The aim of the study is to ascertain the most relevant aspects of the current management of renal replacement therapy (RRT) in critically ill patients, and to analyze renal function recovery and mortality in patients undergoing RRT.
MethodsA non-interventional three-month observational study was made in 2012, with a follow-up period of 90 days, in 21 centers in Catalonia (Spain). Demographic information, severity scores and clinical data were obtained, as well as RRT parameters. Inclusion criteria: patients aged ≥16 years admitted to Intensive Care Units (ICUs) and subjected to RRT.
ResultsA total of 261 critically ill patients were recruited, of which 35% had renal dysfunction prior to admission. The main reason for starting RRT was oliguria; the most widely used RRT modality was hemodiafiltration; and the median prescribed dose at baseline was 35mL/kg/h. The median time of RRT onset from ICU admission was one day. The mortality rate at 30 and 90 days was 46% and 54%, respectively, and was associated to greater severity scores and a later onset of RRT. At discharge, 85% of the survivors had recovered renal function.
ConclusionsCurrent practice in RRT in Catalonia abides with the current clinical practice guidelines. Mortality related to RRT is associated to later onset of such therapy. The renal function recovery rate at hospital discharge was 85% among the patients subjected to RRT.
Determinar las características más relevantes del manejo actual de las terapias continuas de reemplazo renal (TRRC), así como analizar la evolución de la función renal y la mortalidad de los pacientes tratados con estas terapias.
MétodosEstudio observacional sin intervención de 3meses de duración en 2012 con un periodo de seguimiento de 90 días, realizado en 21 hospitales de Cataluña, en que se registraron escalas de gravedad, datos demográficos, clínicos y de las TRRC. Criterios de inclusión: pacientes de ≥16 años ingresados en cuidados intensivos (UCI) tratados con TRRC.
ResultadosSe seleccionó a 261 pacientes. Un 35% tenía disfunción renal previa al ingreso. El principal motivo para iniciar las TRRC fue la oliguria, la modalidad más empleada fue la hemodiafiltración y la mediana de dosis prescrita al inicio fue de 35mL/kg/h. La mediana de tiempo de inicio de la TRRC desde el ingreso en UCI fue de un día. La mortalidad a los 30 y 90 días fue de 46 y 54%, respectivamente, y se relacionó con peores valores en las escalas de gravedad y con un inicio más tardío de la TRRC. Al alta hospitalaria, un 85% de los supervivientes había recuperado la función renal.
ConclusionesEl manejo de las TRRC en Cataluña se adecua a los estándares recomendados por las guías actuales. La mortalidad asociada a las TRRC se relaciona con un inicio más tardío. Un 85% de los pacientes tratados con TRRC recuperan la función renal al alta hospitalaria.
Acute renal dysfunction is a serious common complication in intensive care units (ICU) associated with the use of continuous renal replacement therapies (CRRT) and reported in 4–10 per cent1 of the cases. In 2007, one worldwide multicenter epidemiological study2 revealed that there are various CRRTs in use today, that the most widely used modality is continuous veno-venous hemofiltration (CVVHF, 53 per cent), that the mean dose prescribed was usually 20mL/kg/h and that the intra-hospital mortality of patients treated with CRRT was around 64 per cent. Likewise, the multivariate analysis of this study showed that none of the variables associated with the therapy (technical modality, material of the membrane, anticoagulation, or dose) had an impact on the patients’ mortality. Then, in 2009, another multicenter, observational study3 carried out among 30 ICUs also found that higher doses do not have an impact on survival and that if any, they may improve the survivors’ times of mechanical ventilation and stay at the UCI.
At that time two (2) different survey studies that would be the foundation of what later would become the two (2) best designed-clinical trials about doses and CRRTs were conducted: the VA/NIH Acute Renal Failure Trial Network Study4 (ATN), published in 2008, and the Renal Replacement Therapy Study Investigators5 (RENAL) study, published in 2009– both of them ratified that the dose of CRRT does not have an impact on the patients’ prognosis. These were the most outstanding findings from those early surveys: the survey6 that would be the foundation for the ATN study analyzed 26 centers and confirmed that the intermittent renal replacement therapy (IRRT) was the most common (57 per cent) of all renal replacement therapies (RRT) used in ICUs; when the CRRT was used, the most widely used technique was continuous venovenous hemodialysis (CVVH, 70 per cent) and in over 80 per cent of all cases, dose titration was not weight-based. In the survey7 prior to the RENAL study, 34 centers were studied and these were the findings: the CRTT was the most widely used therapy, and the predilution hemodialfiltration (pre-HDF, 62 per cent) was the most widely technique; dose titration was not weight-based, with an average 2L/h effluent dose. Closer to our country, in England, one survey8 conducted among 270 ICUs confirmed that the most widely used technique was hemofiltration (CVVHF, 65 per cent) with doses over 35mL/kg/h in 75 per cent of all cases. In our setting, the FRAMI9 study showed that 75 per cent of all RRTs were continuous therapies, yet in 10 per cent, the IRRT was used concomitantly and renal dysfunction was high–around 15 per cent.
In this context, we decided to conduct one multicenter study in order to know the actual management of these RRTs in the acute patient in our setting, the actual progression of renal function (RF), and the prognosis of patients treated with these therapies.
Patients and methodsDesign: Prospective, multicenter, epidemiological study. The ethics committees from the six (6) promoting hospitals approved this study and all agreed that no signature from any written informed consents would be needed given the anonymous and non-interventional nature of the study. However, the patients’ families were informed on the nature of the study and data collection. The remaining centers individually informed their respective ethics committees requesting their approval to participate in the study. The study was designed by six (6) experts in the field of IRRT from six (6) different hospitals; these experts were the principal investigators and promoters of the study. The data collection sheet was designed to avoid any excessive information that might jeopardize the collection of data through an online registry (www.regisfra.com) that remained active during the stage of study recruitment. The creation and maintenance of this web fell under the responsibility of the industry, and was maintained during three (3) months for the online registry. The statistical analysis was conducted by the head of the epidemiology unit of one of the promoting hospitals within the Area of Preventive Medicine and Public Health of the Universidad Autónoma de Barcelona.
