were NECPAL positive, with a predominance of males (66.4%, n = 73) and a mean age of 66.3 ± 13 years. The mortality rate at one year was 28.9% (n = 33). Of all the subjects, 16 (13,7%) were previously CCPs (n = 14) or ACCM (n = 2), and 9 (56.2%) had their ISIP, while only one of them moreover also had ADP. After the year of follow-up and the pertinent LN interconsultations, a total of 10 ISIP (62.5%) and 4 ADP had been established (25%). Of the other 100 NECPAL positive patients at discharge, information corresponding to the SCHC could not be obtained in 5 cases, thus leaving 95 patients. At one year, 25.2% of them (n = 24) were catalogued as CCPs (n = 20) or ACCM (n = 4) by the PCTs, though 75% (n = 18) had been catalogued as such at 6 months. In this same period of time almost 60% (58.3%, n = 14) of the ISIP were established, together with the only two ADPs registered during the entire year of follow-up (Fig. 1).
Previous experiences with the NECPAL5 tool are available in other populations for detecting chronic patients with palliative care requirements,7 and even in seeking to predict their mortality.8 To our knowledge, however, this is the first time the mentioned tool is used to detect the palliative needs of patients at discharge from the ICU and to try to implicate the professionals of the PCTs.
Although a range of scales have been validated in different populations to measure frailty,9 none of them have sufficient discriminating capacity to be universally used in the ICU. Until such a tool becomes available, the best approach is to use the scale that is most feasible in our setting and which allows us to make the best decisions regarding our patients. In our healthcare setting it makes full sense to use the NECPAL,5 for in addition to already having been validated and allow multimodal assessment (including comorbidities, subjective aspects of demand or need for palliative care, and clinical severity, disease progression, nutritional, functional, social, emotional distress and resource utilization indicators), it can be consulted and shared by means of the SCHC.
The World Health Organization (WHO) recommends addressing frailty, individual preferences, priorities and psychosocial resources, and incorporation of the latter to the individualized planning of care, since these factors influence individual patient quality of life.10
The few ADPs established initially and at one year of follow-up offer important room for improvement which we should take advantage of.
In view of its prognostic importance, the detection of frailty should be incorporated to our routine clinical practice in order to adequately adjust life support management both upon admission to and at discharge from the ICU. In addition, this would allow us to implement early palliative care strategies and – where needed – to provide adequate end-of-life care.
Please cite this article as: Ferré C, Canelles S, Daniel X, Rubio O, Esteban F, Pobo A. Detección al alta de UCI de la fragilidad y necesidades paliativas del paciente crítico en colaboración con atención primaria. Med Intensiva. 2022;46:101–103.