Study period: the recruitment of patients spanned between the months of February, 2012 and May, 2012 and the follow-up lasted for 90 days.
Inclusion criteria: two (2) different inclusion criteria were needed to be able to participate in the study: age ≥16 years old and receiving one RRT in the ICU. Patients were only included once.
Setting: the study was conducted in the ICUs of 21 different hospitals–both second-level regional hospitals and high-tech tertiary hospitals from the four (4) Catalan provinces.
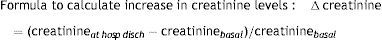
Variables of interest: the baseline characteristics of patients such as the demographic variables: age, sex, and the basal plasma creatinine level (creatinineb). When it comes to creatinineb, the levels of creatinine recorded in the hospital files or in primary care during the three (3) months prior to the actual hospital admission were the ones that were taken into consideration. In the absence of prior hospital admissions and if patients were young (<50 years old) and had no comorbidities, the basal creatinine level was estimated at around 1mg/dL. Otherwise, this variable was not recorded. At admission, several severity scores were recorded like the Charlson Comorbidity Index,10 the Liaño Individual Severity Index (ISI)11 and the Sepsis-related Organ Failure Assessment (SOFA)12 severity score; the type of patient (medical, surgical, traumatic), the clinical data at admission such as creatinine (creatinine0), oliguria0 (diuresis under 400mL/day the first day of admission), nephrotoxic drugs, need for amines and mechanical ventilation. At the beginning of the RRT, the levels of creatinine (creatinine1), the urinary debit during the last 6h prior to the beginning of the RRT (diuresis6hTRR), the SOFA at the beginning of the RRT (SOFA1) and the characteristics of the RRT were all recorded. These were the variables recorded: the location of vascular access (jugular, femoral or subclavian), the type of RRT (CRRT or IRRT), the modality: CVVHF, Pre-HDF, CVVH, the slow continuous ultrafiltration (SCUF), the intermittent hemodialysis (IHD), the slow extended dialysis, or other intermittent modalities. The clinical situation of the patient (sepsis, ischemia, nephrotoxicity, poisoning, multifactor or other) and the reason for beginning the RTT (oliguria or other) were recorded as well. The dose registered was the one prescribed during the first day–in mL/kg/h, but if the dose exceeded 35mL/kg/h it was considered a high volume or flow. Also the duration of the RRT and the need for IHD after CRRT withdrawal were recorded. The withdrawal of the CRRT followed the protocols of each center. Similarly, the recovery of renal function (RF) was recorded–defined as the determination of plasma creatinine levels <1.2mg/dL while not needing RRT in patients without prior RF impairment. Finally, the levels of ICU and hospital mortality were recorded after 30 and 90 days.
We tried to complete all conflicting or absent pieces of information by making phone calls or sending e-mails.
Statistical analysisFirst, one descriptive analysis of the sample was conducted. Percentages were used for the categorical qualitative variables, and the means and the minimum and maximum values were determined for the continuous quantitative variables.
Two (2) comparative studies were conducted aimed at determining the variables associated with the renal function prognosis and the variables associated with mortality.
In the bivariate analyses, the variables were compared using the chi square test or Fisher's exact test for small sample sizes. The Student's t test was used for continuous variables of normal distribution and the Mann–Whitney U test was used for continuous variables of asymmetrical distribution.
All mortality-associated factors in relation to the moment the RRT was initiated were analyzed. To study mortality, the multiple logistic regression was used: all variables with p values <0.15 obtained using the univariate analysis were included in the multivariate Cox proportional-hazards regression model. Adjustments: high-tech hospitals, sex, setting (medical, surgical, or trauma), oliguria, the Liaño ISI, age, time elapsed from hospital admission to the initiation of the RRT, time elapsed from ICU admission to the initiation of the RRT, and time elapsed from hospital admission to ICU admission, SOFA severity score at ICU admission and SOFA severity score at the initiation of the RRT.
p values <0.05 were considered statistically significant.
Data were analyzed using the SAS software, version 9.3 (SAS Institute Inc., Cary, North Carolina, USA).
ResultsTwenty-one (21) centers participated of which thirteen (13) had Hemodialysis Units, and 261 critical patients were included with the following characteristics: 67 per cent were males with an average age of 66 years old. When it comes to severity scores, the mean Charlson Comorbidity Index was 3, the mean Liaño ISI was 0.64, and the SOFA severity score at ICU admission was 8, and when the RRT was initiated the SOFA severity score was 10. At 30 and 90 days mortality was 42.91 and 54.02 per cent, respectively. The main reason for initiating RRT was oliguria in 82.75 per cent of the patients. When it comes to therapy, catheters were placed in the central vein, and the most commonly used route was the femoral approach (85.6 per cent). Anticoagulation of the extracorporeal circuit was induced using unfractionated heparin sodium in almost all of the centers except for one that had just started regional anticoagulation with citrate. When it comes to the type of RRT, the CRRT was the RRT of choice in 91.57 per cent of the cases being the pre-HDF the most widely used technical modality (86.61 per cent), with a prescribed mean dosage at the beginning of 35mL/kg/h. In 60 per cent of the cases, the dosage titration during the first day of the CRTT was between the ranges of 25 and 35mL/kg/h. Twenty-eight per cent of the patients received a high volume (effluent dose >35mL/kg/h). Patients who received a high volume were in more serious condition both at ICU admission (SOFA0 10 vs 8; p=0.022) and when the therapy was initiated (SOFA1 11.5 vs 10; p=0.045), but their mortality was not different from that of the patients who received lower doses (p=0.74). The time mean of RTT initiation from the moment of ICU admission was one day. The mean duration of the RRT was five (5) days, and after the withdrawal of the CRTT, up to 22 per cent of patients received IHD for another five (5) days. Only 8.4 per cent of ICU patients received IRRT from the beginning of the therapy with a mean duration of therapy of three (3) days. The mean duration of ICU stays was 12 days followed by another 14 days in the hospital ward (Table 1).
Characteristics of study patients and renal replacement therapies.
| Variables | Results |
|---|---|
| Age [years, median (min–max)] | 66.2 (16.1–87.2) |
| Sex [male, n (per cent)] | 175 (67.1) |
| Severity scores [median (min–max)]: | |
| Charlson | 3 (0–17) |
| Liaño ISI | 0.65 (0.07–1.12) |
| SOFA0 | 8 (0–17) |
| SOFA1 | 10 (1–18) |
| CV-SOFA0 | |
| 0–2 | 97 (37.2) |
| 3–4 | 164 (62.8) |
| Biomarker of renal function: | |
| Creatinineb [mg/dL, median (min–max)] | 1.06 (0.41–7.40) |
| Creatinine0 [mg/dL, median (min–max)] | 2.17 (0.3–17.71) |
| Creatinine1 [mg/dL, median (min–max)] | 2.87 (0.47–17.71) |
| Diuresis6hTRR [mL; median (min–max)] | 80 (0–400) |
| Situation triggering acute renal failure: [n (per cent)] | |
| Multifactorial | 108 (41.4) |
| Ischemia | 29 (11.1) |
| Sepsis | 92 (35.6) |
| Poisoning | 4 (1.5) |
| Nephrotoxicity | 10 (3.8) |
| Other | 18 (6.9) |
| Clinical situation at ICU admission: [n (per cent)] | |
| Oliguria0 | 225 (86.2) |
| Shock0 | 200 (76.7) |
| Mechanical ventilation0 | 178 (68.2) |
| Vascular approach [n (per cent)]: | |
| Femoral | 222 (85.6) |
| Jugular | 32 (12.26) |
| Subclavian | 7 (2.68) |
| Initial RRT: | |
| CRRT | 239 (91.6) |
| IRRT [n (per cent)] | 22 (8.4) |
| Dose of CRRT [mL/kg/h; median (min–max)] | 35 (10–90) |
| Duration of the CRRT [days; median (min–max)] | 5 (1–35) |
| Duration of the IRRT [days; median (min–max)] | 6 (1–148) |
| Mortality of CRRT [n (per cent)]: (initial) | |
| Pre-HDF | 207 (86.61) |
| CVVHF | 19 (7.95) |
| CVVH | 10 (4.18) |
| SCUF | 3 (1.26) |
| CRRT and IRRT | 46 (17.62) |
| Mortality of IRRT [n (per cent)]: | |
| IHD | 76 (96) |
| Other | 3 (3.95) |
| Recovery of renal function [n (per cent)] | |
| At hospital discharge (alive=135) | 115 (85.18) |
| Several time frames: [days, median (min–max)] | |
| Pre-ICU days | 0 (0–120) |
| ICU to RRT | 1 (0–89) |
| Hospital to RRT | 3 (0–121) |
| ICU stay | 12 (1–108) |
| Stay at hospital ward | 14 (1–123) |
| Hospital stay | 25 (1–208) |
| Mortality: [n (per cent)] | |
| ICU | 112 (42.91) |
| Hospital | 126 (48.28) |
| At 30 days | 121 (46.36) |
| At 90 days | 141 (54.02) |
All words containing subindex 0 represent admission at ICU; subindex 1 represents initiation of the RRT.
Comorbidity: Charlson Comorbidity Index; Creatinine0: creatinine at admission; Creatinina1: Creatinine at the initiation of the RRT; Creatinineb: basal creatinine; CV-SOFA0: Cardiovascular SOFA at ICU admission; from hospital to ICU: time elapsed from hospital admission to ICU admission; from hospital to RRT: time elapsed from hospital admission to initiation of RRT; from ICU to RRT: time elapsed from ICU admission to the initiation of the RRT; Diuresis6hRRT: urinary debit during the 6h prior to initiating RRT; Dose of CRRT: prescribed dose of continuous therapy; Pre-HDF: continuous venovenous hemodialfiltration; IHD: intermittent hemodialysis; CVVH: continuous venovenous hemodialysis; CVVHF: continuous veno-venous hemofiltration; Oliguria0: diuresis <400mL/day during the first day of ICU admission; SCUF: slow continuous ultrafiltration; SOFA0: SOFA at ICU admission; SOFA1: SOFA at the initiation of the RRT; CRRT: continuous renal replacement therapies; IRRT: intermittent renal replacement therapy; Recovery of renal function: creatinine <1.2mg/dL in the absence of RRT.
The patients’ prior RF was assessed and a separate analysis was conducted to separate patients with normal prior RF from patients with abnormal prior RF.
In individuals with normal prior RF, the recovery of RF was achieved both in survivors and in absence of depurative therapy if the levels of creatinine at hospital discharge had been normalized (creatinine <1.2mg/dL) (Table 1).
Thirty five per cent of the patients had an impaired RF (creatinine >1.2mg/dL) prior to hospital admission. In these patients with impaired prior RF, the recovery of RF was achieved when the levels of creatinine at hospital discharge had increased <25 per cent compared to basal creatinine levels.
Recovery of RF in survivors at hospital discharge scored 85 per cent. One bivariate analysis of the predictors of RF recovery was conducted in patients with normal prior RF and it was determined that there was a correlation between the recovery of RF and lower comorbidity, lower plasma creatinine level both at hospital discharge and when therapy was initiated, and lower need for IHD during hospital admission. Likewise, the recovery of RF was associated with a more serious medical condition when therapy was initiated and also with the fact of being hospitalized in high-tech hospitals (see Table 2).
Bivariate analysis of predictors of renal function recovery at hospital discharge.
| Independent variables | Recovery of RF (n=65) | Absence of RF recovery (n=16) | OR (95 per cent CI | p |
|---|---|---|---|---|
| High-tech hospital [n (per cent)] | 35 (53.8) | 4 (25) | 3.5 (1.09–13.6) | 0.045 |
| Feminine sex [n (per cent)] | 33 (50.8) | 12 (75) | 0.34 (0.09–1.1) | NS |
| Oliguria1 [n (per cent)] | 51 (78.5) | 13 (81.3) | 0.84 (0.17–3.07) | NS |
| Mechanical ventilation [n (per cent)] | 43 (66.2) | 9 (56.3) | 1.52 (0.49–4.63) | NS |
| IHD (n) | 15 (23.1) | 11 (68.8) | 0.14 (0.04–0.44) | 0.001 |
| Dose >35mL/kg/h [n (per cent)] | 15 (23.1) | 3 (18.8) | 0.8 (0.219–4.2) | NS |
| Liaño ISI [median (min–max)] | 0.71 (0.07–1.12) | 0.58 (0.1–1.06) | 4.1 (0.5–38.8) | NS |
| Age (years) [median (min–max)] | 59 (20–85) | 68 (16 –83) | 0.99 (0.96–1.02) | NS |
| Creatinineb (mg/dL) [median (min–max)] | 0.84 (0.41–1.19) | 1 (0.6–1.13) | 0.06 (0.002–1.35) | NS |
| Creatinine0 (mg/dL) [median (min–max)] | 1.44 (0.3–11) | 2.45 (0.7–9.0) | 0.77 (0.6–0.98) | 0.04 |
| Creatinine1 (mg/dL) [mediana (min–max)] | 2.2 (0.5–11) | 3.9 (1.8–9) | 0.75 (0.6–0.96) | 0.03 |
| Diuresis6hRRT (mL 6h) [median (min–max)] | 118 (0–410) | 78 (0–390) | 1.0 (0.99–1.0) | NS |
| Time from HOSP to ICU (days) [median (min–max)] | 0 (0–65) | 0 (0–26) | 1.03 (0.98–1.13) | NS |
| Time from ICU to RRT (days) [median (min–max)] | 2 (0–35) | 0.5 (0–14) | 1.12 (0.99 –1.41) | NS |
| Time from hospital to RRT (days) [median (min–max)] | 3 (0–65) | 1 (0–27) | 1.05 (0.99–1.15) | NS |
| Comorbidity [median (min–max)] | 2 (0–7) | 3 (0–9) | 0.73 (0.56–0.94) | 0.02 |
| SOFA0 [median (min–max)] | 8 (1–16) | 7 (0–10) | 1.1 (0.96–1.3) | NS |
| SOFA1 [median (min–max)] | 10 (2–18) | 7 (1–14) | 1.22 (1.05–1.44) | 0.01 |
| Dose of CRRT (mL/kg/h) [median (min–max)] | 35 (19–60) | 33 (15–42) | 1.02 (0.94–1.12) | NS |
Creatinine0: plasma creatinine levels at ICU admission; Creatinine1: plasma creatinine levels at the initiation of the RRT; Creatinineb: prior plasma creatinine levels at; Diuresis6hTRR; 6-h urine volume collection prior to the initiation of the RRT; Dose of CRRT: treatment doses of CRRT (effluent dose); RF: renal function; High-tech hosp: High-tech hospitals; Liaño ISI: Liaño Individual Severity Index; NS: non-significant (p>0.05); SOFA0: SOFA severity score determined at ICU admission; SOFA1: SOFA severity score determined at the initiation of the RRT; Time from hospital to ICU: time from hospital admission to ICU admission; Time from hospital to RRT: time elapsed from hospital admission to the initiation of the RRT; Time from ICU to RRT: time elapsed from ICU admission to the initiation of the RRT; RRT: renal replacement therapy.
Nevertheless, the multivariate analysis could not demonstrate any independent correlations between the variables studied and the recovery of RF.
Analysis of mortalityMortality at the ICU was 42.91 per cent, at 30 days it was 46.36 per cent, at hospital discharge it was 48.28 per cent, and at 90 days it was 54.02 per cent. No patient hospitalized due to poisoning or nephrotoxicity or whose initial RTT was SCUF or IRRT died after hospital discharge. The analysis of mortality was conducted both at 30 and 90 days. Since the analyses conducted at 30 and 90 days were so similar, the 90-day analysis was showed since it included all deceased patients. The bivariate analysis showed that the variables associated with mortality were: oliguria, shock, need for mechanical ventilation at hospital admission, the severity scores (SOFA and the Liaño ISI), and a longer period of time elapsed from hospital admission until the initiation of depurative therapy. Results are shown in Table 3. The multivariate analysis confirmed that mortality was associated with a higher SOFA score at the beginning of the technique (SOFA1 11 vs 8; RR 1.13 and 95 per cent CI: 1.1–1.2; p=0.0007) and with a longer period of time elapsed from ICU admission to the initiation of the RTT (0 vs 1 day; RR 1.02 and 95 per cent CI: 1.01–1.03; p=0.0016). The medical context turned out to be a protective factor against mortality. Results are shown in Table 4.
Bivariate analysis of predictive variables of mortality 90 days after hospital admission.
| Independent variables | 141 deceased patients (54 per cent) | 120 alive patients (46 per cent) | RR (95 per cent CI | p |
|---|---|---|---|---|
| Feminine sex [n (per cent)] | 103 (73) | 76 (63) | 1.24 (0.83–1.84) | NS |
| Age [median (IQR)] | 66.9 (21) | 64 (22) | 1.01 (0.99–1.02) | NS |
| Comorbidity [median (IQR)] | 3 (3) | 2 (3) | 1.06 (0.98–1.14) | NS |
| Context [n (per cent)] | ||||
| Medical | 45 (32) | 49 (41) | ||
| Surgical vs medical | 94 (67) | 62 (52) | 1.43 (0.97–2.1) | NS |
| Trauma vs medical | 2 (1.4) | 9 (7.5) | 0.34 (0.08–1.4) | NS |
| Etiology [n (per cent)] | ||||
| Sepsis | 57 (40) | 33 (26) | ||
| Ischemia vs sepsis | 14 (10) | 16 (13) | 0.7 (0.4–1.3) | NS |
| Multifactor vs sepsis | 59 (42) | 48 (40) | 0.7 (0.5–1.1) | NS |
| Nephrotoxicity vs sepsis | 1 (0.7) | 10 (8) | 0 | |
| Poisoning vs sepsis | 0 (0) | 3 (2.5) | 0 | NS |
| Other vs sepsis | 10 (7) | 10 (8) | 0.8 (0.4–1.7) | |
| High-tech hosp | 77 (55) | 54 (45) | 1.36 (0.95–1.95) | NS |
| Mechanical ventilation | 115 (82) | 69 (57.5) | 3.08 (1.87–5.1) | <0.001 |
| Shock | 123 (87) | 80 (67) | 2.65 (1.54–4.56) | <0.001 |
| Liaño ISI [median (IQR)] | 0.68 (0.3) | 0.59 (0.4) | 5.7 (2.4–13.6) | <0.001 |
| SOFA-CV [n (per cent)] | ||||
| 3–4 | 99 (70) | 65 (54) | 1.9 (1.3–2.8) | <0.001 |
| 0–2 | 42 (30) | 55 (46) | ||
| SOFA0[median (IQR)] | 9 (7) | 7 (6) | 1.1 (1.05–1.15) | <0.001 |
| SOFA1[median (IQR)] | 12 (6) | 8 (6) | 1.16 (1.1–1.2) | <0.001 |
| Creatinineb(mg/dL) [median (IQR)] | 1.1 (0.6) | 1 (0.4) | 1.12 (0.97–1.28) | |
| Creatinine0(mg/dL) [median (IQR)] | 2.2 (1.94) | 1.97 (2.7) | 0.98 (0.9–1.06) | |
| Creatinine1(mg/dL) [median (IQR)] | 2.9 (2.4) | 2.8 (2.9) | 0.96 (0.9–1.04) | |
| Oliguria0[n (per cent)] | 131 (93) | 96 (80) | 2.6 (1.4–6.3) | 0.006 |
| Diuresis6hTRR(mL) [median (IQR)] | 75 (135) | 100 (160) | 0.998 (0.996–1) | 0.045 |
| Time from ICU to RRT (days) [median (IQR)] | 1 (7) | 1 (5) | 1.03 (1.01–1.04) | 0.003 |
| Time from hospital to RRT (days) [median (IQR)] | 4 (14) | 2 (8) | 1.02 (1.01–1.03) | <0.001 |
| Duration of the CRRT (days) [median (IQR)] | 6 (7) | 5 (5) | 0.99 (0.97–1.02) | NS |
| Dose of CRRT (mL/kg/h) [median (IQR)] | 35 (10) | 33 (8.5) | 0.99 (0.98–1.01) | NS |
| Dose of CRRT >35mL/kg/h [n (per cent)] | 41 (29) | 34 (28) | 1.06 (0.7–1.6) | NS |
| Pre-ICU days [median (IQR)] | 0 (5) | 0 (2) | 1.01 (1 –1.025) | NS |
| IHD [n (per cent)] | 25 (18) | 44 (37) | 0.4 (0.24–0.65) | <0.001 |
| Duration of IHD (days) [median (IQR)] | 5 (10) | 5 (9) | 0.99 (0.97–1.03) | NS |
| Vascular access [n (per cent)] | ||||
| Femoral | 126 (89) | 94 (78) | ||
| Jugular vs femoral | 10 (7) | 24 (20) | 0.3 (0.2–0.7) | 0.007 |
| Subclavian vs femoral | 5 (3.5) | 2 (1.6) | 1.8 (0.7–4.3) | NS |
Creatinine0: plasma creatinine levels at ICU admission; Creatinine1: plasma creatinine levels at the initiation of the RRT; Creatinineb: prior plasma creatinine levels; Pre-ICU days: days of hospital stay prior to ICU admission; Diuresis6hTRR: 6h urine volume collection prior to the initiation of the RRT; Dose of CRRT: treatment doses of CRRT (effluent dose); Liaño ISI: Liaño Individual Severity Index; NS: non-significant (p>0.05); SOFA-CV: cardiovascular SOFA; SOFA0: SOFA severity score determined at ICU admission; SOFA1: SOFA severity score at the initiation of the RRT; Time to RRT: time elapsed from the ICU admission date to the moment of initiation of the RRT; RRT: renal replacement therapy; CRRT: continuous renal replacement therapy.
Multivariate analysis of mortality at 90 days.
| RR (95 per cent CI) | p | |
|---|---|---|
| SOFA1 (determined at the beginning of the therapy) | 1.131 (1.053–1.214) | <0.001 |
| Time elapsed from ICu admission to the initiation of the RRT (days) | 1.016 (1.006–1.026) | 0.002 |
| Type of medical context in relation to the surgical context | 0.617 (0.400–0.952) | 0.03 |
Cox proportional-hazards regression model adjusted to age, type of center, context, etiology, oliguria, ICU admission and diuresis 6h before the initiation of the therapy, to the SOFA severity score and the initiation of the therapy, to the SOFA-CV at admission and the Liaño ISI, to the time elapsed from ICU admission to the initiation of the RRT, and also adjusted to the time elapsed from ICU admission to the initiation of the RRT.
We showed the results of one multicenter study conducted in Catalonia on the use of RRT in ICUs that confirm that the main reason for administering this therapy is oliguria, that the most widely used vascular approach is through the femoral vein, that the CRRT is the most widely used therapy and that the pre-HDF is the most widely used modality with initial titrated doses of 35mL/kg/h. The type of patient treated with CRRT is that of a 66 year-old male whose mortality will reach levels of 50 per cent after 3 months, which is related to how serious the condition is and with late initiation of RRT. Eighty-five per cent of survivors will recover their RF at hospital discharge.
This work was planned as one multicenter, epidemiological study in order to have an in-depth knowledge of the actual management of RRT in Catalonia, after completing one preliminary study conducted in 6 different centers.13 The actual study included 21 ICUs in Catalonia and 261 patients.
On the other hand, after completing the study recruitment period, in Summer of 2012, the KDIGO14 guidelines (Kidney Disease: Improving Global Outcomes. Clinical practice guideline for the evaluation and management of acute kidney injury) were published with specific recommendations for the management of acute kidney injuries. Then, after analysing the study data, we decided that we wanted to know the degree of compliance with the KDIGO recommendations yet despite the fact that our study had been conducted before the publications of these guidelines; also we wanted to compare our data to the data from the BEST,2 ATN,4 and RENAL studies.5
Compared to BEST2 study where most patients were treated with CVVHF (53 per cent) and a 20mL/kg/h dose, in our setting patients were cleansed with pre-HDF (87 per cent) and the first day the doses prescribed were 35mL/kg/h. After the publication of the KDIGO guidelines14 it is recommended to administer doses between 20 and 25mL/kg/h, yet to be able to administer such doses, usually it is necessary to titrate higher doses. It could be said that in the absence of regional anticoagulation with citrate, as it was the case in our study, the dose titrated at the beginning probably follows the recommendations stated by the KDIGO guidelines. However, we found that 28 per cent of the patients had been treated with high volumes–not recommended by the KDIGO guidelines because no beneficial effects on survival15–17 have been reported and because high doses can increase the rate of RTT4,5,17 adverse events. On the other hand, former studies18 seem to have confirmed better prognoses with the administration of high volumes. In our case, patients treated with high flows were in more serious condition but their mortality was similar to that of other patients. So it is possible than in selected patients, when the moment is right and for a limited period of time, high volumes can be helpful but only in expert hands and to minimize dialytrauma.19
Another significant aspect is femoral location as the most commonly used vascular approach; however, the jugular vein approach is used 12 per cent of patients only. This contradicts the recommendations stated by the KDIGO14 guidelines where the right jugular vein approach is recommended in the first place. However, more recently, recommendations suggest using20 both the femoral vascular approach and the jugular vein approach equally as the two access routes of choice for RTTs, all conditions being equal.
The time elapsed between admission and the initiation of the RRT is also controversial mainly because no studies specifically designed to find this out have been conducted.21,22 The meta-analyses have not been conclusive though it seemed that in the group of surgical patients –where the moment of aggression is perfectly known, the precocity in the initiation of the RRT seemed to be beneficial for prognosis purposes.23,24 Likewise, the effect that a delayed RRT initiation had on mortality was reported in both the RENAL5 and ATN4 studies in such a way that, in the RENAL study, early initiations were accompanied by better prognoses (44.7 per cent mortality at 90 days), while in the ATN, later initiations were followed by higher mortality rates (52.5 per cent at 60 days), with similar conditions of severity. In our case, late initiations predicted worse prognoses. This is of vital importance since the moment of initiation of the therapy is an aspect that the clinician can act upon and, therefore, only depends on our clinical practice.
The mortality associated with RRT is still high. And yet despite the fact that the BEST study published in 20072 showed that hospital mortality had dropped from 63.8 to 48.3 per cent in our registry, the fact that one out of every two patients on CRRT will end up dying seems unacceptable. Also the latest clinical trials confirm very somber prognoses. The ATN4 study shows an average CV-SOFA of 2.3±1.7 and 52.5 per cent mortality at 60 days; the RENAL5 study shows an average CV-SOFA of 2.8±1.5 and 44.7 per cent mortality at 90 days; and our registry shows an average CV-SOFA of 2.6±1.7 and 54.04 per cent mortality at 90 days. Our registry also provides data on patients’ comorbidities,10 including the Liaño11 ISI severity score that better adjusts the prognosis of patients with acute renal failure. This is how we could confirm that there were patients with a significant comorbidity who were in very serious condition at ICU admission. And yet despite the fact that the other studies mentioned did not implement the ISI, they took other severity scores into consideration, and all studies confirmed that mortality is closely related to the severity of the patient's condition.25–27 On the other hand, other studies have also confirmed that mortality is not associated with any other aspects of RRTs (technical modality, effluent dose, etc.).2
The registry found that up to 86.21 per cent of patients had oliguria at ICU admission. Also it was reported that yet despite the patients’ resuscitation carried out in every center, 82.75 per cent of the patients remained oliguric when the RRT was initiated. Therefore, it is not surprising that the main reason for patients to be titrated with RTT was oliguria. Nevertheless, the RENAL5 study confirmed that 60 per cent of its patients were oliguric. At this point, we can make two considerations: on the one hand, it is well known that transient oliguria is a common event in ICUs, but not necessarily associated with acute renal failure.28 On the other hand, it is also well known that persistent oliguria of over 12-h duration is associated with worse prognosis,29 which means that the moment of initiation of the RRT should be adequate for every patient in order to avoid having to rush the initiation of the RRT in prerenal patients or insufficiently resuscitated patients, or in order to avoid delaying therapy in patients with very serious condition who may benefit from early initiations of therapy.
Recently a couple of clinical trials have been designed aimed at assessing mortality in relation to the initiation of RRT in critical patients with acute renal failure who due to their special relevance are discussed now. On the one hand, the French study AKIKI30 was analyzed and its results have shown that an earlier initiation of the therapy is not followed by better prognosis (49.7 vs 48.5 per cent mortality at 60 days). However, this French multicenter study has some remarkable peculiarities: patients were randomized once they had been categorized as stage 3 according to the KDIGO guidelines14–moment for the early group to initiate the RRT as soon as possible and for the late group to wait for another 72h. In this study, the strategy used for the resuscitation of patients, the study protocol, the technique used, or the analysis of mortality has not been described. The study authors claim that 55 per cent of the patients were treated with IHD and only 30 per cent of the patients received CRRT. The late group received many more diuretics and only 40 per cent of the patients ended up needing RRT. Patients who did not received RRT had a SOFA score of 10 and mortality rate was 37 per cent; patients who received early RRT had a SOFA score of 11 and 48.5 per cent died, and patients who received late RRT had a SOFA score of 12 and 61.8 per cent died. However, the SAPS III was not significantly different among the three (3) groups. The predictors of the need to administer RRT (analyzed in the late group) were urea, pH and the SOFA score. That is, patients with a more serious condition ended up needing RRT, but it is possible that initiating RRT late was followed by a higher mortality rate. Also, the patients from the late group had more hemorrhagic complications (4 vs 0.3 per cent), in such a way that the only hemorrhagic complication in the early group was due to a bleeding arterial puncture. However, in the late group there were 6 abdominal hemorrhages, 3 cases of hemothorax, 1 hemoptisis, 1 polytrauma bleeding, and 2 bleedings secondary to catheter punctures.
On the other hand, we have the German study ELAIN,31 that has published different results than the AKIKI30 study. These authors found that an early initiation (administering the CRRT during the first 8h of a KDIGO stage 2), after a mean 6h randomization was associated with a 39.3 per cent mortality rate compared to a 54.7 per cent mortality rate after later initiations of the therapy (during the first 12h of a KDIGO stage 3), after a mean 26h randomization. In this study, in addition to the KDIGO criterion, the determination of plasma neutrophil gelatinase-associated lipocalin >150ng/mL was also a requirement when ruling out any prerenal cases. Patients received doses of 26mL/kg/h of pre-HDF in predilution at a ratio of 1:1 under regional anticoagulation with citrate. In addition to better survival at 90 days, early initiations of the therapy were associated with shorter courses of CRRT (9 vs 35 days; p=0.04), mechanical ventilation (126 vs 181h; p=0.002) and hospital stays (51 vs 82 days; p<0.001). No differences could be seen in the need for dialysis at 90 days (13 vs 15 per cent). No significant hemorrhagic complications were reported. Likewise, the analysis of inflammatory mediators confirmed a significant drop in the concentrations of cytokines in the early group compared to the late group after 24h of randomization that the authors associated with a better survival rate in these patients. However, this study has some limitations: it was conducted in a single center only, most patients were surgical patients and, yet despite the fact that only 35 per cent were septic patients, the average SOFA score was 16–significantly higher than the SOFA score from the studies published and discussed before.
Given the importance of these last two (2) studies published about the best time to initiate RRT and its relation to mortality and since our results also establish a correlation between the initiation of the RRT and survival, in a-posteriori analysis we were able to study if the initiation of the RRT in a KDIGO stage 2 or 3 would modify the prognosis of patients, but we did not found any significant differences, although we found a correlation between a worse KDIGO stage and a higher mortality rate. Another remarkable aspect is the “creatinine” component in the KDIGO scale that is more relevant for prognosis in cases of non-oliguric acute renal failure, but not as much in oliguric patients. However, oliguria both at admission and at the initiation of the RRT has a strong correlation with mortality. Results are shown in additional material as supplementary material.
However, the moment of RRT initiation should probably be individualized according to the needs of each patient. It will more certainly depend on the patient's severity, thus considering an earlier initiation of RRT in unstable patients after optimal resuscitation with volume that rules out any prerenal states, but it will also depend on the reversibility of the patient's acute renal failure that may be accessed through the use of renal biomarkers,32 the furosemide stress test,33 or even be taken into consideration further in time in stable patients.
In spite of all this, we think it is imperative to do more research with well designed, multicenter clinical trials powered to assess the effect that the moment of RRT initiation has on mortality in our setting, in relation to the type of patients we have and the type of therapies we use.
Finally, we found impairment of prior RF in 35 per cent of the patients–similar to other studies.1 Eighty-five per cent of RF was recovered at hospital discharge–consistent with the numbers of the BEST and FRAMI studies,2,9 and was associated with more serious impairment of RF at hospital admission and with comorbidity–consistent with medical literature.2,34–37 Factors, all of them, that cannot be modified beforehand. So older patients with RF impairment and other comorbidities should be closely monitored and, if possible, renal aggressions should be avoided. Similarly, it seems obvious that the RF of patients treated with RRT should be monitored, and follow-up interconsultations by the nephrology unit after ICU discharge should be protocolized.
Limitations of the studyThis study has some limitations. In the first place, even though the registry results suggest that the precocity in the initiation of RRT is an independent factor in the survival of these patients, these results come from an observational, epidemiological study with no interventions, and this is why any conclusions drawn should be taken with caution. So the main limitation of the conclusions of this study is that we cannot confirm the existence of an undisputed relation between the precocity in the use of therapy and survival. Secondly, another limitation of this type of epidemiological studies is the inability to control any potentially confounding variables in such a way that the association found between two (2) variables may be due to a third one. That is, it may be possible for one RRT to have been administered early in a prerenal situation with good clinical outcome, or delayed in a critical patient while waiting to see the disease progression in such a patient. In both cases, the prognostic result would depend on this third variable and might confound its relationship with the initiation of the RRT. On the other hand, however, it is also possible that the early initiation of the therapy improves survival. This is something that cannot be affirmed or denied. Finally, the study design determined that recruitment should take place for three months during the spring season, which may not be appropriate or representative of the management of CRRT or the type of patients not treated in such season.
ConclusionsOne multicenter, epidemiological study analysing the actual management of CRRT was conducted in Catalonia, and confirmed that mostly it is consistent with the recommendation of the actual clinical practice. Most patients treated with CRRT are oliguric at ICU admission and remain oliguric 6h after the initiation of the therapy, which is the main reason why CRRTs are indicated. The mortality associated with CRRTs is above 50 per cent at 3 months and it is associated with how serious the patient's condition is and how late the RRT was initiated. The RF recovery of survivors was around 85 per cent.
FinancingThis paper has not received any financial support.
Authors/collaborationsTMT had the idea to conduct this study, collaborated in its design, spread the word for the recruitment period for participating centers, solved the doubts from other researchers on data collection, collected data from his center, reviewed the global database, conducted the statistical analysis and wrote the manuscript; JS contributed to the study design, review the database and proofread the manuscript: EP was one of the people who had the idea to conduct this study, contributed to the study design, spread the word for the recruitment period for participating centers, and solved the doubts from other researchers on data collection; JF was one of the people who had the idea to conduct this study and contributed to the study design; MJLL contributed to his center data collection and reviewed its database; JR conducted the statistical analysis: AN collected data for his center and reviewed the database; PO collected data for his center and reviewed the database; LLS collected data for his center and reviewed the database; FJGM collected data for his center and reviewed the database; CR collected data for his center and reviewed the database, and ARTMT was one of the people who had the idea to conduct this study, contributed to the study design, solved the doubts from other researchers on data collection, collected data for his center, reviewed the global database and proofread the manuscript.
Conflicts of interestsWe the authors declare that while conducting this paper there were no conflicts of interests linked whatsoever.
We wish to thank all those people who have given us their help, and collaboration to be able to conduct this paper, both in the selection of patients, data collection and review, and in the follow-up of patients and other necessary chores; all of them are members of the REGISTRA Collaborative Group: without their invaluable contributions we would not have been able to build such a representative registry of patients.
Hospital Arnau de Vilanova de Lérida: Lluís Servià, Joana Domingo, Marisa Martín; Hospital de Bellvitge: Miguel Hueso; Hospital Clínic: José M. Nicolás, Pedro Castro, Néstor Rodríguez, Alejandra Hernández; Hospital General de Catalunya: Teresa Doñate, Maria L. Martínez; Hospital General de L’Hospitalet: Raúl Lafuente; Hospital General de Vic: Rosa M. Catalan, Eugenia Castellote; Hospital Germans Trias i Pujol de Badalona: José M. Manciño, Loreto Fernández; Hospital de Granollers: Judith Xirgu, Diana Colon, Silvia Garcia; Hospital Joan XXIII de Tarragona: Federico Esteban, Carmen Gilavert, Marcos Ibañez, Carmen Peralta, Olga Moreno; Hospital Josep Trueta de Gerona: Josep M. Sirvent, Patricia Ortiz, Anna Baró, Anna Garia-Fragua, Martí Vallés, Cristina Martínez; Hospital de Manresa: Silvia Cano, Núria Garra; Hospital del Mar: Yolanda Díaz; Eva Rodríguez, Juan Rodríguez, Igini Cao; Hospital de Mataró: Manel Solsona; Hospital Moisés Broggi: Miguel Rodríguez, Pilar Ruiz, Oana Rap; Hospital Mútua de Terrassa: Joan Llibre, Maria A. Martínez, Francisco J. González de Molina; Hospital de Palamós: Rosa García; Hospital Parc Taulí de Sabadell: Loreley Betancourt, Manuel García, Gemma Gomà, Gisela Gili. Antonio Artigas; Hospital del Sagrat Cor: Mercedes Ibarz, Antoni Pelegrí; Hospital Sant Joan de Reus: Conxita Rovira; Hospital de Sant Pau: Hernán Aguirre-Bermeo, Mireia Cuartero, Montserrat Vila; Hospital de Terrassa: Maria Alvarez, Alfons Arizmendi, Vanesa Arauzo, Ana Saurina; Hospital Vall d’Hebrón: Raquel Albertos, Lluís Llopart, Marcos Pérez, Elías Jatem, Natalia Ramos; Hospital Verge de la Cinta de Tortosa: Marcos Ibáñez, Juan P. Castañeda, José Luna, P. Angelet; Fundació Puigvert: Enric Andrés, Juan M. Díaz.
See list of centres and participants in Annex.
Please cite this article as: Tomasa Irriguible TM, Sabater Riera J, Poch López de Briñas E, Fort Ros J, Lloret Cora MJ, Roca Antònio J, et al. Manejo actual de las terapias continuas de reemplazo renal: Estudio epidemiológico multicéntrico. Med Intensiva. 2017;41:216–226.